Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Rotator cuff pathology is commonly encountered in an orthopedic practice and can result in significant pain and dysfunction. The prevalence of rotator cuff tears in the general population is reported to be between 9.7% and 62%, and increases with age. Varkey et al. reported 397,116 Medicare patients underwent rotator cuff repair between 2005 and 2012. REFERENCE: Varkey et al JSES 2016 http://dx.doi.org/10.1016/j.jse.2016.05.001 . The majority of these cases are now performed arthroscopically, given advancements in instrumentation, improved technique, and the advantages over open techniques, which include less soft tissue disruption and an improved ability to treat concomitant pathology. Although arthroscopic repair has been shown to yield excellent outcomes in the hands of an experienced surgeon, there is a learning curve, as well as potential preoperative, intraoperative, and postoperative pitfalls.
The overall morbidity of arthroscopic RCR is low compared with other orthopedic procedures; however, there are a number of complications that can occur and have lasting consequences for patients. These complications can be categorized as occurring intraoperatively or postoperatively and may be secondary to patient-related factors or to surgical technique. This chapter aims to discuss possible complications in arthroscopic RCR. An awareness of potential issues allows surgeons to develop improved practices to avoid these pitfalls, recognize problems when they arise, and be prepared to treat issues in an evidenced based manner. Moreover, in an era of shared decision making, real data about the risks of complications after arthroscopic RCR allow the patients to be better informed about the risks of their procedure.
One of the most important factors in avoiding complications is careful and thoughtful patient selection. This includes a robust understanding of the indications for arthroscopic RCR, an assessment of the patient’s risk for undergoing a surgical procedure, and consideration as to whether the pathology can be addressed with the arthroscopic skill that a particular surgeon may possess. Attempting to arthroscopically fix a rotator cuff tear in a patient with advanced rotator cuff tear arthropathy, insufficient quality tissue for repair, advanced fatty infiltration/atrophy, or operating on a medically unstable patient may lead to failure. Although beyond the scope of this chapter, the proper indications should be carefully studied, and surgery should be undertaken when there is a high likelihood of success. Choosing the appropriate procedure in the appropriate patient is of the utmost importance. A preoperative discussion involving appropriate expectations and the risks and benefits of both operative and nonoperative management is critical to allow patients to participate in the decision-making process.
Several patient-related factors have been reported to affect rotator cuff tendon healing, and should be considered. A recent study showed that smoking adversely affected healing failure after arthroscopic RCR. Hyperlipidemia has been identified as a risk factor for retear after arthroscopic RCR. In addition, sustained hyperglycemia was shown to impair tendon–bone healing after RCR in a rodent model, and a higher rate of complications has been noted in the diabetic population. Modification of serum cholesterol levels and blood glucose levels may play a role in improving healing after repairs. Multiple studies have demonstrated inferior clinical outcomes in patients with worker’s compensation claims. , This specific patient population has overall lower clinical outcome scores and a higher rate of noncompliance, which should be factored into decision making.
Most intraoperative problems can be minimized through careful preoperative planning and meticulous operative technique. Some of the common intraoperative issues a surgeon can encounter during RCR are discussed in this section.
Beach chair and lateral decubitus are the most commonly used positions for arthroscopic RCR. Although the preponderance of evidence has not shown any clear superiority in terms of set-up, visualization, or portal placement, there are certain advantages and disadvantages to each. The beach chair position, particularly when a limb positioner is used, allows the surgeon to rotate and position the arm without an assistant to facilitate access for anchor placement and visualization. There are data demonstrating a higher incidence of cerebral desaturation–related effects when in the beach chair position; however, recent studies have shown that this is safe position for shoulder surgery. , The risk of cerebral desaturation may be related to the position of the head and intraoperative management of blood pressure. , The patient’s blood pressure should be closely monitored on the contralateral arm at the level of the heart to avoid errors in pressure measurement, which can potentially produce possible serious complications related to perfusion, including stroke or death. In some centers, a cerebral oximeter has also been used for real-time monitoring of cerebral perfusion, and may be a useful adjunct. Traction injuries specific to the lateral decubitus position may occur from distraction of the extremity. Pressure-related injuries may also be seen in the lateral position, and can be avoided by use of an axillary role and careful padding of the down extremities. Complications innate to general anesthesia may be minimized by careful patient medical optimization preoperatively. Patients with medical comorbidities or prior issues with anesthesia may benefit from a preoperative appointment with anesthesia and/or their primary care provider for medication optimization and anesthetic planning. Regional anesthesia has been shown to be a highly effective adjunct in shoulder surgery, but also carries a low risk of neurovascular injury. The use of multimodal anesthesia, including an interscalene block, may be useful to decrease opioid consumption in shoulder surgery.
Especially in chronic retracted rotator cuff tears, mobilization of the rotator cuff tissue to appropriately cover the footprint may be challenging. In our experience, a significant number of massive and retracted rotator cuff tears seen on magnetic resonance imaging may be amenable to primary repair after adequate mobilization. However, in cases with a high degree of retraction (Patte 2), fatty infiltration (Goutallier 4), macerated tissue, and a large or massive tear pattern according to the Cofield classification, the patient should be consented for alternative procedures such as patch augmentation, superior capsule reconstruction, tendon transfer, or reverse total shoulder arthroplasty ( Table 30.1 ). Critical assessment of the preoperative imaging will allow the surgeon to have the proper instrumentation and implants readily available to quickly transition to another procedure if needed.
| Patte Classification | |
| Stage 1 | Proximal stump close to bony insertion |
| Stage 2 | Proximal stump at level of humeral head |
| Stage 3 | Proximal stump at glenoid level |
| Goutallier Classification | |
| Stage 0 | Normal muscle |
| Stage 1 | Some fatty streaks |
| Stage 2 | <50% fatty muscle atrophy |
| Stage 3 | 50% fatty muscle atrophy |
| Stage 4 | >50% fatty muscle atrophy |
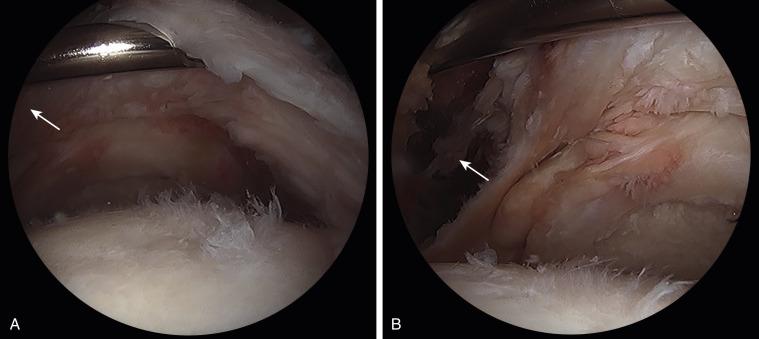
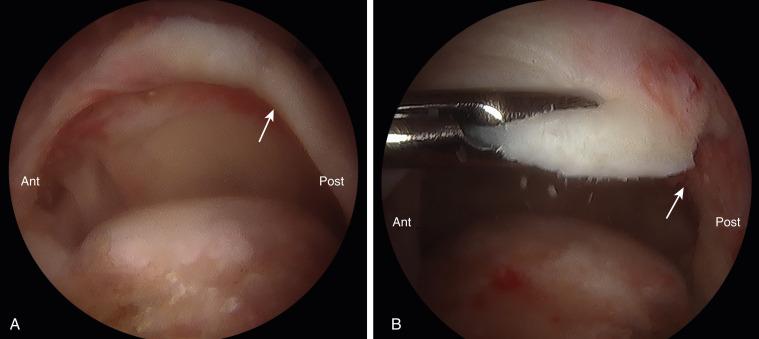
In cases of massive retracted tears, visualization is paramount to allow for proper mobilization. We typically use four portals (posterior, anterior, anterolateral, posterolateral). After the subacromial bursectomy is performed and the tear is visualized, traction can be applied by pulling the arm downward in a slightly forward flexed and abducted position to increase the subacromial space, yielding an improved view. An arthroscopic tissue grasper or a traction suture can be used to test the tissue excursion and maintain traction while releasing scar tissue. Adhesions must be carefully released in both the subacromial space and intraarticular space on the underside of the cuff to allow full mobilization. The coracohumeral ligament can be released to improve excursion of the supraspinatus ( Fig. 30.1 ), and in certain cases a posterior interval slide ( Fig. 30.2 ) can be of utility. Awareness of the anatomy of the suprascapular nerve (SSN) is essential to avoid damage while performing the releases. The surgeon should be prepared to perform extensive releases and arthroscopic mobilization; however, if the tissue will not fully reduce to the footprint, being prepared with appropriate grafts for a patch augmentation or superior capsular reconstruction is essential. Advanced preparation will allow for the completion of a procedure in one setting rather than requiring a return to the operating room and separate anesthetic. In cases where the surgeon does not have experience with a grafting procedure, the patient can be treated with a debridement and partial repair.
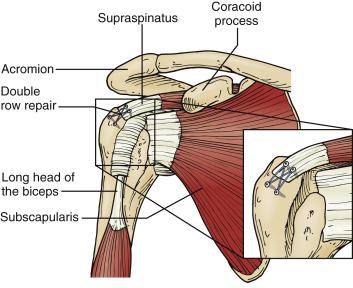
Anchor pull-out is rare with modern suture anchor designs; however, when the bone is soft, inadequate purchase can be a problem. We typically use 4.75-mm suture anchors and a punch to assess the bone quality. In cases where the bone is soft, we either will change to a smaller punch (most cases) or place a larger (5.5-mm) suture anchor. Suture anchors should be placed in the proximal and middle parts of the greater tuberosity (rather than distal) to improve load to failure. Double-row fixation using linked constructs also dissipates the force and decreases the risk of anchor failure. In cases where the bone quality is so poor that anchor fixation is impossible to achieve, transosseus repair techniques using cortical augmentation may be considered as well.
The so called “deadman-angle” of suture anchor insertion has been reported to improve pull-out strength and minimize total tension across the sutures. , Other studies have recommended a 90-degree angle of insertion for improved fixation. It is clear that the loading direction and placement of the suture anchor play a role in the performance of the suture anchor suture complex. Moreover, the depth of the anchor is important because Bynum et al. found that the varying the depth of suture anchor insertion changes the mechanical properties and mode of failure of suture anchor constructs. These results were consistent with other data demonstrating that deeper placement of suture anchors for increased purchase caused greater displacement and was not recommended. The best location to place an anchor at is the articular margin or the lateral cortex of the tuberosity. A linked double-row construct can optimize placement of anchors in these positions with tension shared across each of the anchors. We prefer to use a double-row linked construct, to insert the anchors perpendicular to the bone, and to insert the anchor to a depth flush with the bone ( Fig. 30.3 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here