Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Gastroesophageal reflux is a frequently seen condition in infants and children. In fact, in premature and young infants, it can be normal until the lower esophageal sphincter (LES) matures. With maturation of the LES, these symptoms often resolve spontaneously. In other infants and children, medical management may be effective in relieving symptoms but is not likely to yield long-term results after several years of age. Laparoscopic fundoplication can provide a very effective treatment for the long-term cure of this condition and its associated complications.
Infants with gastroesophageal reflux who are feeding well and growing nicely do not usually require operative intervention, as the condition frequently resolves spontaneously with medical management in this very young age group. Indications for surgical intervention for gastroesophageal reflux disease in young infants includes acute life-threatening events secondary to aspiration, failure to thrive with associated weight loss, and sometimes in combination with the need for placement of a gastrostomy in neurologically impaired infants. In older children, indications for fundoplication include failure of medical therapy, esophagitis, and reactive airway disease secondary to gastroesophageal reflux. Also included in this older group are the neurologically impaired children who cannot protect their airway and require placement of a gastrostomy for enteral alimentation.
The diagnostic evaluation for infants and children with gastroesophageal reflux has changed over the past 20 years. Twenty years ago, a pH study, an upper gastrointestinal (GI) contrast study, endoscopy with or without biopsy, and a gastric emptying study were utilized in most patients. Because none of these studies are close to 100% sensitive, many surgeons in the United States have transitioned to evaluating the patient for operation based more on the clinical symptomatology as opposed to diagnostic studies. In Europe, however, a 24-hour pH study/impedance study is performed routinely. The impedance study allows evaluation for alkaline reflux, which has been shown to occur in up to 40% of children with reflux. Additionally, the upper GI contrast study is not very sensitive for evaluating reflux, although it can be helpful in determining if the patient has distal obstruction, such as a gastric outlet obstruction or malrotation. Endoscopy usually requires general anesthesia in infants and children and, for this reason, is not used extensively. Finally, in the United States, gastric emptying studies are felt not to be helpful at all as many patients have been found to have improved gastric emptying following fundoplication. Therefore, knowing whether or not the patient has preoperative gastric emptying is probably not important because the gastric emptying will likely improve following fundoplication. In Europe, in contrast, gastric emptying studies are deemed to be important, as gastric emptying disorders are considered a contraindication for fundoplication.
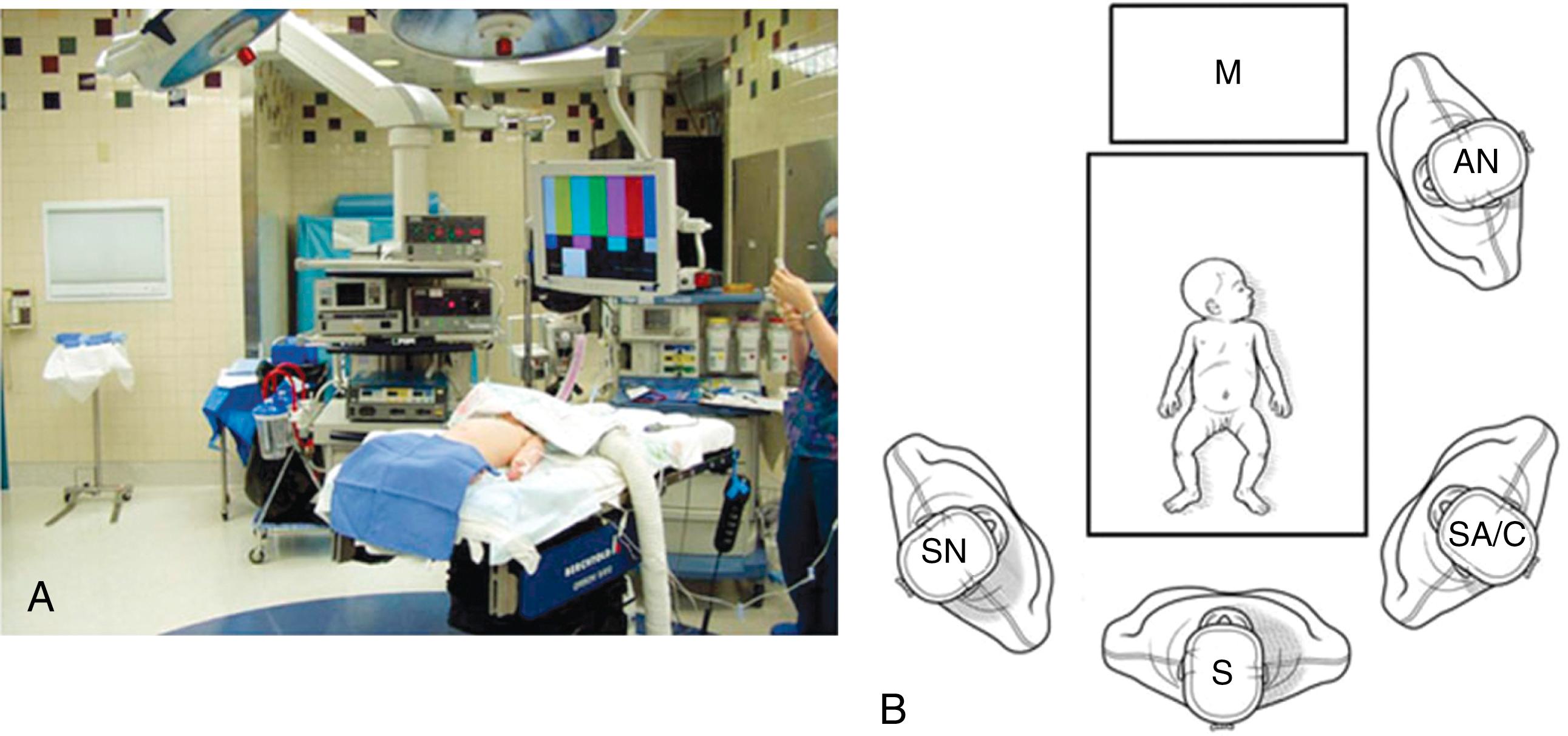
The patient is placed supine on the operating room table, and general endotracheal anesthesia is administered. Infants and young children are positioned at the foot of the bed in a frog-leg position ( Fig. 2-1A ). The foot of the bed is dropped so that the surgeon and assistant can stand at the end of the bed ( Fig. 2-1B ). For older children, the legs are placed in stirrups. An orogastric tube is introduced to decompress the stomach, but a urinary catheter is not routinely inserted. If a gastrostomy is needed, this site is marked prior to insufflation. This site will also be one of the working incisions for the laparoscopic fundoplication. A single monitor is positioned over and slightly cephalad to the patient’s head.
After the preparation and draping, a vertical 5-mm incision is made in the center of the umbilicus. We prefer a cutdown approach (as opposed to using a Veress needle) so the dissection is continued through the umbilical fascia with cautery. An umbilical hernia is often present, especially in infants and young children, providing easy access to the peritoneal cavity. A 5-mm cannula with a blunt-tipped trocar is then introduced through the umbilical fascial and peritoneal incision, and CO 2 insufflation is initiated with a flow rate of 3 to 5 L/min and a maximal pressure of 10 to 12 mm Hg. A 5-mm, 45-degree angled telescope is introduced through the umbilical cannula and diagnostic laparoscopy is performed.
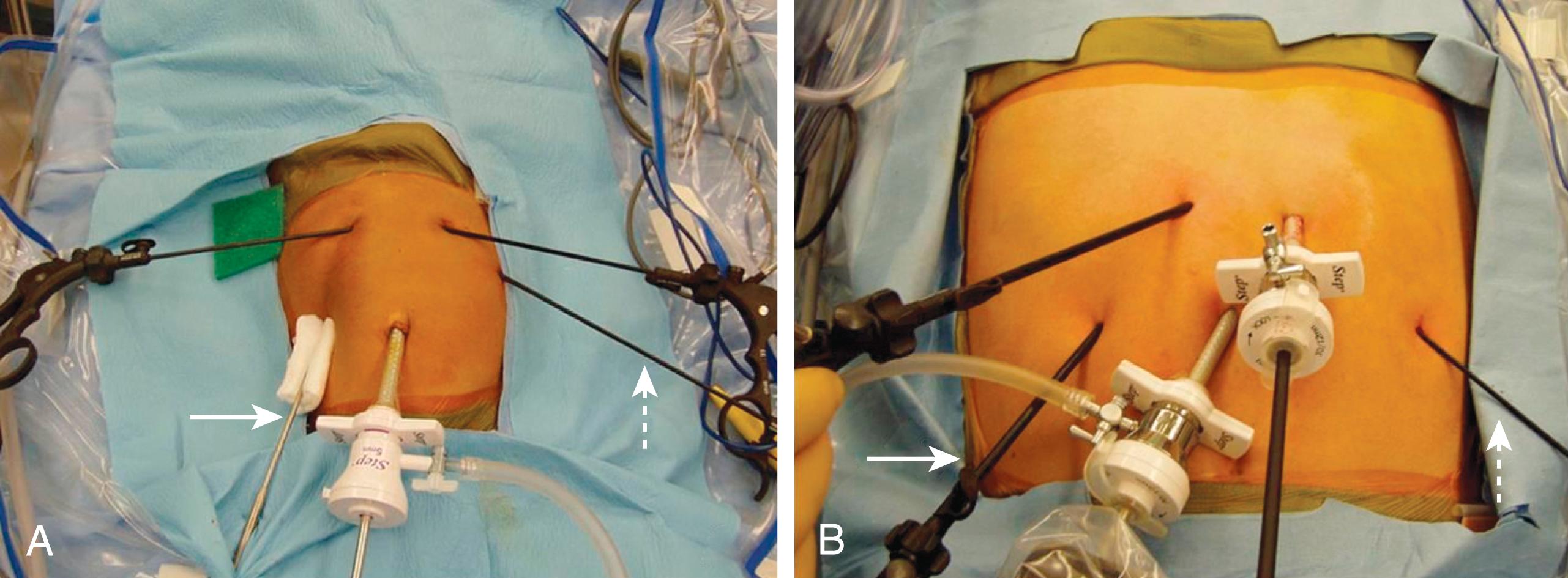
After a brief diagnostic laparoscopy, four accessory stab incisions are made (see Chapter 1 ). The first incision is created in the patient’s right subcostal region, which is the site for introduction of the liver retractor. We now utilize the Nathansan liver retractor (Mediflex Surgical Products, Islandia, NY) and secure it using the Thompson instrument holder (Thompson Surgical Instruments, Traverse City, MI). The two main working sites for the operation are to the right and left of the midline in the upper epigastrium. In the left hand, the surgeon uses an atraumatic grasper that has been inserted through the stab incision in the patient’s right epigastrium. The incision in the patient’s left epigastrium is the surgeon’s primary working site. Through this incision, dissecting instruments and the needle holder (and sealing device, if used) are introduced. The final stab incision is in the patient’s left lateral subcostal region, through which an atraumatic forceps is introduced for retraction purposes by the assistant surgeon ( Fig. 2-2 ).
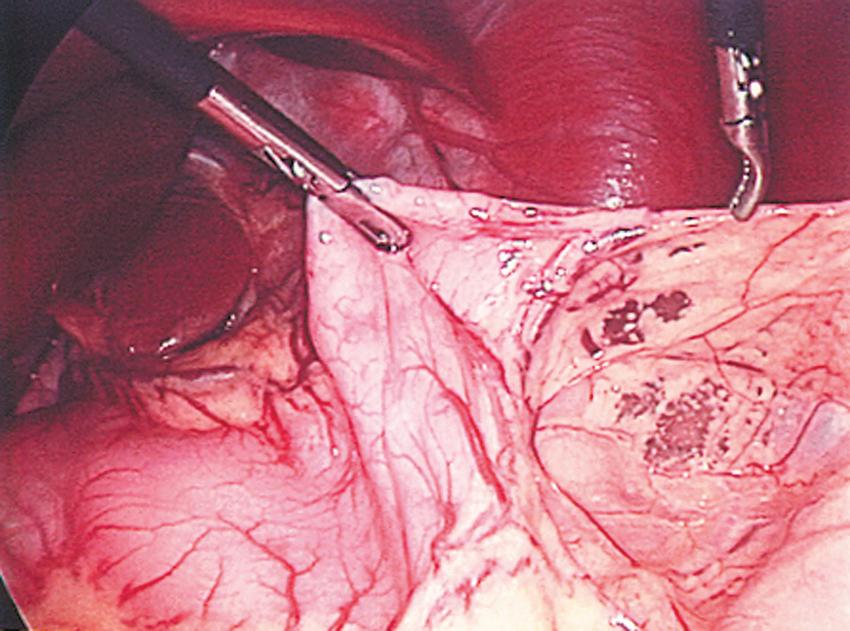
The initial operative step is to ligate and divide the short gastric vessels in order to mobilize the gastric fundus to allow a tension-free fundoplication. This dissection starts at a point one-third the way down the greater curvature of the stomach ( Fig. 2-3 ). In infants and children up to the age of 5 years, this ligation and division is performed with the Maryland dissecting instrument connected to cautery. For children older than 5 years, a 3-mm sealing device (Bolder Surgical, Louisville, CO) is preferred for this purpose. (In these older children, instead of a stab incision in the left epigastrium, a 3- or 5-mm cannula can be used.) Dissection along the greater curvature is carried to the esophageal hiatus, where the hiatus is carefully inspected. We now perform as little dissection as possible to help prevent transmigration of the fundoplication wrap through an enlarged esophageal hiatus ( Fig. 2-4 ). We try to keep the phrenoesophageal membrane intact for this reason. The retroesophageal space is then opened from the patient’s left side (see Fig. 2-4 ).
After creation of an adequate retroesophageal window, attention is turned to the right side of the esophagus for further mobilization if needed. With minimal esophageal dissection and mobilization, there may not be a significant crural deficit that needs repair. However, if needed, the crura are approximated posteriorly with a single 2-0 suture on an RB needle in infants, or with a 0-silk on an SH needle in adolescents. The length of this suture is approximately 11 cm. The suture is tied intracorporeally. Rarely, because of the size of the hiatus, a second suture is needed. So as to not angulate the esophagus too much posteriorly, this second suture is usually placed anterior to the esophagus and incorporates a portion of the anterior esophageal wall with the crural closure. Again, 2-0 or 0-silk suture is used for this purpose.
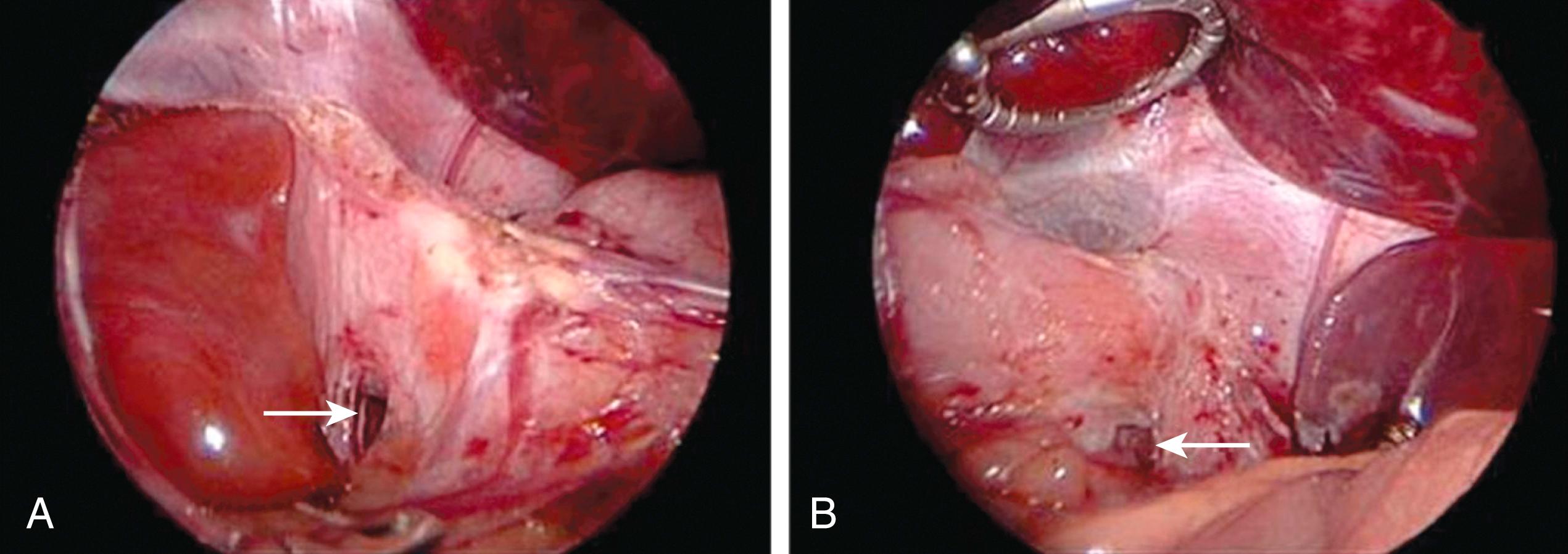
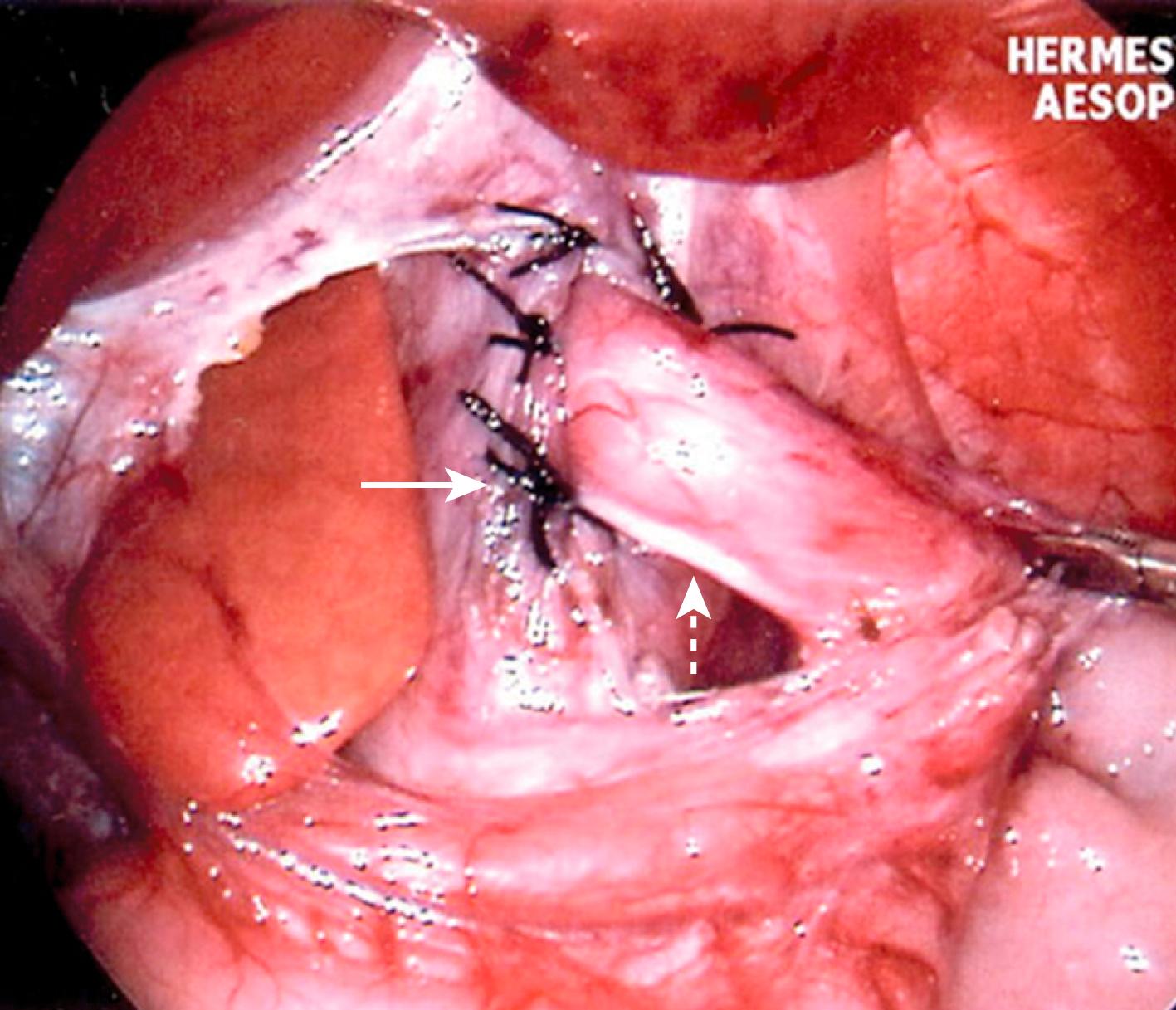
We used to secure the esophagus to the crura circumferentially with interrupted 3-0 silk sutures on an RB-1 needle. These sutures were placed at the 7-, 11-, 1-, and 5-o’clock positions and were tied intracorporeally as well ( Fig. 2-5 ). The purpose of these esophagocrural sutures was twofold: first, to secure the esophagus in an intra-abdominal position to reduce the incidence of gastroesophageal reflux, and second, to obliterate the space between the esophagus and the crura, which, hopefully, would prevent transmigration of the fundoplication wrap into the lower mediastinum. However, in a recent prospective randomized trial, we found these sutures were not necessary if there was minimal esophageal dissection and mobilization (see Fig. 2-4 ).
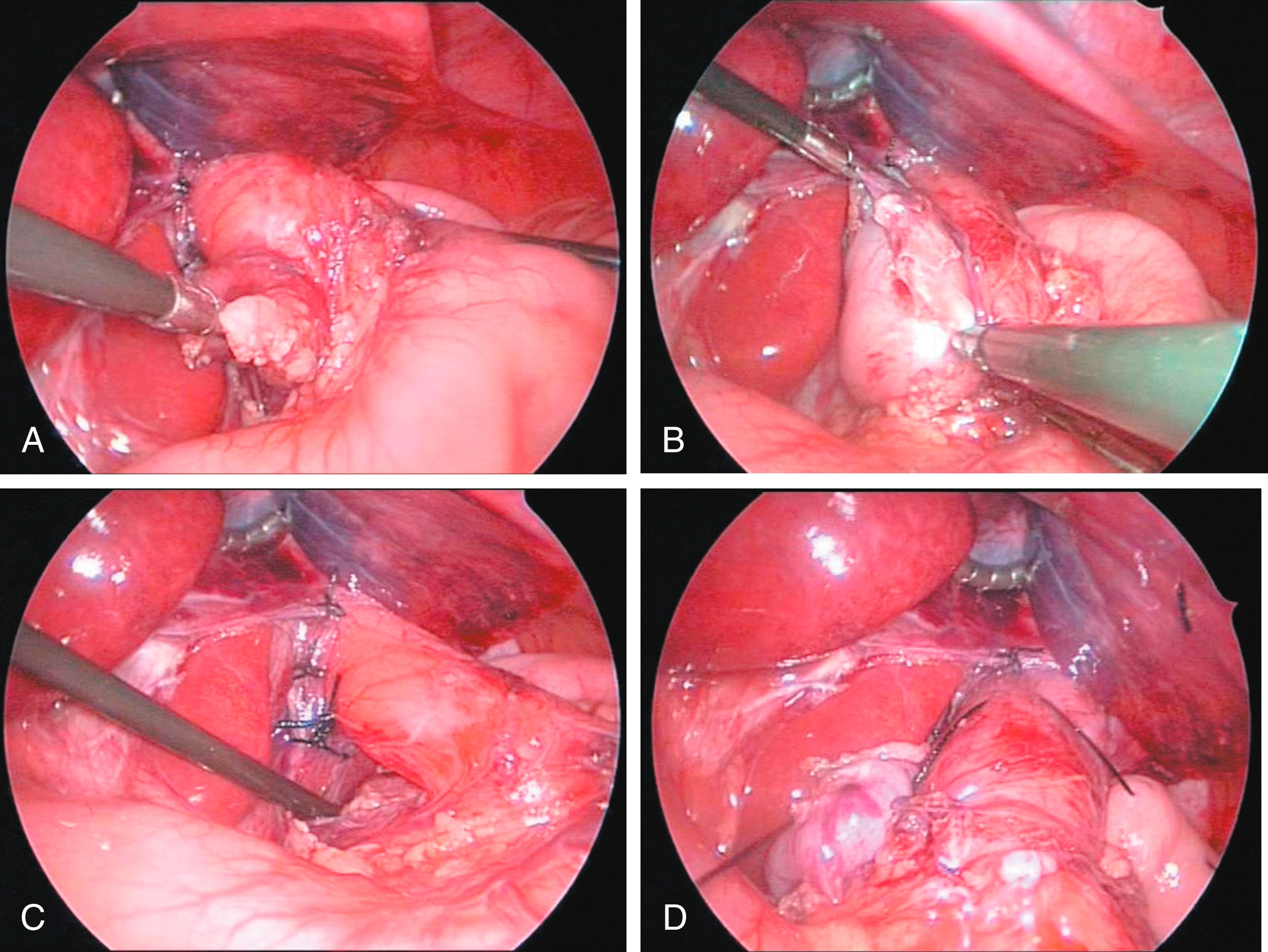
At this point, attention is turned toward the fundoplication. The telescope is reoriented so that it is easy to visualize the retroesophageal space from the patient’s right side of the esophagus. The gastric fundus is grasped with the atraumatic grasping forceps in the surgeon’s left hand and delivered through the retroesophageal space ( Fig. 2-6A ). It is then oriented appropriately to ensure that there is no twisting of the fundus as it is brought through the retroesophageal space (see Fig. 2-6B ). The fundus is then returned through the retroesophageal space, and a bougie is introduced orally by the anesthesiologist (see Fig. 2-6C ). In infants and young children, the appropriate size of the bougie depends on the patient’s weight ( Table 2-1 ). A great deal of care must be taken to ensure that the bougie is carefully guided into the stomach and does not inadvertently perforate the esophagus or stomach.
| Weight (kg) | Bougie Size (Fr) |
|---|---|
| 2.5-4.0 | 20-24 |
| 4.0-5.5 | 24-28 |
| 5.5-7.0 | 28-32 |
| 7.0-.5 | 32-34 |
| 8.5-10.0 | 34-36 |
| 10.0-15.0 | 36-40 |
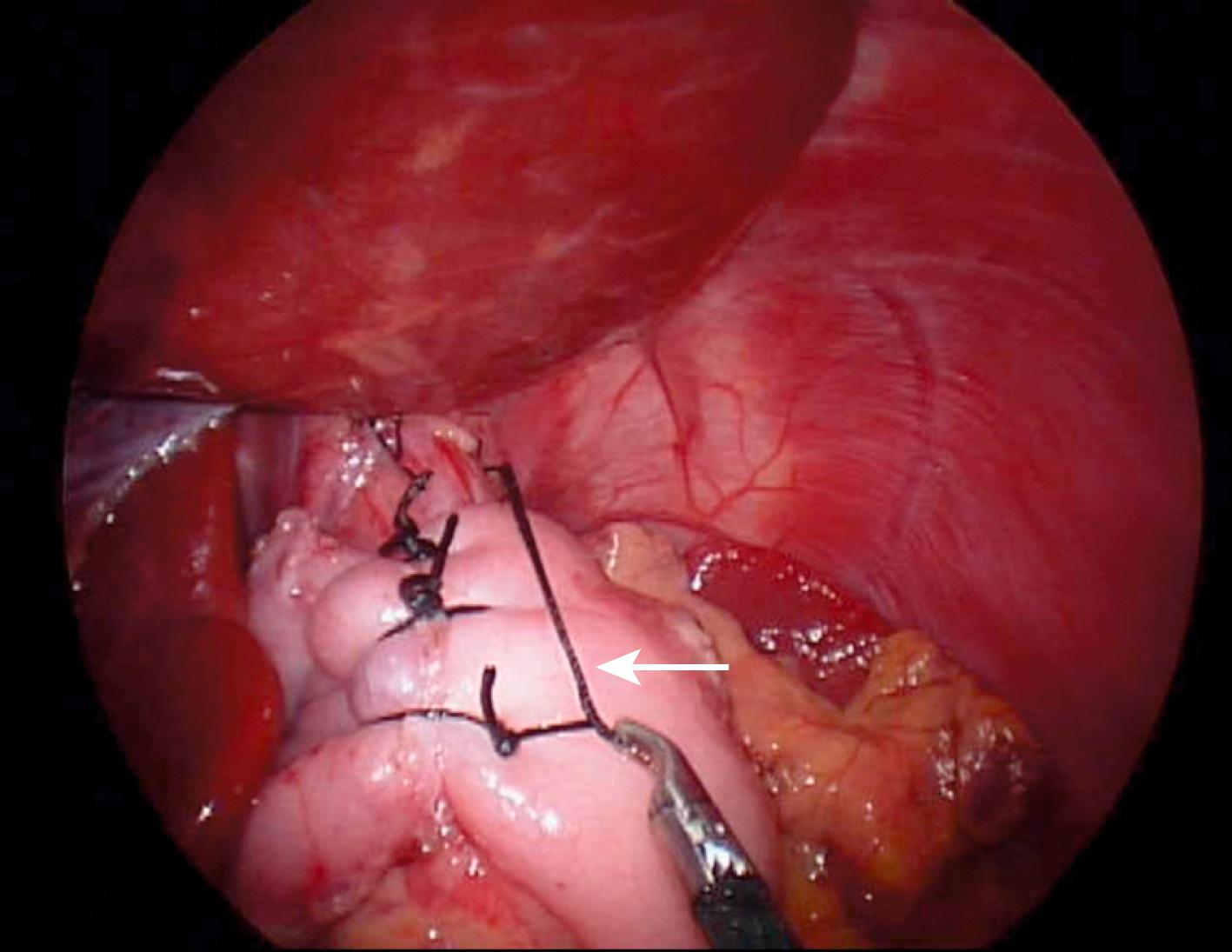
Once the bougie has been introduced into the stomach, the fundus is brought back through the retroesophageal space and sewn to itself in a standard Nissen fundoplication technique. Silk sutures (2-0) on an RB-1 needle in infants and young children and 0-silk sutures on an SH needle in adolescents are used to create the fundoplication. Usually, three sutures are placed, with the most cephalad suture also incorporating the anterior wall of the esophagus (see Fig. 2-6D ). The length of the first silk suture is 12 cm, and the remaining ones are 8 to 10 cm. The posterior and anterior vagus nerves are both incorporated within the wrap. The fundoplication length is always measured and should approximate 2 cm in infants and young children and 2.5 cm in adolescents ( Fig. 2-7 ). At this point, the bougie is removed, the instruments are withdrawn, and the stab incisions are approximated with Steri-Strips (3M Corp, St. Paul, MN). The umbilical fascia is closed with absorbable suture and the umbilical skin approximated with 5-0 plain catgut suture. Sterile dressings are then applied and anesthesia is terminated.
The patients are admitted after the operation and allowed to drink clear liquids or formula approximately 4 to 6 hours after the operation at a low volume and low concentration. The volume and concentration can be advanced over 24 hours. Over 80% of our patients are ready for discharge the day after the operation, and the remaining 20% are discharged on the second postoperative morning. Very few patients admitted the day of the operation have required hospitalization longer than 48 hours.
In children older than 2 years, it is extremely important to institute a mechanical soft diet for 3 weeks, as there is swelling that occurs at the level of the fundoplication. This is especially true for adolescents, in whom moderate bites of meat, toast, or the like can become lodged at the fundoplication wrap early in the postoperative course.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here