Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Primary sclerosing cholangitis (PSC) is a chronic cholestatic liver disease of unknown cause. This disease has a typical onset from 20 to 30 years of age but may begin in childhood; it has a 2:1 male-to-female predilection. PSC is commonly associated with inflammatory bowel disease, particularly ulcerative colitis. In patients with ulcerative colitis, 3% to 7.5% have or will develop PSC. The term primary is used even when there is associated ulcerative colitis because there is no convincing evidence that PSC is caused by or is secondary to inflammatory bowel disease. Other associated conditions include sicca complex, Riedel’s struma, retroperitoneal fibrosis, and mediastinal fibrosis. , Patients with PSC also have an increased risk for cholangiocarcinoma, with a lifetime risk of 10% to 15%.
Approximately 25% of patients with PSC are asymptomatic at presentation. Clinical features of PSC include fatigue, pruritus, jaundice, right upper quadrant pain, and hepatosplenomegaly. Elevations of serum bilirubin concentration and serum aspartate transaminase activity are usually not as marked or as consistent as increased serum alkaline phosphatase activity. There is strong evidence that genetic and immunologic factors are important in the pathogenesis of PSC. There is no specific serologic marker for PSC. ,
The natural history of PSC is variable but usually progressively downhill, with a 5-year survival of 88% and a median survival of 11.9 years from the time of diagnosis. No known therapy, short of liver transplantation, has been proved effective.
Whereas findings from liver biopsy may be compatible with PSC, they alone are not diagnostic. In general, the diagnostic criteria for PSC should include the following: typical radiographic appearance of cholangiographic abnormalities; appropriate clinical, biochemical, and histologic findings obtained from liver biopsy; and exclusion of secondary causes of sclerosing cholangitis. Of these, typical radiographic cholangiographic abnormalities are crucial for the diagnosis of PSC.
Although features of PSC can be demonstrated on a variety of imaging modalities, the most important and most characteristic radiographic findings are seen at fluoroscopic cholangiography ( Fig. 51.1 ). Fluoroscopic cholangiography is usually accomplished by endoscopic retrograde cholangiopancreatography (ERCP).
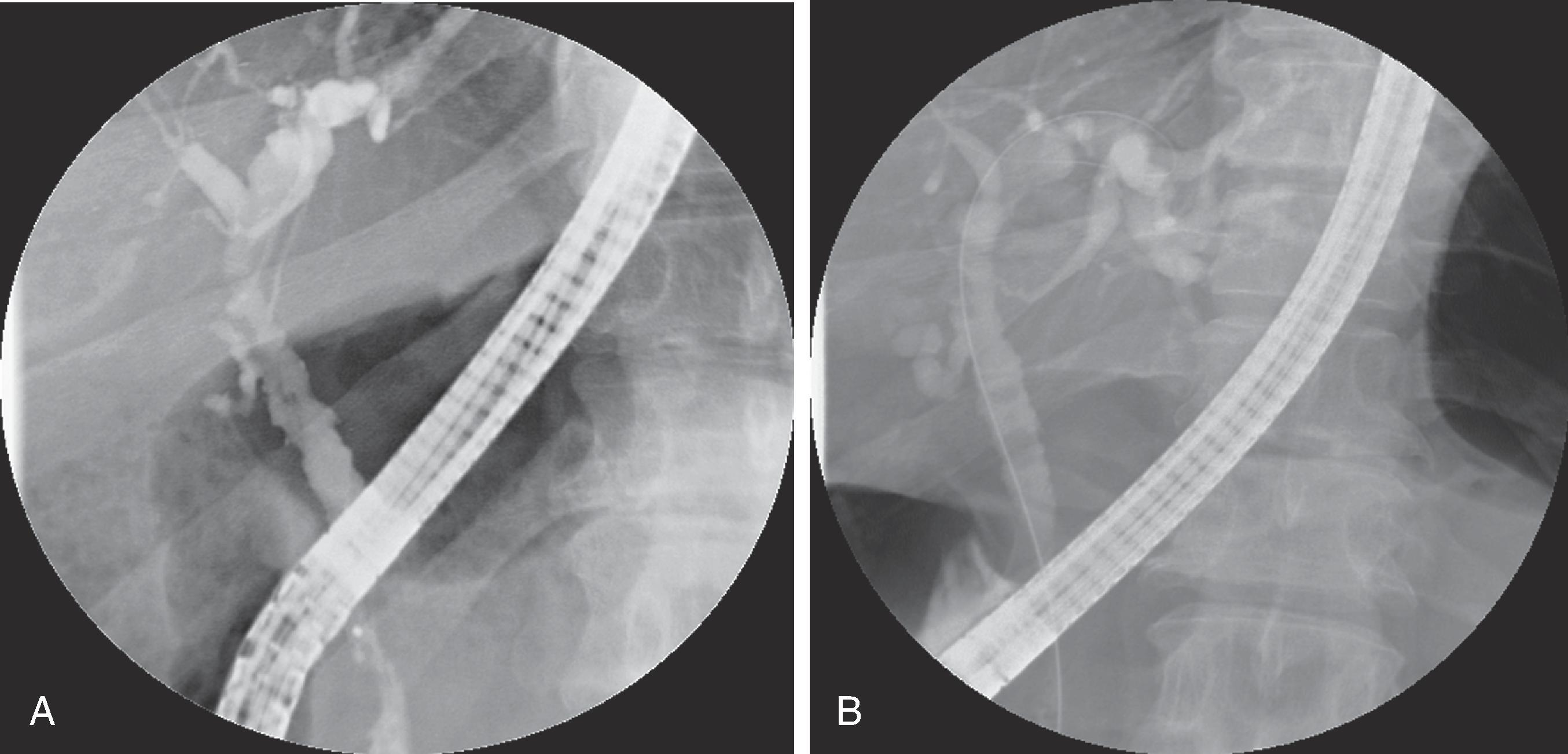
Multiple segmental strictures involving both the intrahepatic and extrahepatic bile ducts are the hallmark of PSC. The fluoroscopic cholangiographic findings in PSC depend on the stage of the disease process. Random segments of the biliary tree may be involved by periductal inflammation and fibrosis. In the early phases of PSC, normal or less involved duct segments may alternate with segmental strictures, producing the classic beaded appearance. Stricture length can vary from 1 to 2 mm (so-called band strictures) to several centimeters; the most common length is 1 to 1.5 cm. Strictures usually occur at the bifurcation of bile ducts and are out of proportion to upstream ductal dilation. When the periductal fibrosis worsens, the bile ducts take on a “pruned tree” appearance that reflects peripheral duct obliteration. In addition, the angles formed with the central ducts become more obtuse.
Almost half of patients with PSC have some degree of ductal mural irregularity varying from a fine, brush-border appearance to a coarse, shaggy, or frankly nodular appearance. Characteristic diverticular outpouchings, varying in size from 1 to 2 mm to 1 cm, are seen in a minority of patients on high-quality cholangiograms. The combined findings of short strictures, beading, pruning, diverticula, and mural irregularities often result in a composite cholangiographic appearance that is nearly pathognomonic for PSC.
Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) are common first-line imaging tests for abnormal liver function. These modalities can assess for the presence of biliary tract abnormalities. Cross-sectional imaging allows evaluation of not only the bile duct but also the bile duct wall and the surrounding liver parenchyma. In patients with PSC, cross-sectional imaging allows detection of complications such as cirrhosis and malignant disease.
Because ultrasound is relatively inexpensive and can effectively evaluate the biliary system, it is commonly the initial imaging modality used in the evaluation of cholestatic liver disease. Findings of PSC by ultrasound evaluation include duct dilation and wall thickening of the common bile duct or the intrahepatic ducts. The normal intrahepatic bile ducts have a wall thickness of less than 1 mm and appear sonographically as a thin echogenic line. Thickened bile ducts appear as two parallel echogenic lines with a central hypoechoic stripe. Bile duct wall thickening in PSC usually measures 2 to 5 mm. Common bile duct wall thickening, when present, is easily seen at ultrasound. However, intrahepatic bile duct wall thickening may be subtle and not always readily apparent.
With ever-improving technology, CT scanning continues to serve as one of the primary imaging modalities for the evaluation of abdominal disease. Multidetector CT scanners allow rapid acquisition of data and the creation of high-resolution reformatted images for the evaluation of the biliary system, sometimes referred to as CT cholangiography. CT cholangiography allows cross-sectional imaging of the biliary tree with multiplanar reformations in patients who are unable to undergo MRI.
CT findings of PSC are similar to ERCP findings and include segmental intrahepatic biliary duct dilations with focal constrictions ( Fig. 51.2 ). The common hepatic duct and common bile duct can also demonstrate alternating narrowing and dilation. Mural contrast enhancement of the extrahepatic bile ducts can be seen, although this is a nonspecific finding that can be seen with other causes of cholangitis. Intrahepatic bile duct calculi are present in approximately 8% of patients with PSC. These calculi appear as foci of faint high attenuation or as coarse calcifications and are best seen on non–contrast-enhanced images. Upper abdominal lymphadenopathy is frequently seen in patients with PSC, although this is nonspecific. The presence of lymphadenopathy does not necessarily indicate the development of cholangiocarcinoma and should not be regarded as an exclusion criterion for liver transplantation.
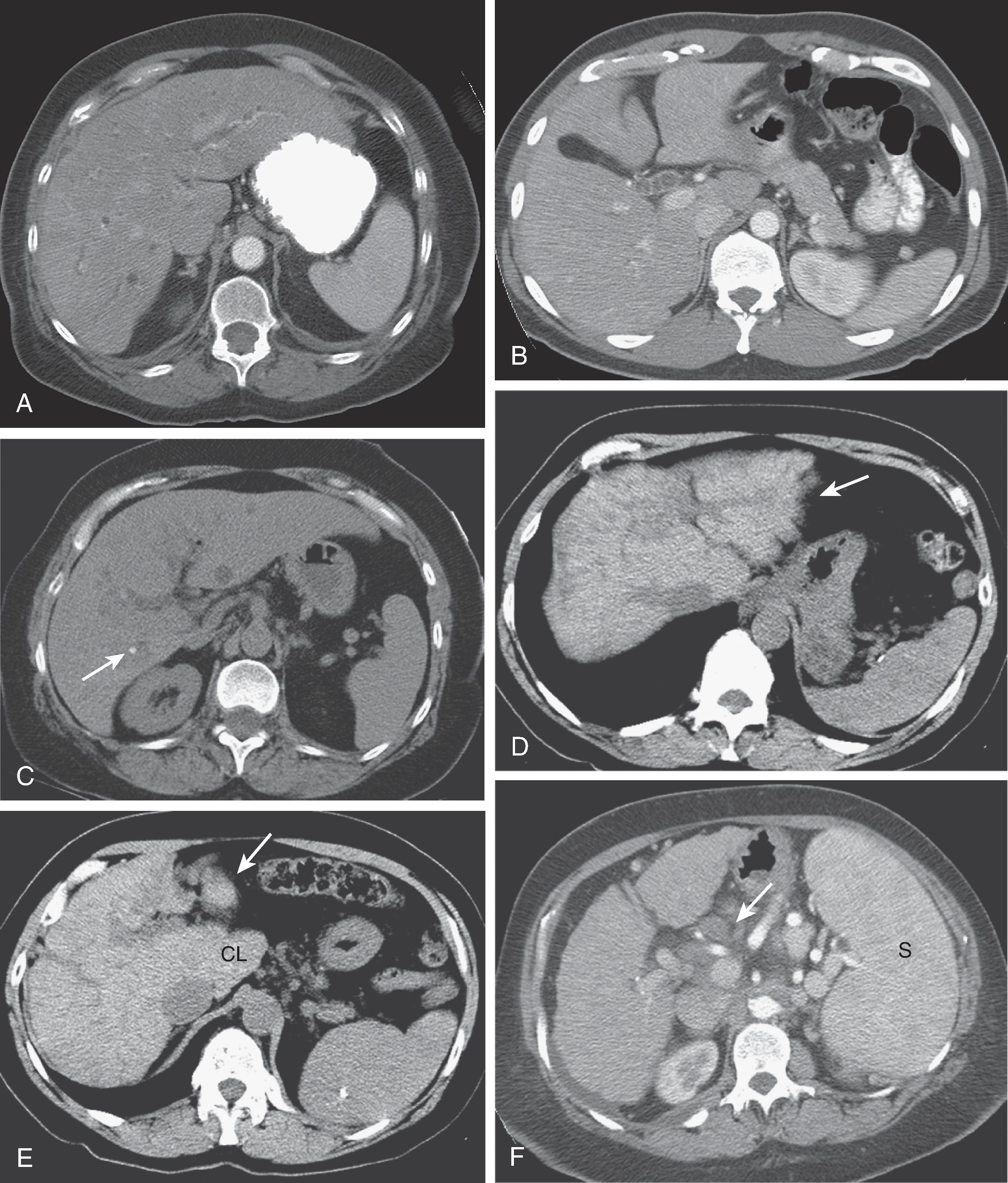
There are unique hepatic morphologic changes associated with PSC-induced cirrhosis that can be seen with CT. The liver is markedly deformed with severe contour lobulations, creating an organ that appears rounded. This is due to atrophy of both the posterior segment of the right hepatic lobe and the lateral segment of the left lobe and marked hypertrophy of the caudate lobe. In addition, the atrophied right hepatic lobe may be hypodense (due to fibrosis) relative to the hypertrophied caudate lobe, creating the effect of a pseudotumor. When these morphologic changes are seen in conjunction with scattered, dilated intrahepatic bile ducts and intrahepatic bile duct stones, PSC can be suggested as the cause of the cirrhosis. There is substantial overlap in the appearance of livers affected by cirrhosis due to PSC and those affected by end-stage cirrhosis caused by the usual factors (alcohol and hepatitis).
Introduced in 1991, magnetic resonance cholangiopancreatography (MRCP) is a technique that uses heavily T2-weighted pulse sequences to depict the bile and pancreatic ducts. MRCP is noninvasive and does not require the use of iodinated contrast material or ionizing radiation. Studies have shown good correlation between MRCP and ERCP in the diagnosis of PSC. MRCP findings of PSC are similar to ERCP findings and include multifocal segmental strictures alternating with normal or slightly dilated bile duct segments ( Fig. 51.3 ). The strictures are usually out of proportion to the degree of upstream ductal dilation. Periductal inflammation and fibrosis prevent the ducts from dilating; therefore, high-grade strictures can be present with only minimal proximal dilation. With progressive fibrosis, the peripheral bile ducts are obliterated, resulting in a pruned tree appearance at MRCP, similar to findings at fluoroscopic cholangiography. Other findings include mural irregularities, webs, diverticula, and stones.
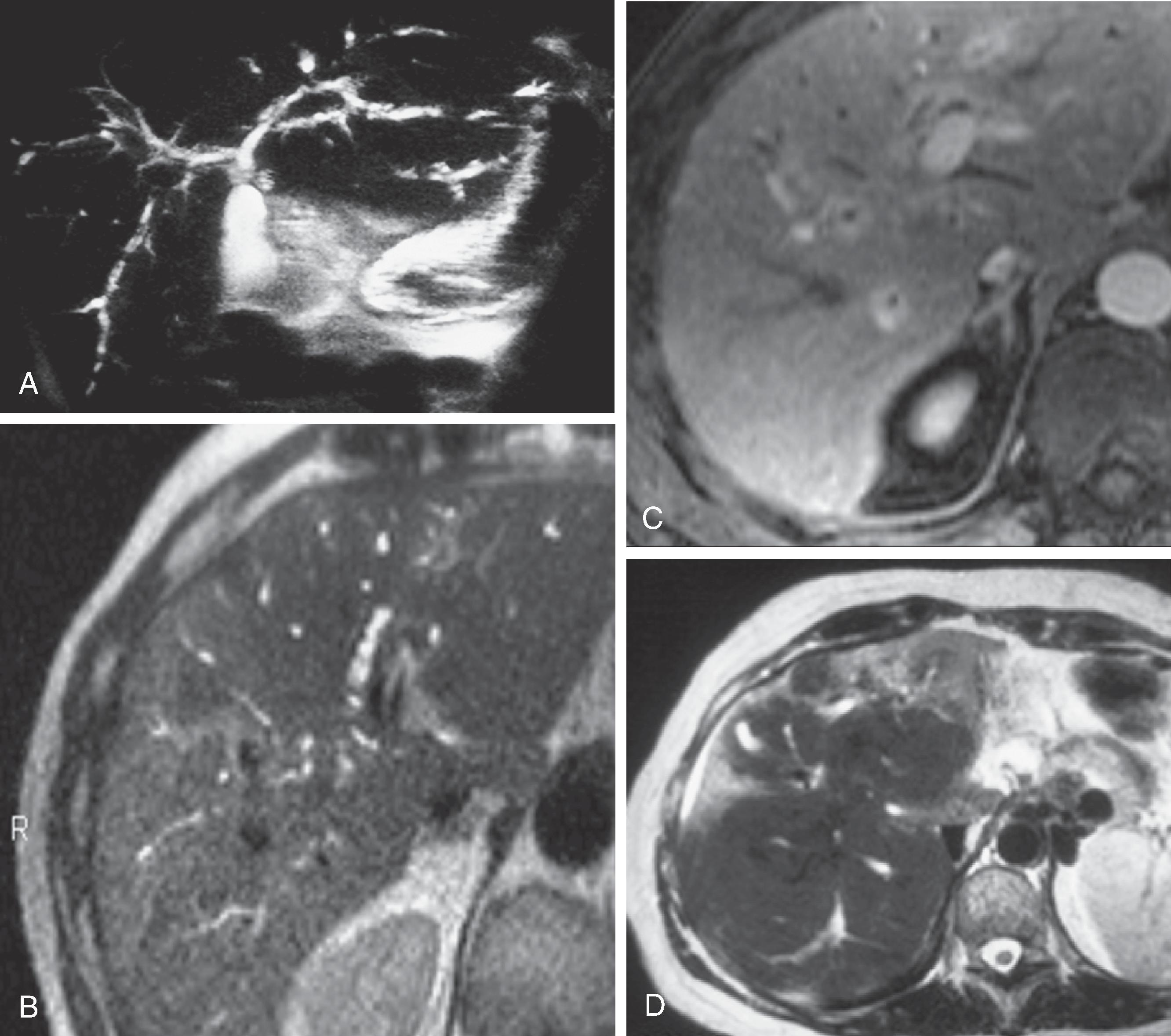
Hepatic parenchymal changes associated with PSC can be observed by MRI. Extension of the ductal inflammation into the hepatic parenchyma, retention of bile salts, and accumulation of copper in hepatocytes are thought to be responsible for the parenchymal changes seen on MRI. The extrahepatic bile duct demonstrates wall thickening (1.5 mm or more) and enhancement. On T1-weighted images, randomly distributed areas of high signal intensity can be seen in a minority of patients. This abnormal signal is assumed to be due to cholestasis and lipofuscin deposits in atrophic liver cells. T2-weighted images may demonstrate increased signal intensity in a peripheral wedge-shaped or fine reticular pattern. Extension of periductal inflammation to involve the vascular and lymphatic channels is considered to be the reason for the signal abnormality. Inflammatory changes of the hilar bile ducts result in a high T2 signal along the porta hepatis. Postcontrast images can demonstrate peripheral areas of enhancement possibly due to alterations in blood flow in response to regional inflammation.
A macronodular pattern of cirrhosis can be seen in patients with PSC. These large nodules (usually more than 3 cm) can be found predominantly within the central portion of the liver. The nodules are typically isointense on T1-weighted images and hypointense on T2-weighted images. After the administration of contrast material, the nodules are hypointense immediately after the injection and 2 minutes afterward, eventually becoming isointense. The peripheral wedge-shaped areas of parenchymal atrophy seen with PSC-induced cirrhosis are typically hypointense on T1-weighted images and hyperintense on T2-weighted images. Corresponding areas demonstrate hypoenhancement on images obtained immediately after administration of contrast material and hyperenhancement on images obtained 2 minutes afterward.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here