Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Keratotic lesions of the plantar skin result from friction, pressure, shearing, or a combination of these mechanisms. They are often related to underlying bony prominences, muscle imbalance leading to atypical foot posture, or improper footwear. These must be distinguished from the intrinsic disorders of the skin, such as verrucae and dermatosis, especially tinea infestations (see Chapter 16 ). Keratotic lesions are related to both the pressure applied and the amount of time the pressure resides unabated.
Localization of pressure along the plantar aspect of the foot reflects the relative length of time that the center of pressure dwells beneath the metatarsal heads during normal walking (see Chapter 1 ). After heel strike, the center of pressure moves rapidly to the metatarsal head area during the second rocker, where it dwells for more than 50% of the stance phase, after which it moves toward the toes ( Fig. 13-1 ). Because of this extended period of weight bearing in the metatarsal area, abnormal alignment of the forefoot, either localized or generalized, compounds the pressure-time dynamic leading to the formation of a keratotic lesion.
A broad differential diagnosis must be considered in the evaluation of the patient presenting with a plantar callus ( Box 13-1 ). The diagnosis of hyperkeratosis is usually not difficult to make, but at times the underlying diagnosis may not be clear. Maintaining a broad differential helps avoid treating the symptom without solving the underlying problem.
Osseous Causes
Prominent fibular condyle metatarsal head
Long metatarsal
Morton foot
Hypermobile first ray
Posttraumatic effects
Abnormal foot posture (varus or valgus)
Systemic Diseases
Rheumatoid arthritis
Psoriatic arthritis
Dermatologic Lesions
Wart
Seed corn
Hyperkeratotic skin
Keratosis palmoplantaris nummularis
Epithelioma cuniculatum (verrucous carcinoma)
Soft Tissue Causes
Atrophy of plantar fat pad
Crush injury sequelae
Plantar scar secondary to trauma
Neurogenic Causes
Upper motor neuron lesions (e.g., hyperactivity of peroneus longus)
Lower motor neuron lesions (e.g., neuropathy leading to claw-toes)
Mechanical Causes
Subluxated or dislocated metatarsophalangeal joint
Hallux valgus deformity resulting in transfer lesion
Iatrogenic Causes
Secondary to metatarsal surgery (e.g., plantar flexion)
Transfer lesion
Hallux valgus surgery (e.g., shortening or dorsiflexion of metatarsal)
The predominant pattern of the metatarsal cascade demonstrates that the first metatarsal is shorter than the second approximately 60% of the time. The mobility of the first metatarsocuneiform (MTC) joint or the first metatarsophalangeal (MTP) joint determines the degree of weight bearing of the first ray. The plantar aponeurosis mechanism brings about plantar flexion of the first metatarsal during the last half of stance phase as the first MTP dorsiflexes, and it may become less functional as a hallux valgus deformity develops. As a result, plantar flexion of the first ray might not occur, which can lead to increased pressure under the second metatarsal head and diffuse callus formation.
Hypermobility of the first MTC joint, which may be pathologic in no more than 5% of patients, can also lead to increased weight bearing by the first metatarsal. Pressure is then transferred to the lesser metatarsals, where a diffuse callus can develop beneath the second and possibly third metatarsal ( Fig. 13-2 ). The base of the second and third metatarsals is quite stable because of the rigidity of their tarsometatarsal articulations; therefore if the first metatarsal is hypermobile or elevated from any cause, callus formation can occur beneath the second and third metatarsal heads. The fourth and fifth metatarsals are more mobile, and therefore calluses rarely develop beneath them unless there is an abnormal foot posture or an osseous deformity.

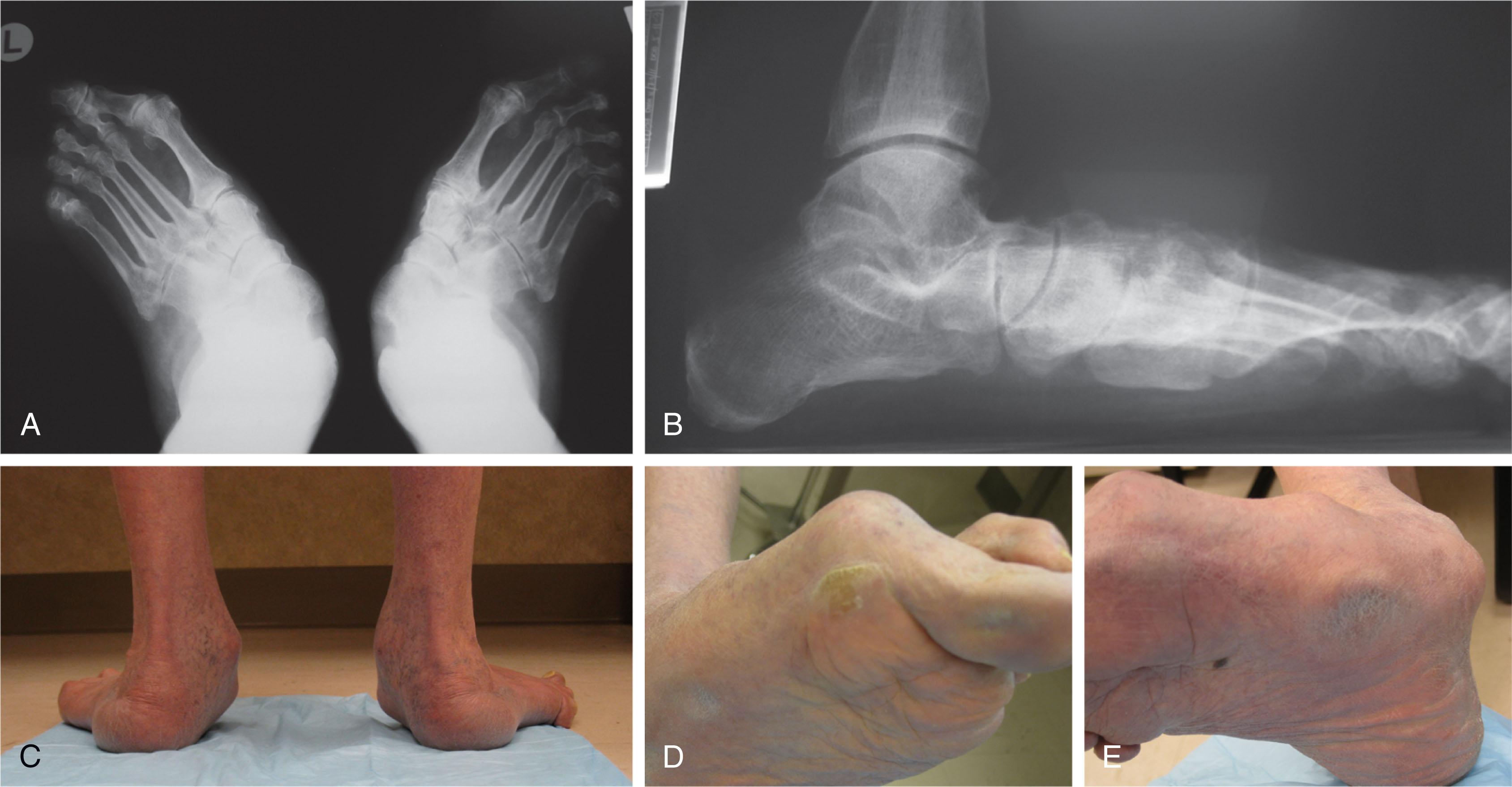
The posture of the foot and entire lower leg must always be considered in evaluating the patient with an intractable plantar keratosis (IPK). Abnormal callus formation can be due to excessive genu varum or valgum, an equinus deformity of the ankle joint, a cavus foot, pes planus, a varus forefoot deformity, a pes planovalgus deformity ( Fig. 13-3 ), or abnormal alignment of the MTP joints. Unless the underlying deformity is addressed, the IPK will persist.
An equinus deformity of the ankle joint that results in increased weight bearing on the metatarsal heads can result in a diffuse callus beneath the first, second, and third metatarsal heads. This can be painful, particularly in the older patient with atrophy of the fat pad. In the patient with an insensate foot, such as the patient with diabetes or a peripheral neuropathy, ulceration of the plantar aspect of the foot can occur. The equinus may be hidden by hindfoot varus or valgus malalignment but revealed on physical exam when the heel is held in a neutral position and the ankle dorsiflexed.
In the cavus foot, the calcaneus is usually in a dorsiflexed position and the forefoot in equinus, leading to an abnormally diminished weight-bearing area and resultant diffuse callus formation beneath the metatarsal head area. This condition often becomes more symptomatic with increasing patient age and fat pad atrophy. With cavovarus hindfoot alignment, the lateral border of the foot also becomes a weight-bearing prominence prone to painful callus formation ( Fig. 13-4 ) (see Chapter 30 ).

The foot with pes planus does not usually develop significant callus formation beneath the metatarsal heads, unless it is associated with a hallux valgus deformity. This combination can lead to callus formation along the plantar medial aspect of the great toe at the level of the interphalangeal (IP) joint. However, with more advanced planovalgus deformity, the patient may bear weight on the talar head in the medial midfoot, leading to painful callosity ( Fig. 13-5 ) (see Chapter 29 ).

A varus forefoot deformity, in which the lateral border of the foot is more plantar flexed than the medial border, often results in a diffuse callus beneath the fifth metatarsal head ( Fig. 13-6 ).
A valgus forefoot deformity, in which the first metatarsal is more plantar flexed in relation to the lesser metatarsals, often results in a diffuse callus beneath the first metatarsal head region ( Fig. 13-7 ). This is often associated with a cavus foot deformity.
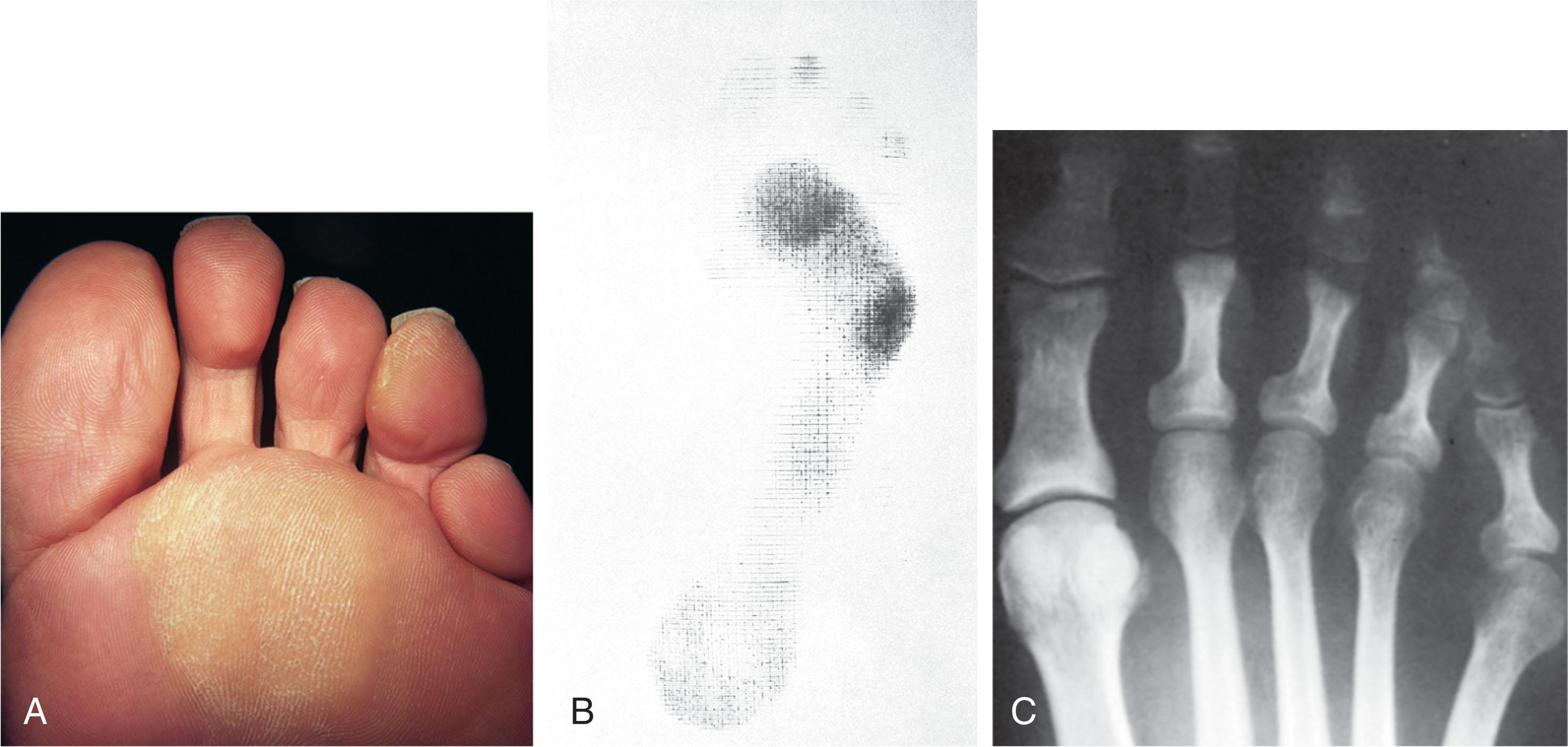
Abnormal alignment of the MTP joints, secondary to either subluxation or dorsal dislocation, results in a plantarward force on the metatarsal head and development of a diffuse callus beneath the involved metatarsal head. An extreme example is a patient with advanced rheumatoid arthritis ( Fig. 13-8 ).
Dynamic deformity may also present, especially in patients with neurologic involvement including peripheral neuropathy, traumatic brain injury, stroke, or hereditary sensory-motor neuropathy ( Fig. 13-9 ). Intrinsic weakness due to peripheral neuropathy may lead to clawing of the toes revealed during stance and gait but resolved at rest. Atypical firing patterns after upper motor neuron injury can cause dynamic pathologic loading of the foot and elevated pressure on the overlying skin.

The evaluation of a patient with a plantar keratotic lesion begins with a careful history of the condition. This should include pertinent medical conditions, history of trauma, prior surgeries, what type of footwear aggravates and relieves the pain, the wear pattern of footwear, as well as what type of treatment has been attempted in the past. Examination of shoes, insoles, and braces may reveal extrinsic contributory factors.
The physical examination begins with the patient standing. Careful observation should be made of the posture of the toes, characteristics of the MTP joints and longitudinal arch, and the position and posture of the hindfoot in relation to the forefoot. Strength testing of all muscle groups, a thorough neurovascular examination, and range of motion of the ankle, subtalar, transverse tarsal, and MTP joints should be noted. Hypermobility of the first ray, the presence of hallux rigidus, as well as swelling, thickening, synovitis, and instability of the lesser MTP joints are important diagnostic findings. Stability of the lesser MTP joints is assessed using the drawer test.
The plantar aspect of the foot is carefully evaluated. The location of the lesion and its characteristics are observed. The callus may consist of a localized seed corn, a discrete plantar keratosis beneath the fibular condyle of a metatarsal head or beneath the tibial sesamoid, a diffuse callus beneath a metatarsal head, or a diffuse callus beneath several metatarsal heads.
Weight-bearing radiographs should be obtained along with sesamoid views, if indicated. A small marker can be placed over the lesion to identify the offending structure if needed.
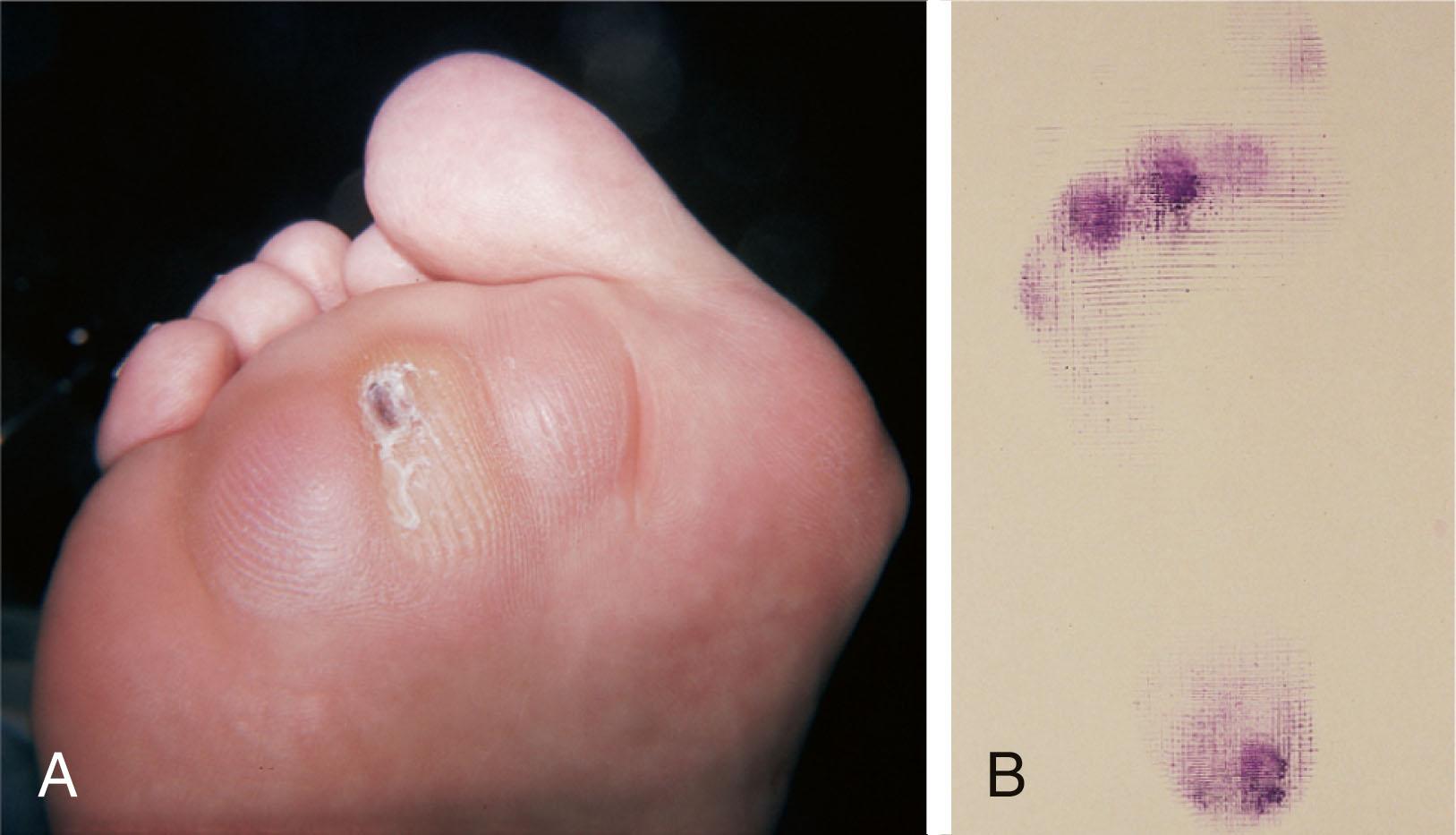
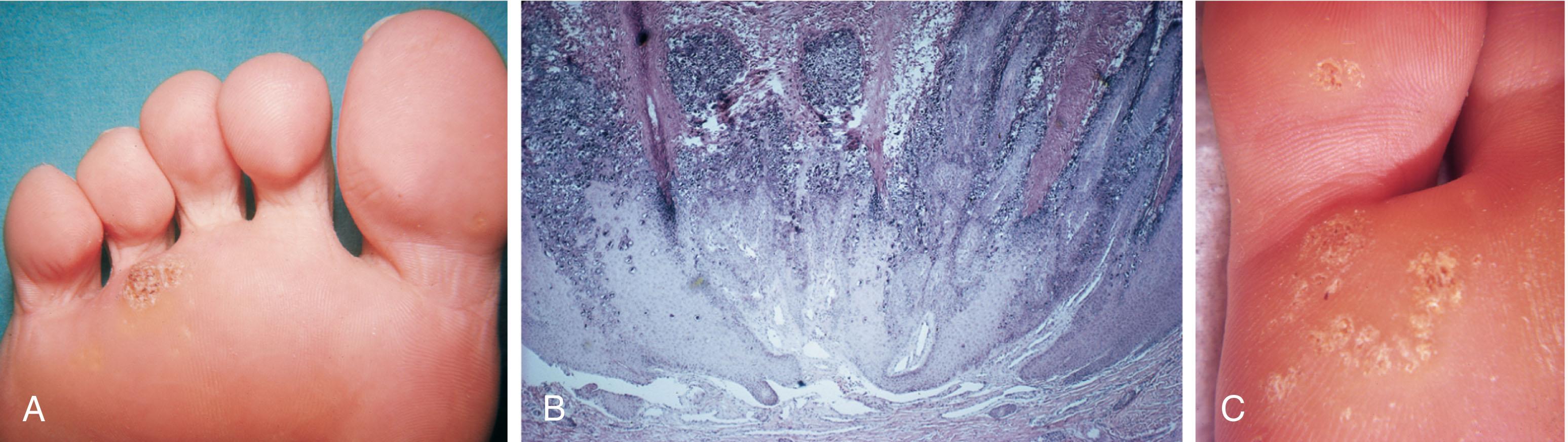
It is important to differentiate a wart, or plantar verruca, from a callus. Plantar verrucae are common, affecting 7% to 10% of the population. A plantar verruca is usually localized but occasionally demonstrates a mosaic pattern and is usually not discretely located beneath a metatarsal head. Papillary lines, or rete ridges, diverge around the lesion, whereas in a callus, the rete run unchanged across the lesion. To facilitate identification, the lesion is often trimmed with a No. 17 blade. Trimming enables the clinician to identify the margins of the callus, because in a well-localized plantar keratosis, the callus itself has definite circumscribed edges, as opposed to a diffuse callus, which is a generalized thickening of the plantar skin without a defined margin.
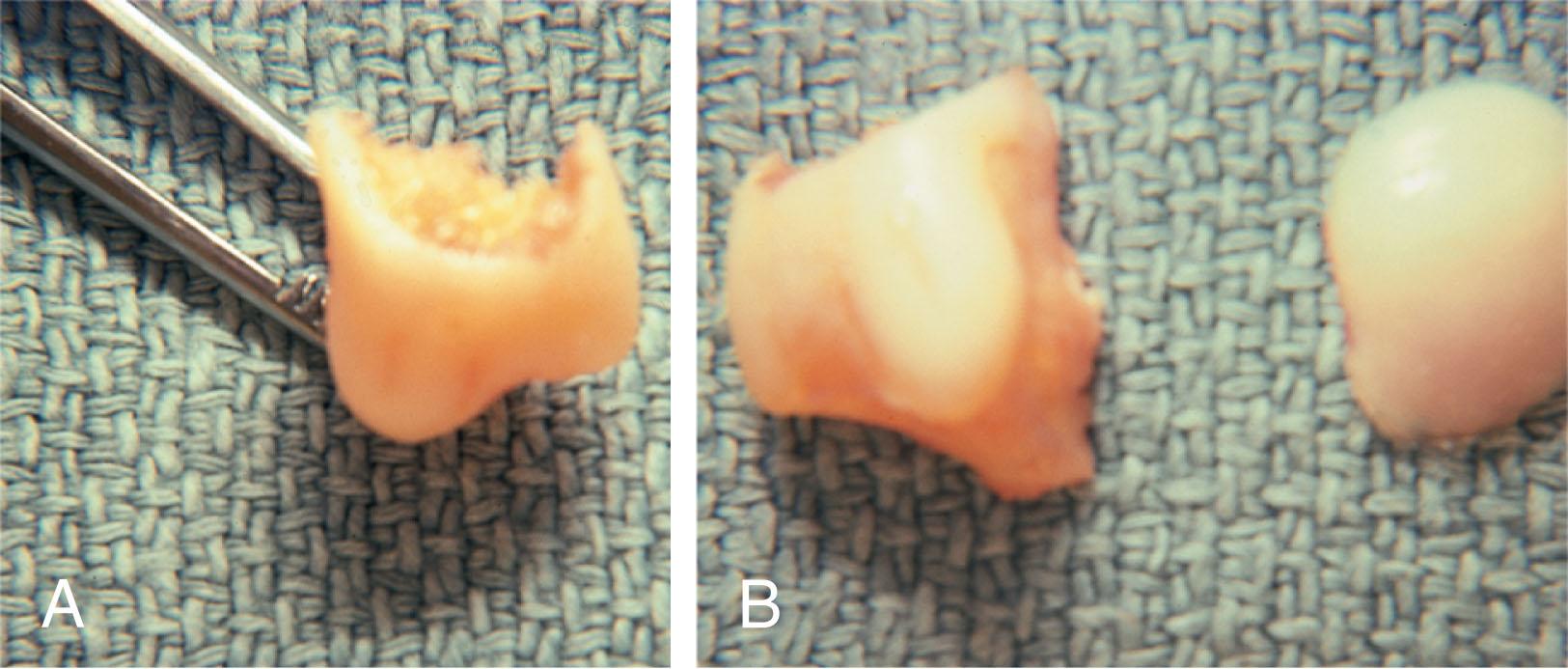
A wart, on the other hand, may have a small amount of hyperkeratotic skin overlying it, but very quickly one enters the warty material, which consists of multiple end arteries that bleed vigorously, as opposed to a true plantar keratosis, which has no blood supply ( Fig. 13-10 ). Warts are commonly caused by the human papilloma virus (HPV), with the dark and moist environment within a shoe facilitating survival. Numerous treatments have been described for this often recalcitrant lesion, including chemical ablation, immunologic modifying treatments, and surgery. Common chemical ablation techniques include phenol, 10% formaldehyde, 10% formaldehyde with monochloroacetic acid, fluorouracil, and bleomycin sulfate. Topical treatments include salicylic acid, fluorouracil, canthadrin and podophyllotoxin, formaldehyde, silver nitrate, corticosteroids, and garlic extract. Cryotherapy and electrocautery have been used with varying results. Surgical excision is often required, with recurrence not uncommon.
Epidermal inclusion cyst on the plantar surface of the foot may mimic an IPK.
Other rare dermatologic lesions that present as plantar callosities include keratosis palmoplantaris nummularis and epithelioma cuniculatum. If these lesions are suspected, dermatology consultation is recommended ( Fig. 13-11 ). Keratosis palmoplantaris nummularis is an autosomal dominant skin disorder characterized by painful callus formation over areas of mechanical stress on the palms and plantar surface of the foot. It often presents upon the onset of walking in a child, with pain being the primary complaint. Physical examination reveals essentially normal motor and sensory function, with multiple areas of large hyperkeratotic callus formation over weight-bearing areas of the feet that are confluent with the surrounding skin. Histologic evaluation is consistent with epidermolytic hyperkeratosis. Operative treatment has been reported to be unsuccessful. The mainstay of treatment is shaving of the callosities, orthotics, and footwear modification. The natural history and successful treatment of the disorder remain elusive.

Epithelioma cuniculatum is a form of verrucous carcinoma that affects the plantar surface of the feet. It is an uncommon low-grade squamous cell carcinoma that is typically slow growing and has a tendency to local recurrence. Although metastatic disease is rare, lack of timely diagnosis can lead to its spread. It can present as a painless, nonhealing ulceration on the plantar surface of the foot that slowly increases in size and is refractory to standard callus treatment. Diagnosis of this rare lesion can be challenging, and deep biopsy is required. The HPV has been implicated as a causative factor, but both HPV-positive and -negative lesions have been reported. Histologic analysis reveals a well-differentiated tumor composed of keratinocytes that extend the dermis and deeper structures, forming sinuses and keratin-filled cysts. Tumor cells in the granular layer may show vacuoles. There is often marked hyperkeratosis, with perakeratosis of a prominent granular layer occasionally seen. Treatment options include imiquimod (a topical immune-modulating drug), carbon dioxide (CO 2 ) laser ablation, and surgical excision.
The plantar callus can be trimmed with a sharp knife. A No. 15 or No. 17 podiatric blade is especially useful for trimming of hyperkeratotic skin. When trimming a callus, one should attempt to reduce the hyperkeratotic tissue, and if it is invaginated, this too should be trimmed. With a deep-seated lesion, however, it may not be possible to remove all of the keratotic lesion at the first trimming, and several trimmings may be necessary to permit the deep-seated portion of the callus to surface. Occasionally, a seed corn, which is a well-localized keratotic lesion, usually 2 to 3 mm in diameter, can be removed at the first sitting, although it might require a second trimming ( Fig. 13-12 ). Care must be given to diabetic or neuropathic patients to avoid creating a wound that can become infected; it is better to bring the patient back for a second look than trim into the subdermal layers.
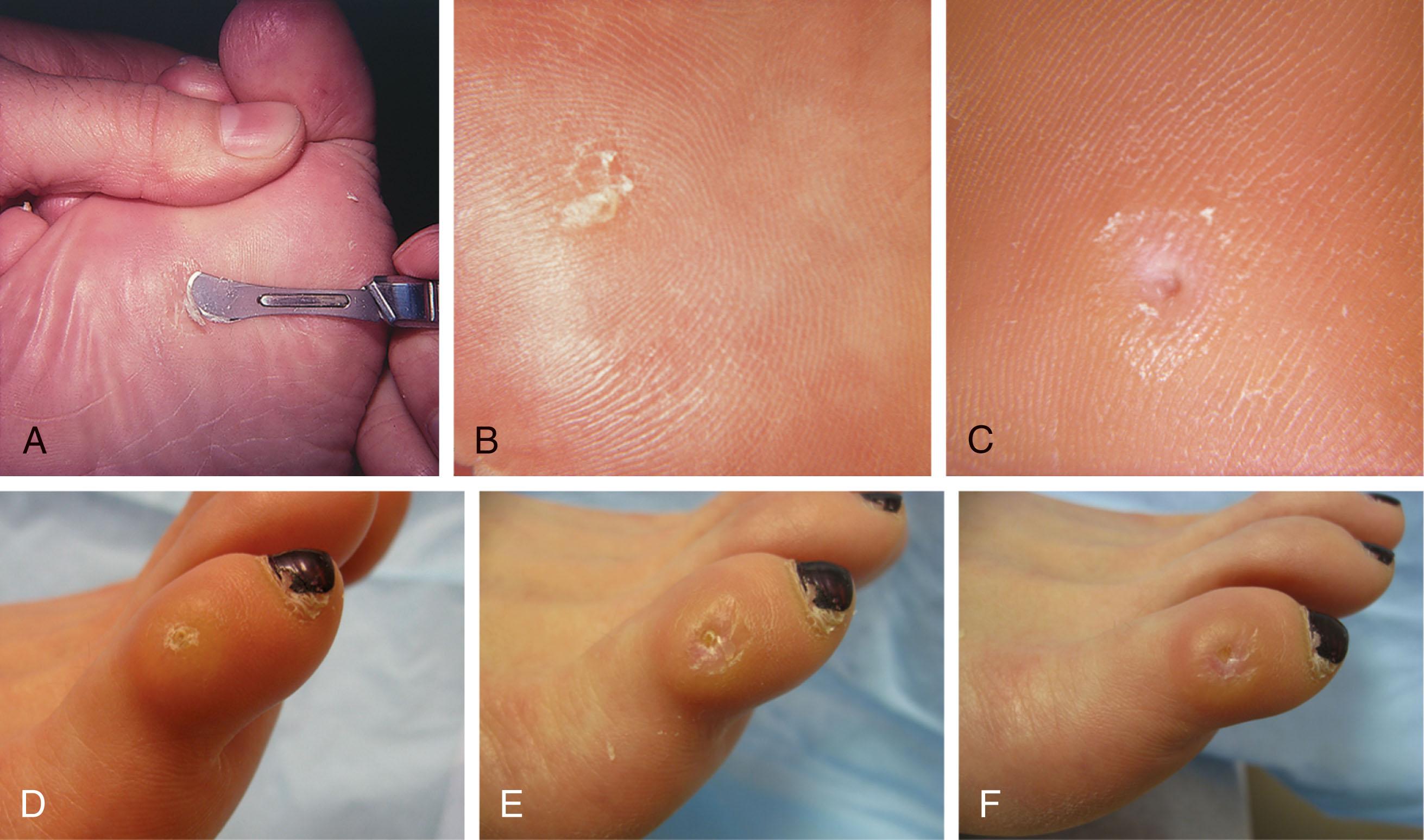
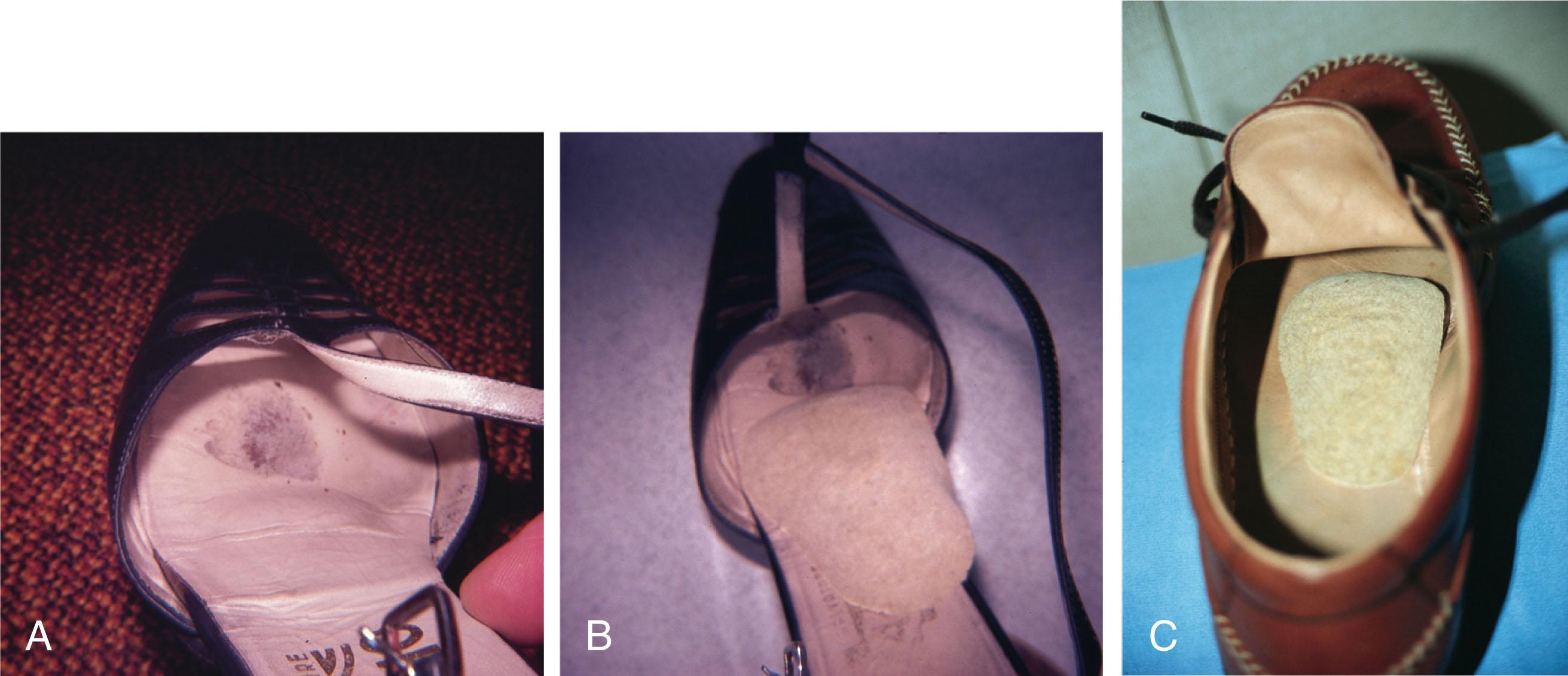
After debridement of the callus, a soft metatarsal support is used to relieve pressure on the involved area ( Fig. 13-13 ). A “dancer’s” pad contains a cutout, making it ideal for IPK under the sesamoids. For other areas, a donut-type pad may be appropriate to reduce pressure on the symptomatic region. The soft support can be used, provided that the patient’s shoe is of adequate size. If the patient is wearing stylish women’s dress shoes, there may not be sufficient volume for the foot and the metatarsal support. The patient with a significant keratotic lesion should be encouraged to wear a broad, stiff-soled, preferably low-heeled shoe with soft, accommodative insole to provide more cushioning for the plantar aspect of the foot but prevent excess pressure on the metatarsal heads after heel-rise. The metatarsal support should be placed into the shoe just proximal to the area of the lesion ( Fig. 13-14 ). It is important to instruct the patient that this support may initially feel uncomfortable and may take a period of breaking in of a week to 10 days. However, if the pad drifts to position direction under the painful lesion, it needs to be readjusted.
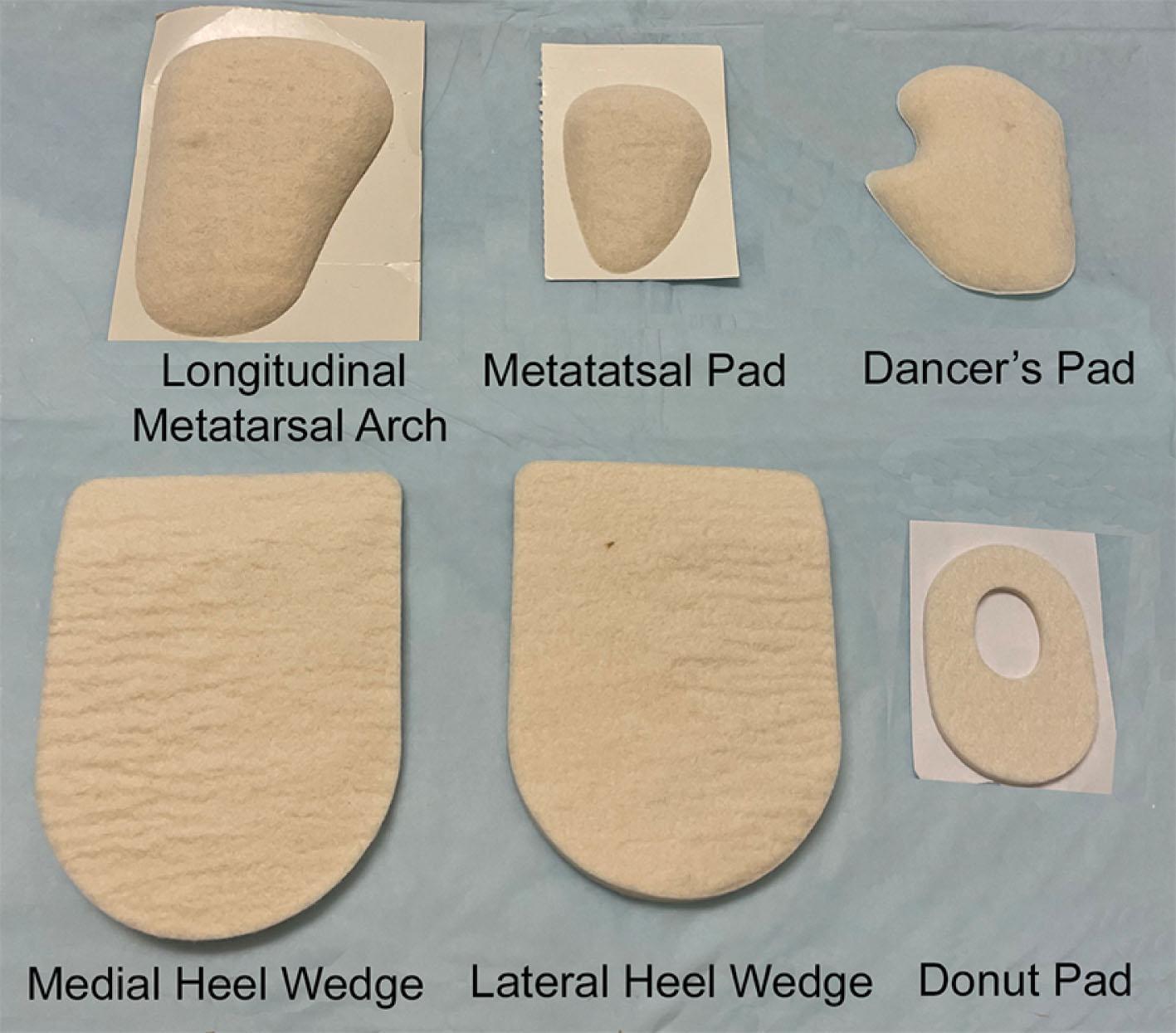
The patient is then seen periodically in the office for trimming of the lesion, adjustment of the metatarsal support, and possibly even placement of a larger one, as necessary. If the patient has a postural abnormality of the foot, such as forefoot varus or valgus, or possibly a pes planovalgus deformity or a cavus foot, a custom-made, well-molded orthotic or felt heel wedge may be of benefit.
Dry needling, injection of saline, and injection of lidocaine were no more beneficial than debridement and were poorly tolerated by patients in a prospective feasibility study. Injection of platelet-rich plasma (PRP) after paring was not more beneficial than saline injection.
Other footwear modification, such as a wide or tall toe box or the addition of a rocker-bottom sole, can potentially provide relief. If an equinus contracture is a contributing cause, physical therapy to stretch the gastrocsoleus complex and strengthen the ankle dorsiflexors can increase the relative length of the Achilles tendon unit, thereby increasing ankle dorsiflexion. Gait retraining to encourage the patient to shift their center of gravity posteriorly, stretch the hip musculature to allow increased range of motion, and relax the gastrocsoleus musculature during toe off may further off-weight the forefoot.
If the callus persists and is symptomatic, surgical intervention can be considered.
Surgical management of a plantar keratosis is based on the characteristics of the callus.
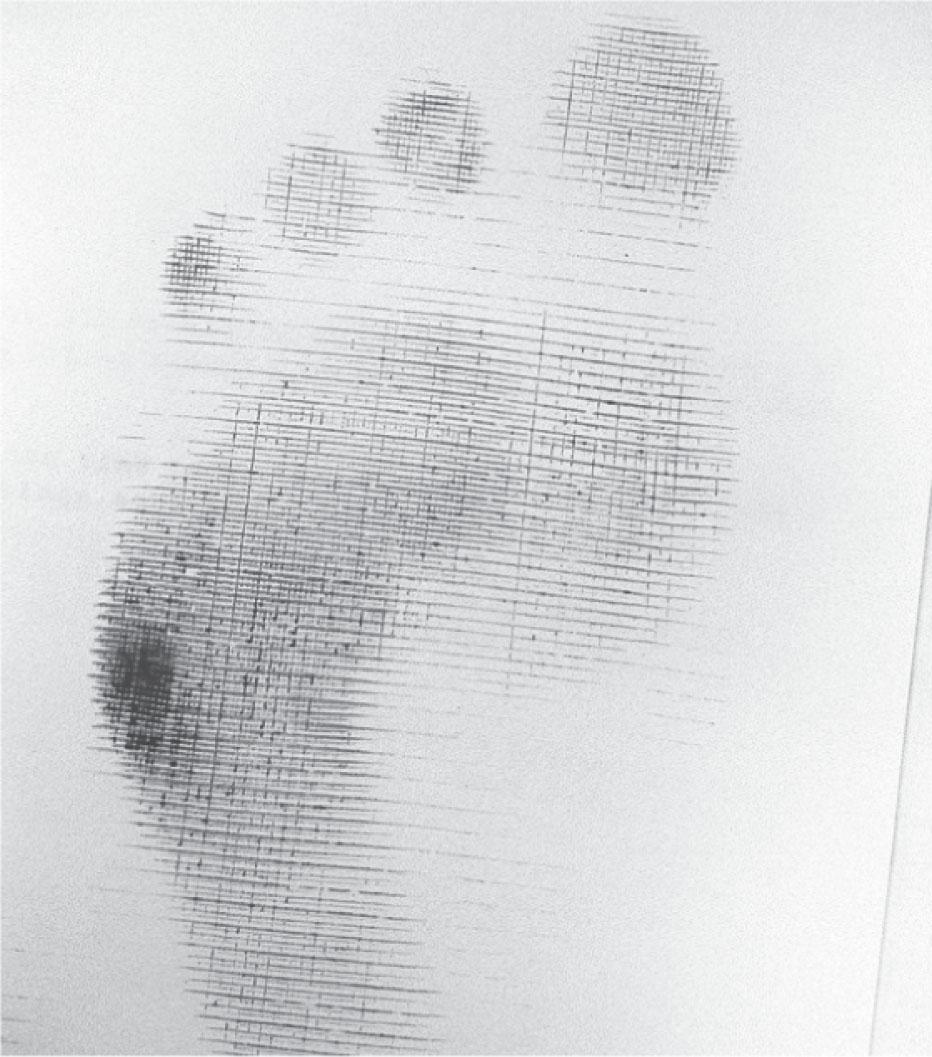
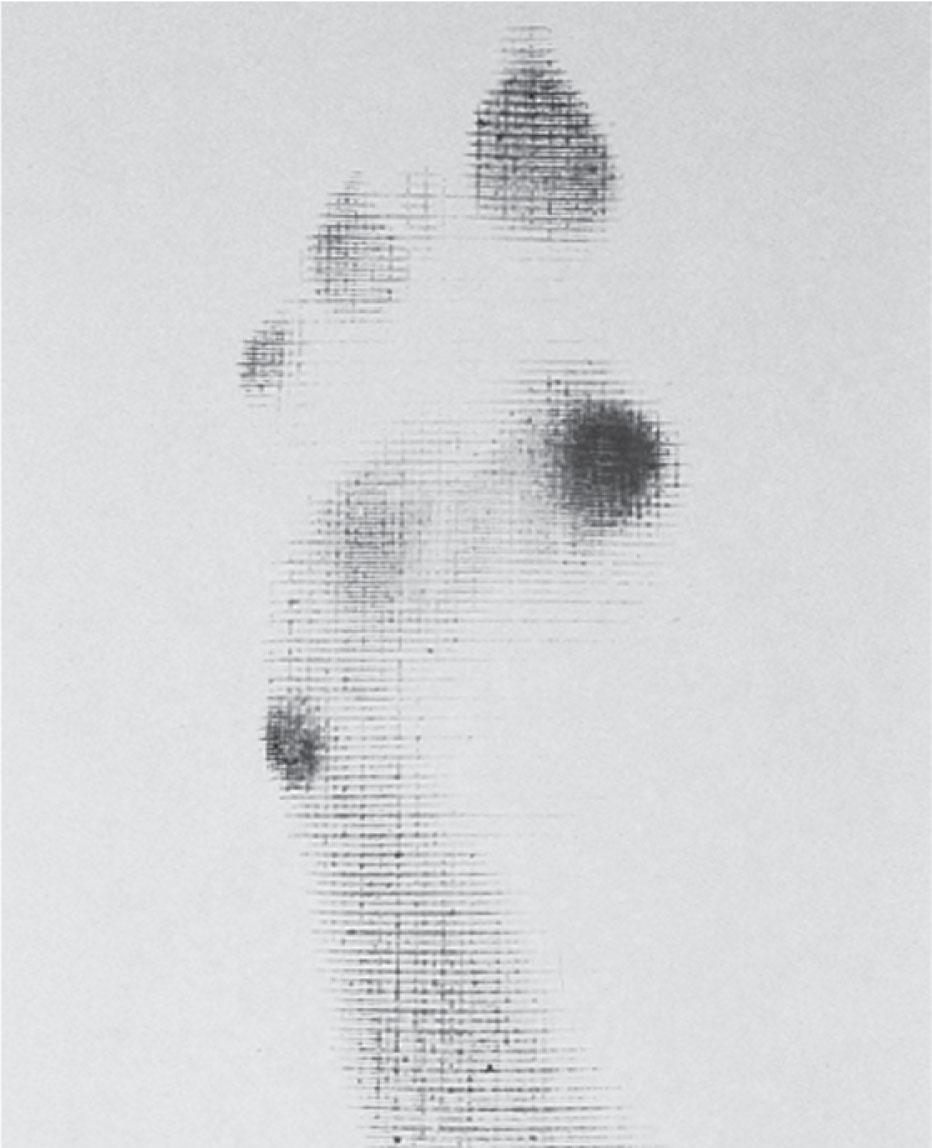
A discrete callus with a central keratotic core is observed beneath the fibular condyle of the metatarsal head and beneath the tibial sesamoid ( Fig. 13-15 ). When the patient with a discrete, localized lesion walks over a Harris mat, the imprint created is well localized beneath the prominence that has brought about the callus ( Fig. 13-16 ). Histologically, this lesion is a dense, keratinized lesion with a central core ( Fig. 13-17 ).

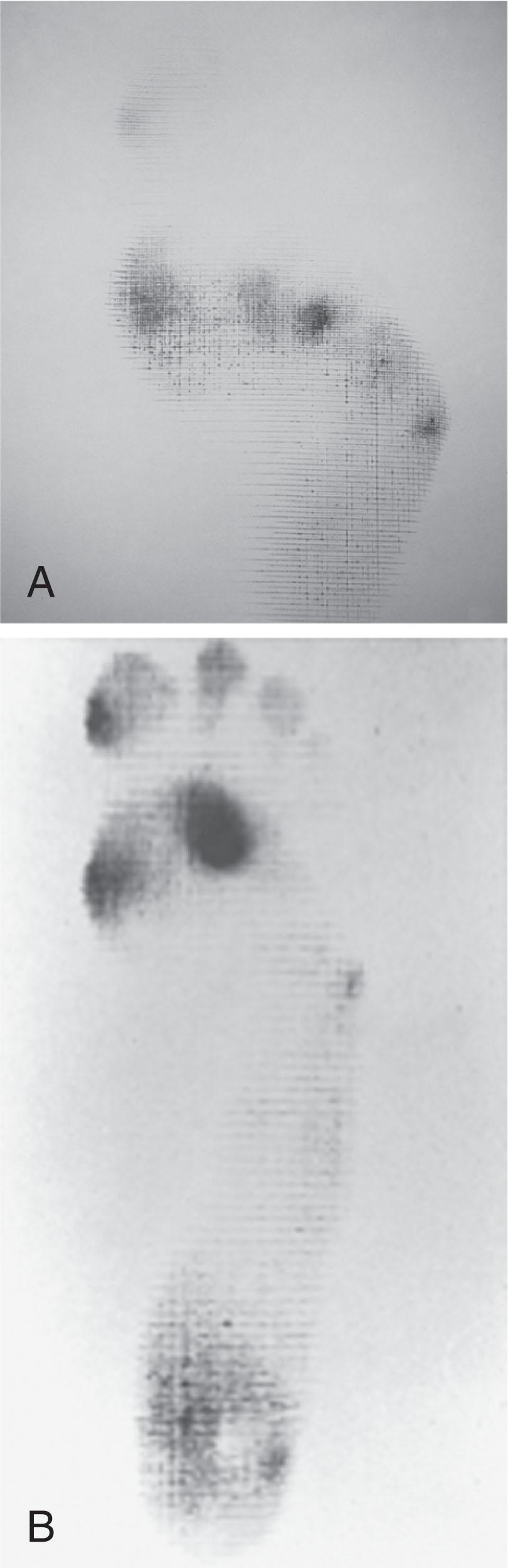
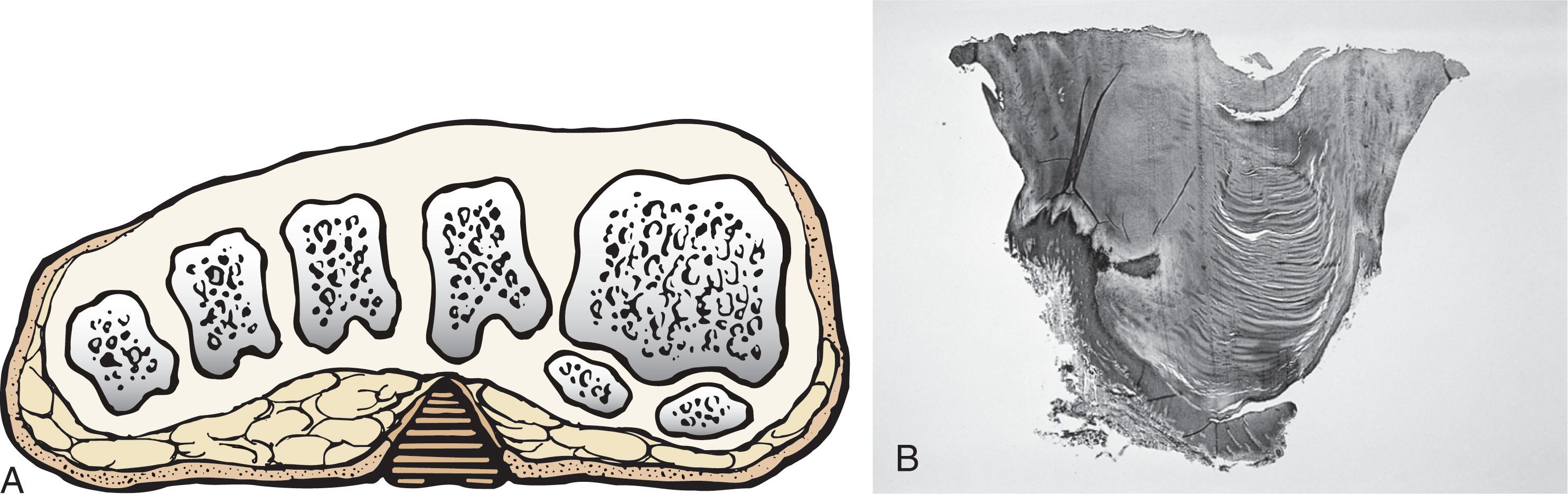
This should be differentiated from a diffuse callus, which is often caused by deformity at the MTP joints because of instability, and usually associated with abnormal weight bearing during the third rocker portion of the gait cycle, in which only the forefoot is in contact with the ground ( Fig. 13-18 ). A diffuse callus is observed beneath a metatarsal head that does not have a prominent fibular condyle and is noted most often beneath the second metatarsal head. Occasionally, a diffuse callus is noted beneath multiple metatarsal heads. When this type of callus is present and is trimmed, although the material consists of hyperkeratotic skin, there is no central core as observed in a discrete callus. When this patient walks over a Harris mat, the print that is observed is diffuse beneath the entire metatarsal head or beneath multiple metatarsal heads ( Fig. 13-16 ). In general, a callus underneath several metatarsals is often due to forefoot overload, such as seen in ankle equinus; plantar flexion of the metatarsals, as in a cavus foot; or first-ray insufficiency. This indicates overload during the foot flat portion of the gait cycle during the second rocker portion of swing phase. This type of diffuse lesion is occasionally observed beneath the first metatarsal head if it is plantar flexed. It can be observed beneath the second metatarsal head when the first metatarsal is short, hypermobile, or due to first-ray instability brought about by an advanced hallux valgus deformity or possibly insufficiency after bunion surgery, if the joint has been destabilized. A diffuse callus beneath the second, third, and fourth metatarsal heads is usually observed in a patient with an extremely short first metatarsal, which results in increased weight bearing beneath the three middle metatarsals ( Fig. 13-19 ). Occasionally, a diffuse callus is present beneath the fifth metatarsal head in patients with a varus configuration of the forefoot, or with a plantar-flexed fifth metatarsal associated with a tailor’s bunion.

A diffuse type of callus can also result after trauma. A metatarsal malunion can result in a plantar-flexion deformity and resultant callus underneath the fractured metatarsal. A dorsiflexion malunion can lead to callus formation beneath an adjacent metatarsal, with the normal metatarsal left to bear increased weight.
Differentiating the type of callus is essential because the nature of the callus determines the type of surgical procedure that will give the best result. In general, a localized callus will require an elevating procedure, whereas a diffuse callus requires a shortening procedure.
A localized IPK, which is usually caused by the prominence of the fibular condyle, can be treated by a DuVries metatarsal condylectomy. DuVries initially described the procedure in which he carried out an arthroplasty of the MTP joint by removing a portion of the distal articular surface and the plantar condyle. Coughlin and Mann modified the procedure by removing only the plantar condyle. Both procedures seem to lead to satisfactory clinical results.
The technique is as follows.
A hockey stick–shaped incision begins in the second web space and is carried across the metatarsal head proximally to about the distal third of the metatarsal shaft ( Fig. 13-20A ).
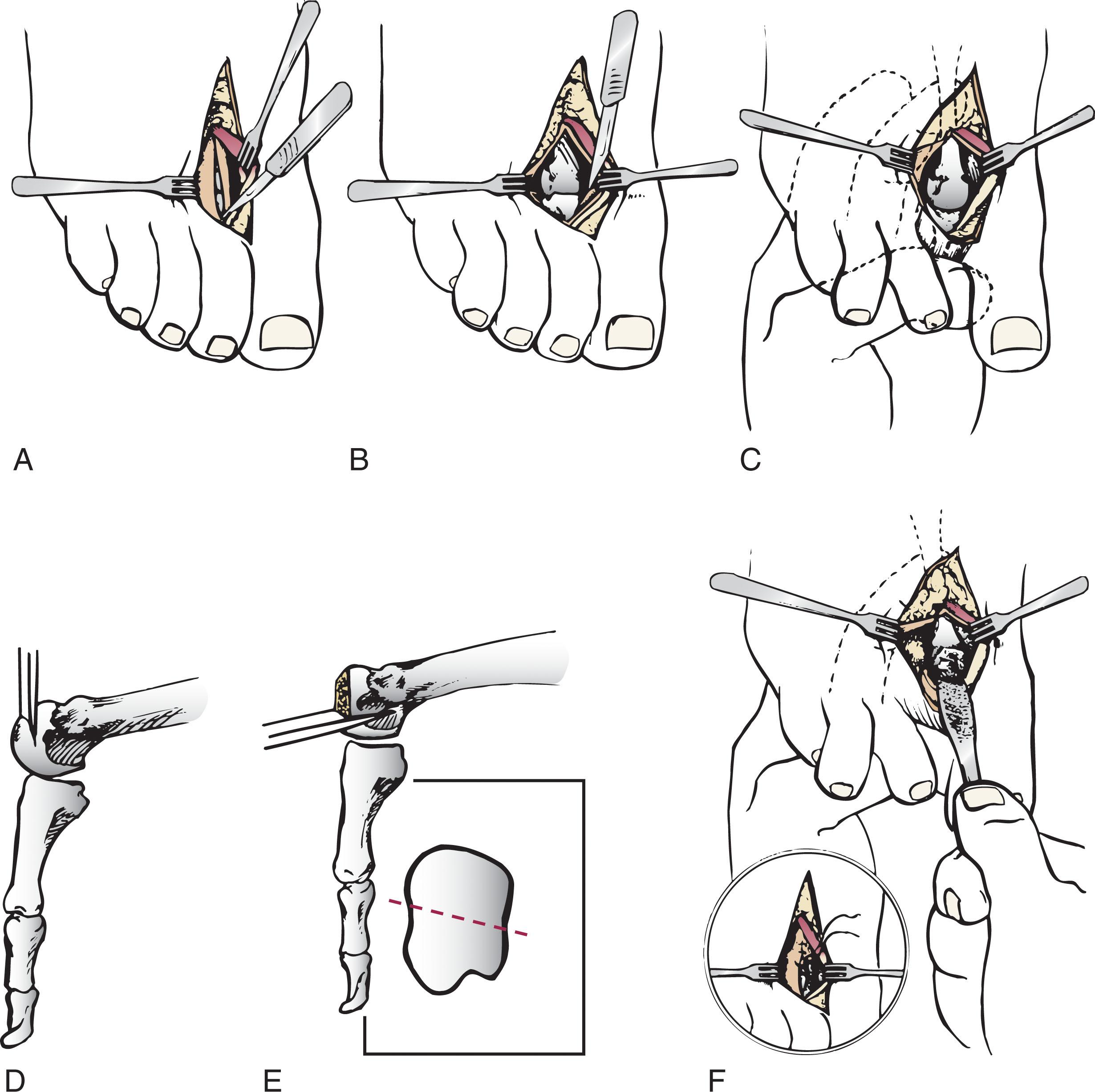
Passing medially and laterally to the extensor hood, the transverse metatarsal ligament is identified and released.
The interval between the long and short extensor tendons is opened and continued through the joint capsule to expose the MTP joint.
The collateral ligaments are transected, and the MTP joint is sharply plantar flexed while pressure is applied to the plantar aspect of the foot with the index finger of the same hand ( Fig. 13-20B and C ).
The distal 2 mm of articular cartilage is removed from the metatarsal head in a plane perpendicular to the metatarsal shaft. As this cut is made, the osteotome is angled slightly proximally; otherwise, it will skid off the cartilage and make an oblique cut ( Fig. 13-20D ).
The MTP joint is now sharply plantar flexed to bring into view the plantar condyle. The plantar 20% to 30% of the metatarsal head is removed with a 10- to 12-mm thin osteotome. The osteotome is angled slightly plantarward to avoid inadvertent splitting of the metatarsal shaft ( Fig. 13-20E ).
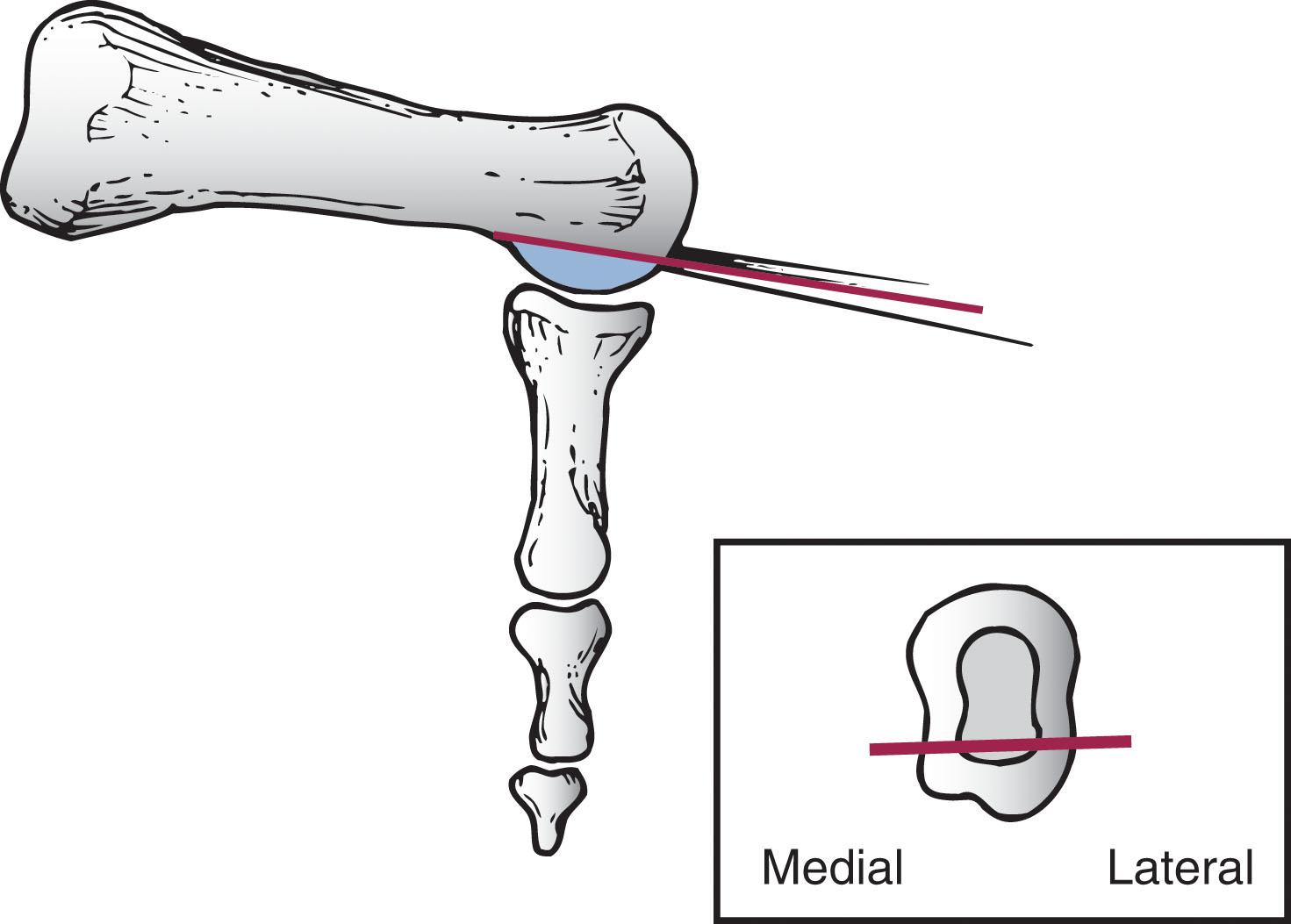
On completion of the osteotomy in the metatarsal head, the plantar condyle is delivered by use of a Freer elevator or thin rongeur in the adjacent interspace, and the condyle is removed. It is difficult to pull this fragment of bone out directly over the proximal phalanx, so it is pushed into the interspace and removed ( Fig. 13-21 ).
The edges are carefully rongeured, and the joint is reduced ( Fig. 13-20F ). The skin is closed in a routine manner.
A gentle compression dressing is applied for 12 to 18 hours, and the patient is permitted to ambulate in a postoperative shoe.
The bulky surgical dressing is changed after 18 to 24 hours, and the patient is placed into a snug compression dressing consisting of 2-inch conforming gauze (Kling) and adhesive tape. The patient is permitted to ambulate in the postoperative shoe, which is worn for 3 weeks. The shoe is removed, and the patient is encouraged to work on range-of-motion exercises.
Mann and DuVries reported on 100 patients after metatarsal condylectomy. It was observed that 42% of the lesions were beneath the second metatarsal head, 31% beneath the third, 19% beneath the fourth, and 8% beneath the fifth. Overall, there was 93% patient satisfaction.
A transfer lesion occurred in 13% of the patients, and the original lesion failed to resolve in 5%. The 5% complication rate included fracture of a metatarsal head, avascular necrosis of the metatarsal head, and clawing of the toe. There were no cases of dislocation of the MTP joint after this procedure. Postoperative range of motion of the MTP joint rarely demonstrates more than 25% loss of motion. It has always been somewhat surprising that so little motion is lost after this type of arthroplasty, whereas when a similar procedure is carried out for a dislocated MTP joint, significantly more motion is lost.
The modification of the condylectomy by Coughlin is carried out in the same way as the DuVries metatarsal condylectomy, except that the distal portion of the metatarsal is not removed ( Fig. 13-22 ). This makes removing the plantar condyle a little more difficult. Until now, there has been no published report regarding the results of this modification of the DuVries procedure, although preliminary data indicate about a 5% incidence of transfer lesions. The use of a power rasp with which to shave down the prominent fibular condyle has been described. This avoids the potential difficulty of retrieving the osteotomized plantar condyle from the interspace. Thermal necrosis and bone debris can be avoided by irrigating during burring.
Dreeben et al described a vertical chevron osteotomy of the distal metaphyseal metatarsal with 3 mm elevation of the head for treatment of a painful callus beneath the metatarsal head. The article did not classify the callus into a localized or diffuse category.
The technique is as follows.
A 2-cm dorsal incision is made over the metatarsal head and neck region. The extensor tendons are retracted, the metatarsal neck exposed subperiosteally, and the plantar periosteum left intact. The MTP joint is not entered.
A chevron-type cut with the apex based distally is produced with a power saw just proximal to the edge of the dorsal joint capsule. An attempt should be made to leave the plantar periosteum intact ( Fig. 13-23 ).

The metatarsal head is displaced dorsally by plantar pressure but not more than 3 to 4 mm.
The osteotomy site is stabilized with a 0.045-inch Kirschner wire introduced through a separate stab wound. The skin is closed in a routine manner.
The patient walks in a postoperative shoe with weight bearing as tolerated. The Kirschner wire is removed after 3 weeks, and gentle range of motion is begun at that time. The postoperative shoe is continued for a total of 6 weeks.
Dreeben et al reported 45 patients after the vertical Chevron procedure. Complete relief of the symptoms was noted in 67%, 24% had residual pain, 9% demonstrated a transfer lesion, and in 4%, the callus was unchanged. The authors pointed out that the metatarsal head should be elevated at least 3 mm but not more than 4.5 mm. Kitaoka and Patzer used the same procedure on 21 feet, with a mean age of 59 years (32–85). They reported good results in 16, fair in 2, and poor in 3. In four patients (20%), the callosity persisted, and in three (14%), a transfer lesion developed.
Pontious et al found a high complication rate in 40 patients treated for IPK with vertical chevron with or without internal fixation including 43% transfer lesions or metatarsalgia, 10% recurrence, and 25% floating toe. Fixation was not found to improve results other than time to osteotomy healing.
Excision of the localized IPK and rotational soft tissue coverage has been recommended. A series of 54 consecutive cases was studied after excision of callus for IPK or plantar wart, with improvement in pain and functional outcome scores and 89% of patients reporting the surgery achieved their expectations. Longer term follow-up is required to evaluate the recurrence, however, since the underlying pathology is not addressed.
A discrete callus beneath the first metatarsal head typically lies under the tibial sesamoid. A localized lesion does not occur beneath the fibular sesamoid. A diffuse callus can be observed beneath the entire first metatarsal and is usually associated with a plantar-flexed metatarsal, as seen in the patient with a cavus foot or Charcot-Marie-Tooth disease.
The lesion beneath the tibial sesamoid can often be managed conservatively, although when it occurs after bunion surgery and the sesamoid is localized beneath the crista of the metatarsal head, surgical intervention is usually required ( Fig. 13-24 ).

Tibial sesamoid shaving involves removing the plantar half of the sesamoid directly over the discrete callosity. This is associated with significantly less morbidity than excision of the sesamoid for this problem.
The technique is as follows.
The skin incision is made slightly plantar to the midline and centered over the medial aspect of the MTP joint. The incision is carried down to the capsular structures without undermining the skin ( Fig. 13-25A and B ).
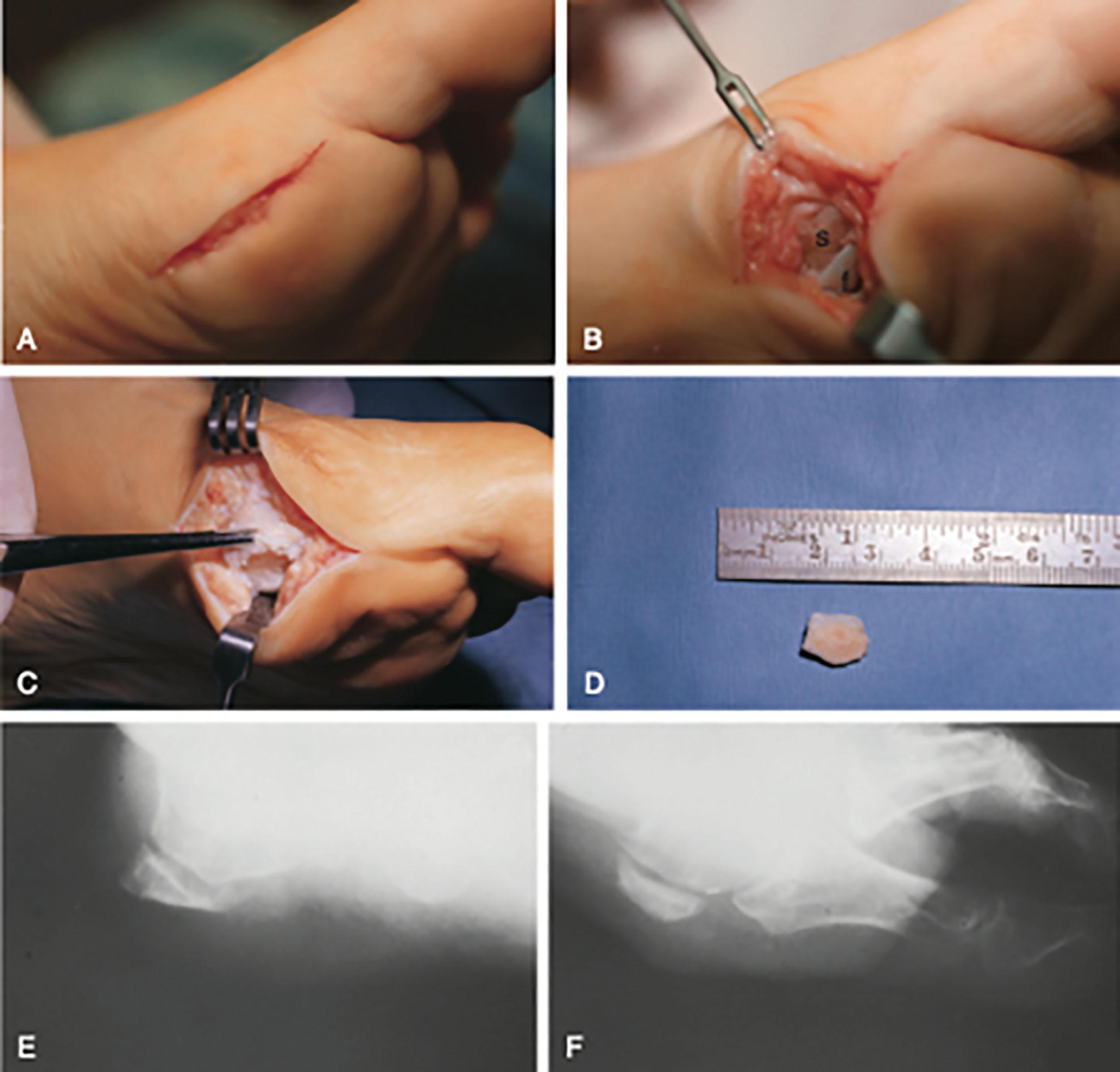
Along the capsular plane, the incision is developed in a plantar direction over the medial aspect of the tibial sesamoid. Great care is taken to identify the medial plantar cutaneous nerve, which often passes with a small vessel along the plantar aspect of the abductor hallucis tendon.
With the nerve identified and retracted plantarward, the periosteum over the tibial sesamoid is stripped plantarly to expose the plantar two thirds of the sesamoid. The plantar half of the tibial sesamoid is removed with a small oscillating saw, and the edges are smoothed ( Fig. 13-25C and D ). Care must be taken to avoid injury to the flexor hallucis longus (FHL) tendon, which lies just lateral to the medial sesamoid. The integrity of the FHB tendon on the remaining sesamoid is also checked.
The wound is closed in a routine manner, and a compression dressing is applied ( Fig. 13-25E and F ).
The patient is kept in a postoperative shoe with the foot in a firm dressing for 3 weeks and then is permitted to ambulate as tolerated.
A follow-up study of 12 patients after plantar sesamoid shaving demonstrated that 58% had excellent results with no recurrent callus, 33% had good results with slight recurrence of the callus, and 1 patient (9%) had a fair result and required periodic trimming of the plantar callus. All patients maintained full range of motion of the first MTP joint, and none had a painful scar.
The most significant complication after this procedure is injury to the medial plantar cutaneous nerve. If this occurs and is noted at surgery, the surgeon must consider freeing up the nerve more proximally and moving it away from the plantar aspect of the foot. If the damage to the nerve appears to be too severe, the surgeon must consider whether the nerve should be sectioned and buried beneath the abductor hallucis muscle to prevent a neuroma from forming on the plantar medial aspect of the foot.
Further discussion of tibial sesamoid shaving is presented in Chapter 11 .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here