Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Juvenile idiopathic arthritis (JIA) is the most common rheumatic disease in children and one of the more common chronic illnesses of childhood. JIA represents a heterogeneous group of disorders sharing the clinical manifestation of arthritis. The etiology and pathogenesis of JIA are largely unknown, and the genetic component is complex, making clear distinction among various subtypes difficult. As a result, several classification schemes exist, each with its own limitations. The former classification of the American College of Rheumatology (ACR) uses the term juvenile rheumatoid arthritis and categorizes the disease into 3 onset types ( Table 180.1 ). Attempting to standardize nomenclature, the International League of Associations for Rheumatology (ILAR) proposed a different classification using the term juvenile idiopathic arthritis ( Table 180.2 ), inclusive of all subtypes of chronic juvenile arthritis. We refer to the ILAR classification criteria; see Chapter 181 for enthesitis-related arthritis (ERA) and psoriatic JIA ( Tables 180.3 and 180.4 ).
Age at onset: <16 yr
Arthritis (swelling or effusion, or the presence of ≥2 of the following signs: limitation of range of motion, tenderness or pain on motion, increased heat) in ≥1 joint
Duration of disease: ≥6 wk
Onset type defined by type of articular involvement in the 1st 6 mo after onset:
Polyarthritis: ≥5 inflamed joints
Oligoarthritis: ≤4 inflamed joints
Systemic-onset disease: arthritis with rash and a characteristic quotidian fever
Exclusion of other forms of juvenile arthritis
| CATEGORY | DEFINITION | EXCLUSIONS |
|---|---|---|
| Systemic JIA | Arthritis in ≥1 joint with, or preceded by, fever of at least 2 wk in duration that is documented to be daily (quotidian * ) for at least 3 days and accompanied by ≥1 of the following:
|
|
| Oligoarthritis | Arthritis affecting 1-4 joints during 1st 6 mo of disease; 2 subcategories are recognized:
|
|
| Polyarthritis (RF negative) | Arthritis affecting ≥5 joints during 1st 6 mo of disease; a test for RF is negative | a, b, c, d, e |
| Polyarthritis (RF positive) | Arthritis affecting ≥5 joints during 1st 6 mo of disease; ≥2 tests for RF at least 3 mo apart during 1st 6 mo of disease are positive | a, b, c, e |
| Psoriatic arthritis | Arthritis and psoriasis, or arthritis and at least 2 of the following: | b, c, d, e |
| Enthesitis-related arthritis | Arthritis and enthesitis, ‖ or arthritis or enthesitis with at least 2 of the following: | a, d, e |
|
||
| Undifferentiated arthritis | Arthritis that fulfills criteria in no category or in ≥2 of the above categories. |
* Quotidian fever is defined as a fever that rises to 39°C (102.2°F) once daily and returns to 37°C (98.6°F) between fever peaks.
† Serositis refers to pericarditis, pleuritis, or peritonitis, or some combination of the 3.
‡ Dactylitis is swelling of ≥1 digit(s), usually in an asymmetric distribution, that extends beyond the joint margin.
§ A minimum of 2 pits on any 1 or more nails at any time.
‖ Enthesitis is defined as tenderness at the insertion of a tendon, ligament, joint capsule, or fascia to bone.
¶ Inflammatory lumbosacral pain refers to lumbosacral pain at rest with morning stiffness that improves on movement.
| PARAMETER | ACR (1977) | ILAR (1997) |
|---|---|---|
| Term | Juvenile rheumatoid arthritis (JRA) | Juvenile idiopathic arthritis (JIA) |
| Minimum duration | ≥6 wk | ≥6 wk |
| Age at onset | <16 yr | <16 yr |
| ≤4 joints in 1st 6 mo after presentation | Pauciarticular | Oligoarthritis:
|
| >4 joints in 1st 6 mo after presentation | Polyarticular | Polyarthritis, RF negative Polyarthritis, RF positive |
| Fever, rash, arthritis | Systemic onset | Systemic |
| Other categories included | Exclusion of other forms | Psoriatic arthritis Enthesitis-related arthritis Undifferentiated:
|
| Inclusion of psoriatic arthritis, inflammatory bowel disease, ankylosing spondylitis | No (see Chapter 181 ) | Yes |
| ILAR SUBTYPE | PEAK AGE at ONSET (yr) | FEMALE:MALE RATIO | % of ALL JIA CASES | ARTHRITIS PATTERN | EXTRAARTICULAR FEATURES | LABORATORY INVESTIGATIONS | NOTES ON THERAPY |
|---|---|---|---|---|---|---|---|
| Systemic arthritis | 1-5 | 1 : 1 | 5-15 | Polyarticular, often affecting knees, wrists, and ankles; also fingers, neck, and hips | Daily fever; evanescent rash; pericarditis; pleuritis | Anemia; WBC ↑↑; ESR ↑↑; CRP ↑↑; ferritin ↑; platelets ↑↑ (normal or ↓ in MAS) | Less responsive to standard treatment with MTX and anti-TNF agents; consider IL-1 or IL-6 inhibitors in resistant cases or as first-line therapy |
| Oligoarthritis | 2-4 | 3 : 1 | 40-50 (but ethnic variation) | Knees ++; ankles, fingers + | Uveitis in 30% of cases | ANA positive in 60%; other test results usually normal; may have mildly ↑ ESR/CRP | NSAIDs and intraarticular corticosteroids; MTX occasionally required |
| Polyarthritis: | |||||||
| RF negative | 2-4 and 10-14 | 3 : 1 and 10 : 1 | 20-35 | Symmetric or asymmetric; small and large joints; cervical spine; temporomandibular joint | Uveitis in 10% | ANA positive in 40%; RF negative; ESR ↑ or ↑↑; CRP ↑ or normal; mild anemia | Standard therapy with MTX and NSAIDs; then, if nonresponsive, anti-TNF agents or other biologics, including abatacept, indicated as first-line therapy |
| RF positive | 9-12 | 9 : 1 | <10 | Aggressive symmetric polyarthritis | Rheumatoid nodules in 10%; low-grade fever | RF positive; ESR ↑↑; CRP ↑/normal; mild anemia | Long-term remission unlikely; early aggressive therapy is warranted |
| Psoriatic arthritis | 2-4 and 9-11 | 2 : 1 | 5-10 | Asymmetric arthritis of small or medium-sized joints | Uveitis in 10%; psoriasis in 50% | ANA positive in 50%; ESR ↑; CRP ↑ or normal; mild anemia | NSAIDs and intraarticular corticosteroids; MTX, anti-TNF agents |
| Enthesitis-related arthritis | 9-12 | 1 : 7 | 5-10 | Predominantly lower limb joints affected; sometimes axial skeleton (but less than in adult, ankylosing spondylitis) | Acute anterior uveitis; association with reactive arthritis and inflammatory bowel disease | 80% of patients positive for HLA-B27 | NSAIDs and intraarticular corticosteroids; consider sulfasalazine as alternative to MTX; anti-TNF agents |
The worldwide incidence of JIA ranges from 0.8-22.6 per 100,000 children per year, with prevalence ranges from 7-401 per 100,000. These wide-ranging numbers reflect population differences, particularly environmental exposure and immunogenetic susceptibility, along with variations in diagnostic criteria, difficulty in case ascertainment, and lack of population-based data. An estimated 300,000 U.S. children have arthritis, including 100,000 with a form of JIA. Oligoarthritis is the most common subtype (40–50%), followed by polyarthritis (25–30%) and systemic JIA (5–15%) (see Table 180.4 ). There is no sex predominance in systemic JIA ( sJIA ), but more girls than boys are affected in both oligoarticular (3 : 1) and polyarticular (5 : 1) JIA. The peak age at onset is 2-4 yr for oligoarticular disease. Age of onset has a bimodal distribution in polyarthritis, with peaks at 2-4 yr and 10-14 yr. sJIA occurs throughout childhood, with a peak at 1-5 yr.
The etiology and pathogenesis of JIA are not completely understood, although both immunogenetic susceptibility and an external trigger are considered necessary. Twin and family studies suggest a substantial role for genetic factors. JIA is a complex genetic trait in which multiple genes may affect disease susceptibility. Variants in major histocompatibility complex (MHC) class I and class II regions have indisputably been associated with different JIA subtypes. Non-HLA candidate loci are also associated with JIA, including polymorphisms in the genes encoding protein tyrosine phosphatase nonreceptor 22 (PTPN22), tumor necrosis factor (TNF)-α, macrophage inhibitory factor, interleukin (IL)-6 and its receptor, and IL-1α. Possible nongenetic triggers include bacterial and viral infections, enhanced immune responses to bacterial or mycobacterial heat shock proteins, abnormal reproductive hormone levels, and joint trauma.
JIA is an autoimmune disease associated with alterations in both humoral and cell-mediated immunity. T lymphocytes have a central role, releasing proinflammatory cytokines favoring a type 1 helper T lymphocyte response. Studies of T-cell receptor expression confirm recruitment of T lymphocytes specific for synovial non–self-antigens. B-cell activation, immune complex formation, and complement activation also promote inflammation. Inheritance of specific cytokine alleles may predispose to upregulation of inflammatory networks, resulting in systemic disease or more severe articular disease.
Systemic JIA is characterized by dysregulation of the innate immune system with a lack of autoreactive T cells and autoantibodies. It therefore may be more accurately classified as an autoinflammatory disorder , more like familial Mediterranean fever, than the other subtypes of JIA. This theory is also supported by work demonstrating similar expression patterns of a phagocytic protein (S100A12) in sJIA and familial Mediterranean fever, as well as the same marked responsiveness to IL-1 inhibitors.
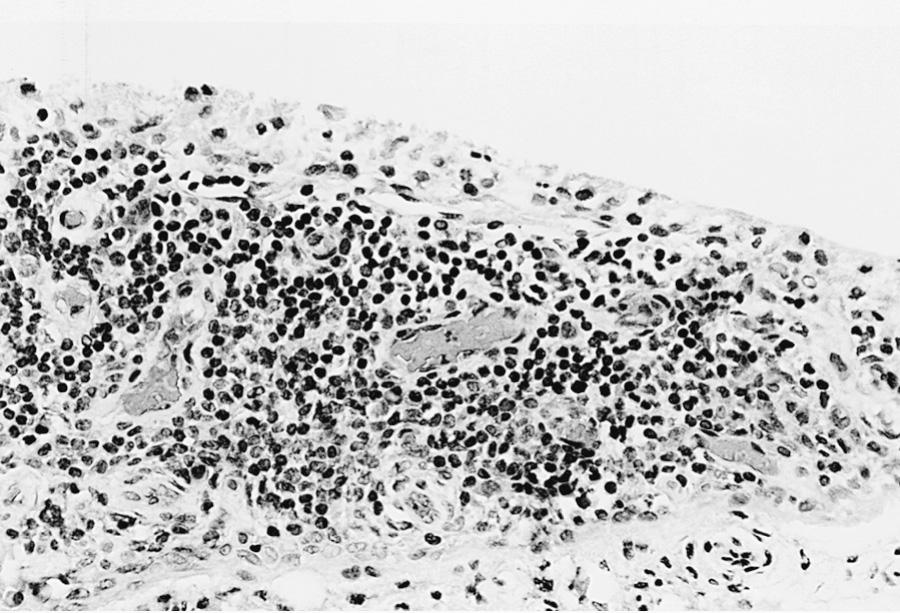
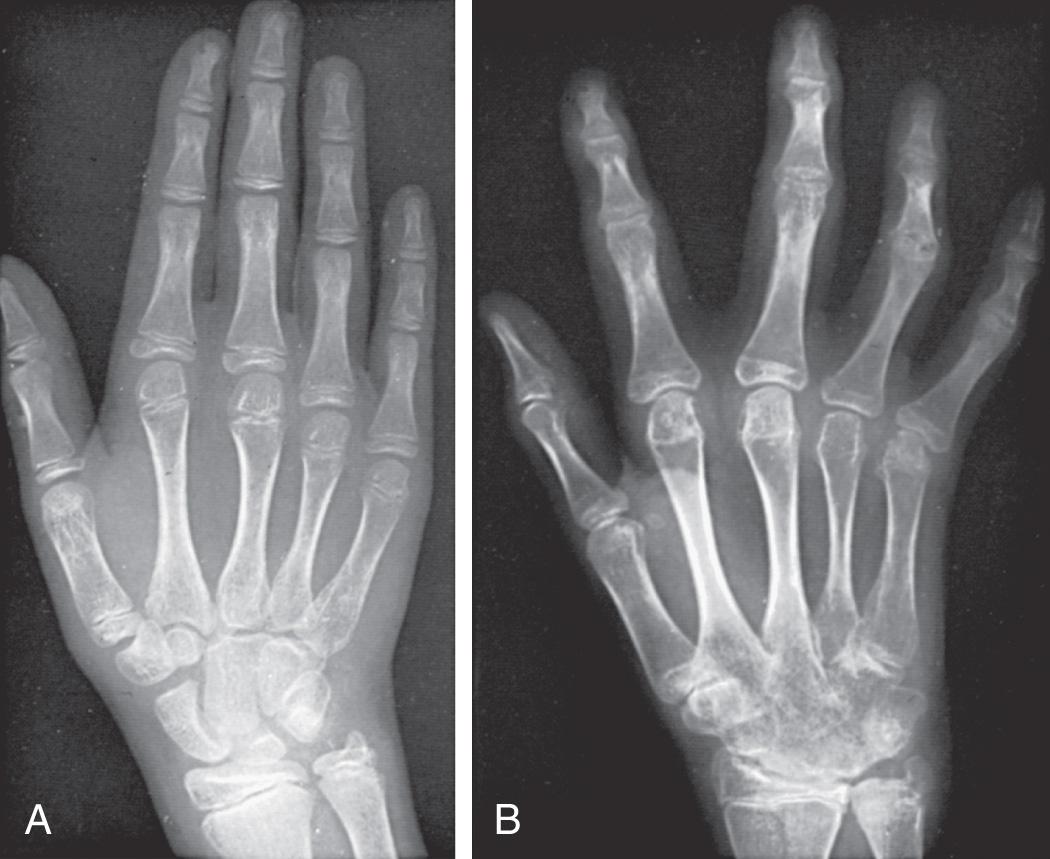
All these immunologic abnormalities cause inflammatory synovitis, characterized pathologically by villous hypertrophy and hyperplasia with hyperemia and edema of the synovial tissue. Vascular endothelial hyperplasia is prominent and is characterized by infiltration of mononuclear and plasma cells with a predominance of T lymphocytes ( Fig. 180.1 ). Advanced and uncontrolled disease leads to pannus formation and progressive erosion of articular cartilage and contiguous bone ( Figs. 180.2 and 180.3 ).


Arthritis must be present ≥6 wk to make a diagnosis of any JIA subtype. Arthritis is defined by intraarticular swelling or the presence of ≥2 of the following signs: limitation in range of motion (ROM), tenderness or pain on motion, and warmth. Initial symptoms may be subtle or acute and often include morning stiffness with a limp or gelling after inactivity. Easy fatigability and poor sleep quality may be present. Involved joints are often swollen, warm to touch, and uncomfortable on movement or palpation with reduced ROM, but usually are not erythematous. Arthritis in large joints, especially knees, initially accelerates linear growth and causes the affected limb to be longer, resulting in a discrepancy in limb lengths. Continued inflammation stimulates rapid and premature closure of the growth plate, resulting in shortened bones.
Oligoarthritis is defined as involving ≤4 joints within the 1st 6 mo of disease onset, and often only a single joint is involved (see Table 180.4 ). It predominantly affects the large joints of the lower extremities, such as the knees and ankles ( Fig. 180.4 ). Isolated involvement of upper-extremity large joints is less common. Those in whom disease never develops in >4 joints are regarded as having persistent oligoarticular JIA , whereas evolution of disease in >4 joints after 6 mo changes the classification to extended oligoarticular JIA and is associated with a worse prognosis. Isolated involvement of the hip is almost never a presenting sign and suggests ERA (see Chapter 181 ) or a nonrheumatic cause. The presence of a positive antinuclear antibody (ANA) test confers increased risk for asymptomatic anterior uveitis, requiring periodic slit-lamp examination ( Table 180.5 ). ANA positivity may also be correlated with younger age at disease onset, female sex, asymmetric arthritis, and fewer involved joints over time.

| Referral | |
|
|
| Initial screening examination | |
|
|
|
|
| Ongoing screening | |
|
|
|
|
| Oligoarticular JIA, psoriatic arthritis, and enthesitis-related arthritis irrespective of ANA status, onset under 11 yr | |
| AGE AT ONSET (YR) | LENGTH OF SCREENING (YR) |
| <3 | 8 |
| 3-4 | 6 |
| 5-8 | 3 |
| 9-10 | 1 |
| Polyarticular, ANA-positive JIA, onset <10 yr | |
| AGE AT ONSET (YR) | LENGTH OF SCREENING (YR) |
| <6 | 5 |
| 6-9 | 2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
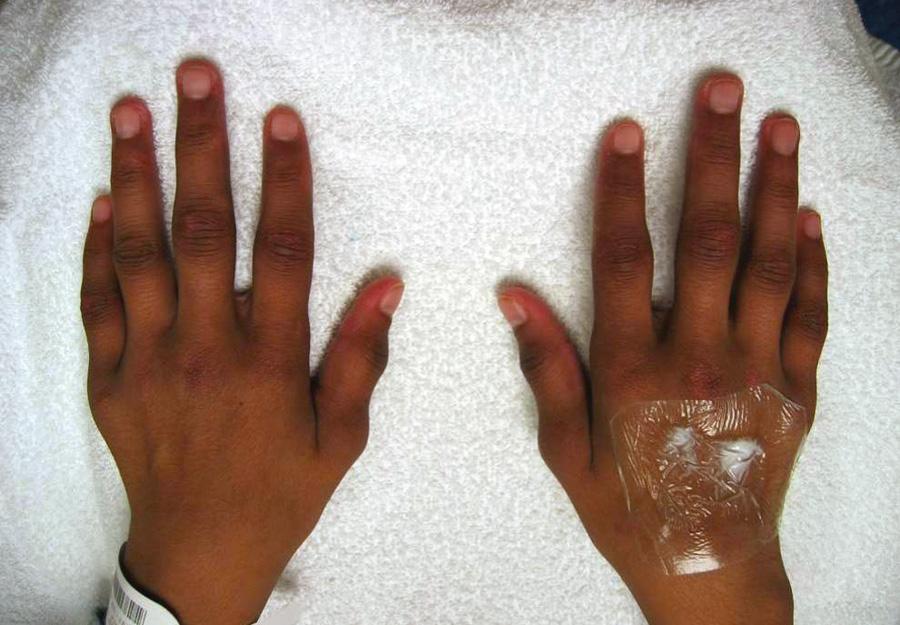
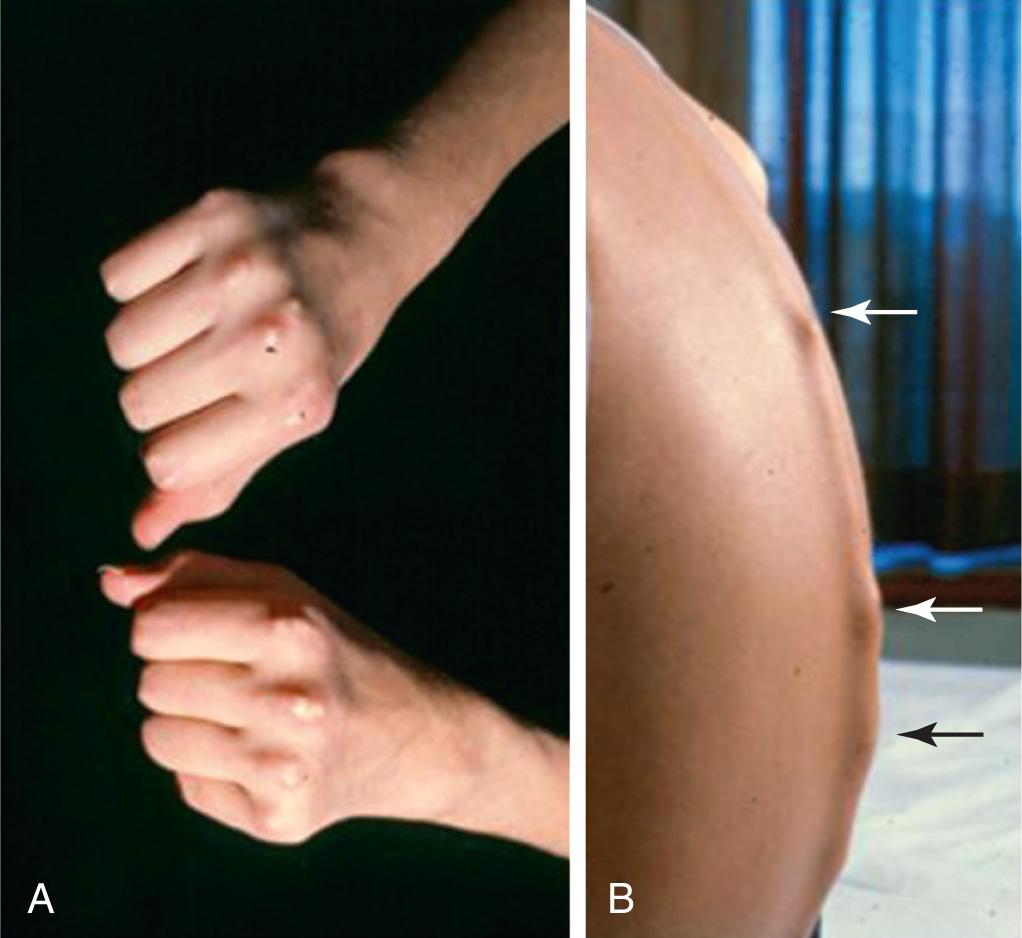
Polyarthritis is characterized by inflammation of ≥5 joints in both upper and lower extremities ( Figs. 180.5 and 180.6 ). Rheumatoid factor (RF)–positive polyarthritis resembles the characteristic symmetric presentation of adult rheumatoid arthritis. Rheumatoid nodules on the extensor surfaces of the elbows, spine, and over the Achilles tendons, although unusual, are associated with a more severe course and almost exclusively occur in RF-positive individuals ( Fig. 180.7 ). Micrognathia reflects chronic temporomandibular joint disease ( Fig. 180.8 ). Cervical spine involvement ( Fig. 180.9 ), manifesting as decreased neck extension, occurs with a risk of atlantoaxial subluxation and neurologic sequelae. Hip disease may be subtle, with findings of decreased or painful ROM on examination ( Fig. 180.10 ).



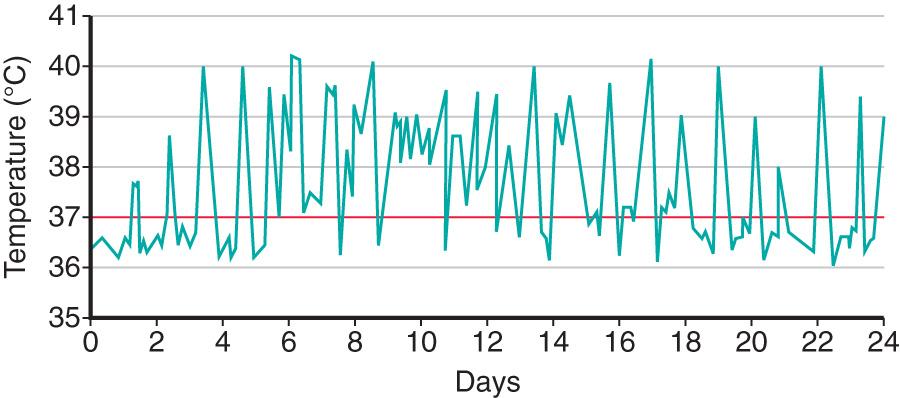
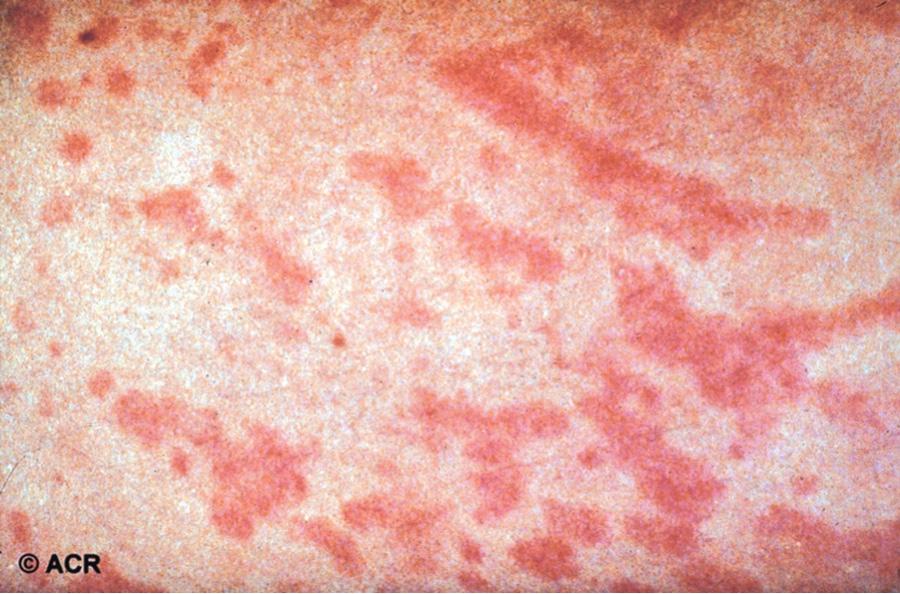
Systemic JIA is characterized by arthritis, fever, rash, and prominent visceral involvement, including hepatosplenomegaly, lymphadenopathy, and serositis (pericarditis). The characteristic fever, defined as spiking temperatures to ≥39°C (102.2°F), occurs on a daily or twice-daily basis for at least 2 wk, with a rapid return to normal or subnormal temperatures ( Fig. 180.11 ). The fever is often present in the evening and is frequently accompanied by a characteristic faint, erythematous, macular rash. The evanescent salmon-colored lesions, classic for sJIA, are linear or circular and are usually distributed over the trunk and proximal extremities ( Fig. 180.12 ). The classic rash is nonpruritic and migratory with lesions lasting <1 hr. Koebner phenomenon , a cutaneous hypersensitivity in which classic lesions are brought on by superficial trauma, is often present. Heat can also evoke rash. Fever, rash, hepatosplenomegaly, and lymphadenopathy are present in >70% of affected children. Without arthritis, the differential diagnosis includes the episodic fever (autoinflammatory) syndromes (see Chapter 188 ), infection (endocarditis, rheumatic fever, brucellosis), other rheumatic disorders (SLE, vasculitis syndromes, serum sickness, Kawasaki disease, sarcoidosis, Castleman disease), inflammatory bowel disease, hemophagocytic syndromes, and malignancy. Some children initially present with only systemic features and evolve over time, but definitive diagnosis requires presence of arthritis. Arthritis may affect any number of joints, but the course is classically polyarticular, may be very destructive, and can include hip, cervical spine, and temporomandibular joint involvement.
Macrophage activation syndrome (MAS) is a rare but potentially fatal complication of sJIA that can occur at any time (onset, medication change, active or remission) during the disease course. It is also referred to as secondary hemophagocytic syndrome or hemophagocytic lymphohistiocytosis (HLH) (see Chapter 534.2 ). There is increasing evidence that sJIA/MAS and HLH share similar functional defects in granule-dependent cytotoxic lymphocyte activity. In addition, sJIA-associated MAS and HLH share genetic variants in approximately 35% of patients with sJIA/MAS. MAS classically manifests as acute onset of high-spiking fevers, lymphadenopathy, hepatosplenomegaly, and encephalopathy. Laboratory evaluation shows thrombocytopenia and leukopenia with elevated liver enzymes, lactate dehydrogenase, ferritin, and triglycerides. Patients may have purpura and mucosal bleeding, as well as elevated fibrin split product values and prolonged prothrombin and partial prothromboplastin times. The erythrocyte sedimentation rate (ESR) falls because of hypofibrinogenemia and hepatic dysfunction, a feature useful in distinguishing MAS from a flare of systemic disease ( Table 180.6 ). An international consensus panel developed a set of classification criteria for sJIA-associated MAS, including hyperferritinemia (>684 ng/mL) and any 2 of the following: thrombocytopenia (≤181 × 10 9 /L), elevated liver enzymes (aspartate transaminase >48 U/L), hypertriglyceridemia (>156 mg/dL), and hypofibrinogenemia (≤360 mg/dL) ( Table 180.6 ). These criteria apply to a febrile patient suspected of sJIA and in the absence of disorders such as immune-mediated thrombocytopenia, infectious hepatitis, familial hypertriglyceridemia or visceral leishmaniasis. A relative change in laboratory values is likely more relevant in making an early diagnosis than are absolute normal values . A bone marrow aspiration and biopsy may be helpful in diagnosis, but evidence of hemophagocytosis is not always evident. Emergency treatment with high-dose intravenous methylprednisolone, cyclosporine, or anakinra may be effective. Severe cases may require therapy similar to that for primary HLH (see Chapter 534.2 ).
* From Ravelli A, Grom A, Behrens E, Cron R: Macrophage activation syndrome as part of systemic juvenile idiopathic arthritis: diagnosis, genetics, pathophysiology and treatment, Genes Immun 13:289–298, 2012.
Cytopenias
Abnormal liver function tests
Coagulopathy (hypofibrinogenemia)
Decreased erythrocyte sedimentation rate
Hypertriglyceridemia
Hyponatremia
Hypoalbuminemia
Hyperferritinemia
Elevated sCD25 and sCD163
Nonremitting fever
Hepatomegaly
Splenomegaly
Lymphadenopathy
Hemorrhages
Central nervous system dysfunction (headache, seizures, lethargy, coma, disorientation)
Macrophage hemophagocytosis in the bone marrow aspirate
Increased CD163 staining of the bone marrow
† From Ravelli A, Minoia F, Davì S, et al: 2016 Classification criteria for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials Organisation collaborative initiative, Arthritis Rheumatol 68:566-576, 2016.
Serum ferritin >684 ng/mL and
Any 2 of the following:
Thrombocytopenia (≤181 × 10 9 /L)
Elevated liver enzymes (aspartate transaminase >48 U/L)
Hypertriglyceridemia (>156 mg/dL)
Hypofibrinogenemia (≤360 mg/dL)
Bone mineral metabolism and skeletal maturation are adversely affected in children with JIA, regardless of subtype. Children with JIA have decreased bone mass (osteopenia), which appears to be associated with increased disease activity. Increased levels of cytokines such as TNF-α and IL-6, both key regulators in bone metabolism, have deleterious effects on bone within the joint as well as systemically in the axial and appendicular bones. Abnormalities of skeletal maturation become most prominent during the pubertal growth spurt.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here