Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
▪ Itch mite infestation ▪ “Seven-year itch”
Human scabies is a pruritic condition caused by infestation with the host-specific mite Sarcoptes scabiei var. hominis , which lives its entire life within the epidermis
Although the scabies mite is not a known vector for any systemic disease, secondary bacterial infections with Streptococcus pyogenes or Staphylococcus aureus may develop
Transmission typically occurs via direct close contact with an infested person; fomite transmission is also possible, especially with the crusted variant
Permethrin 5% cream is currently the first-line treatment for classic scabies
The scabies mite continues to plague all countries of the world. An estimated 300 million individuals are affected. Pruritus associated with this infestation is usually severe, especially at night, and treatment requires prescription scabicidal therapy.
Scabies has been a common companion of the human species for over 2500 years .
Scabies is a worldwide problem and all ages, races, and socioeconomic groups are susceptible. Environmental factors that promote its spread include overcrowding, delayed treatment, and lack of public awareness of the condition. There is considerable variation in the prevalence of scabies, with rates in low-income countries ranging from 4% to 100% . Higher incidences occur with overcrowding related to natural disasters, wars, economic depression, and refugee camps . Scabies can be transmitted directly by close personal contact, sexual or otherwise, or indirectly via fomites. Prevalence is higher in children and people who are sexually active, and spread of the infestation among family members and other close contacts is common . The scabies mite is not a known vector for systemic disease.
Crusted scabies (formerly called Norwegian scabies) is found in individuals with compromised immune systems, such as the elderly, people infected with HIV or human T-cell lymphotropic virus type 1 (HTLV-1), and solid organ transplant recipients; it can also occur in those with decreased sensory functions and/or ability to scratch (e.g. patients with leprosy or paraplegia). These patients may experience minimal pruritus despite their infestation with a large number of mites and are highly contagious .
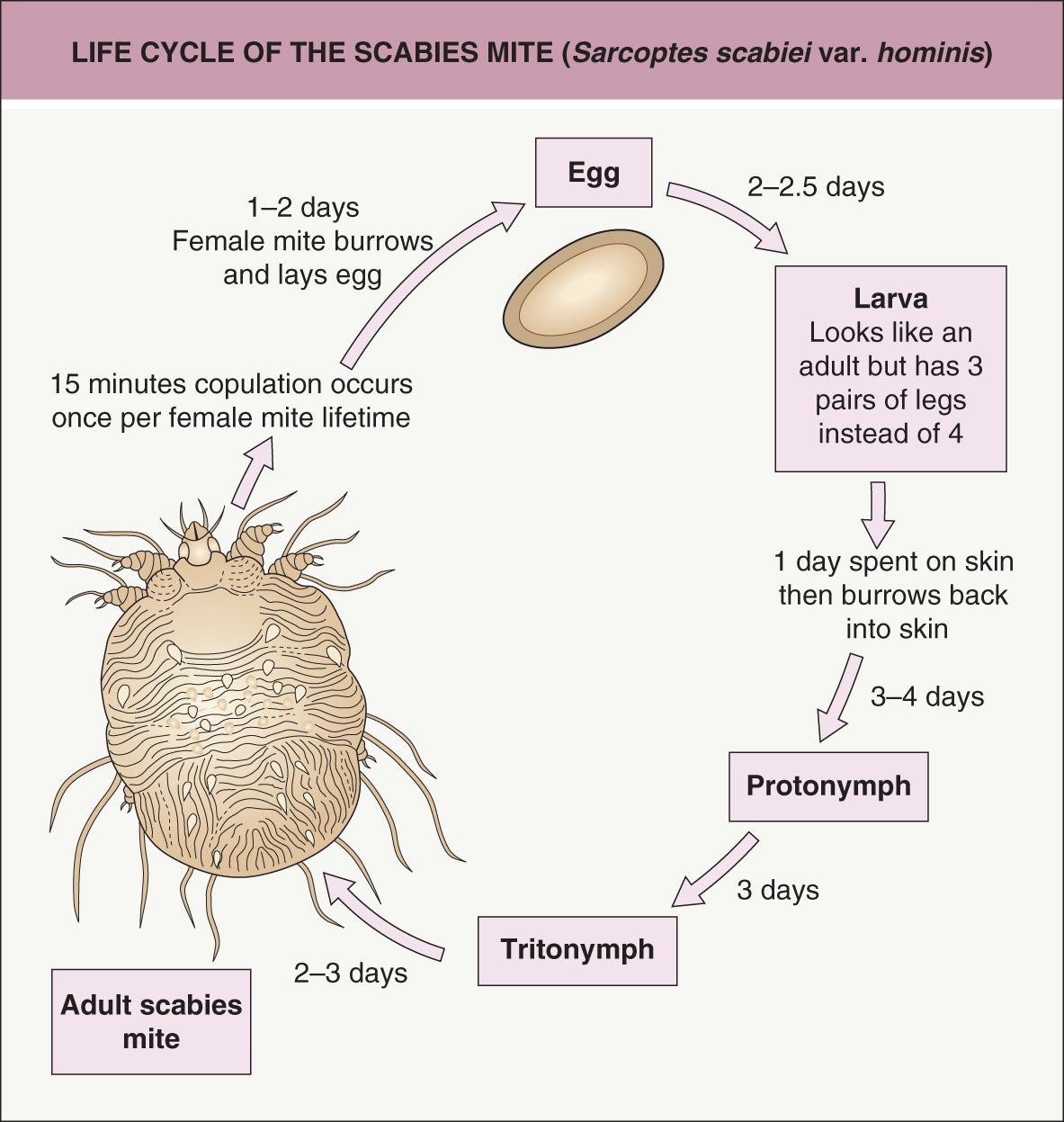
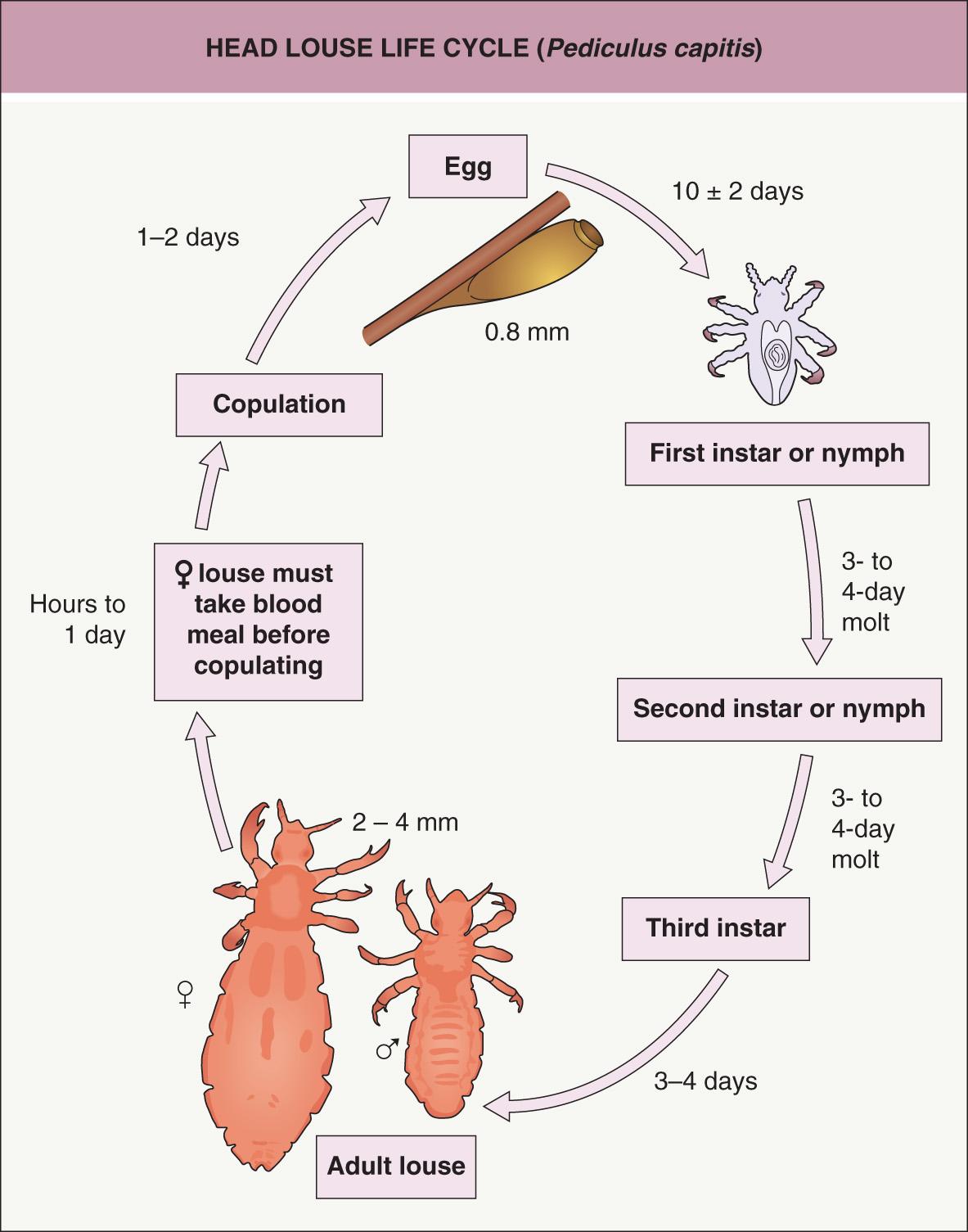
The species-specific, eight-legged mite Sarcoptes scabiei var. hominis causes human scabies ( Fig. 84.1 ). The Sarcoptes mites that cause infestations in animals (e.g. S. scabiei var. canis in dogs) are not a source of human infestation, but they can produce bite reactions (see Ch. 85 ). The scabies mite is 0.35 × 0.3 mm in size and too small to be seen by the naked eye. The entire 30-day life cycle of these mites is completed within the epidermis ( Fig. 84.2 ). Each day a female mite lays 3 eggs, which require approximately 10 days to mature. The number of mites living on an infested host can vary greatly, although there are usually fewer than a hundred and often no more than 10–15. However, patients with crusted scabies may have thousands of mites on their skin surface, and live mites can be recovered in debris from sheets, the floor, curtains, and chairs in the environment of affected individuals . Scabies mites usually live 3 days or fewer off a human host, but those from patients with crusted scabies may live up to 7 days by feeding on sloughed skin.
The incubation period before symptoms develop can range from days to months. In first-time infestations, it usually takes 2–6 weeks before the host's immune system becomes sensitized to the mite or its by-products, resulting in pruritus and cutaneous lesions. In contrast, a subsequent infestation often becomes symptomatic within 24–48 hours. Asymptomatic scabies-infested individuals are not uncommon, and they can be considered “carriers” .
The epidemiologic history (e.g. pruritus in household members or other close personal contacts), the distribution and types of lesions, and pruritus form the basis of the clinical diagnosis. The intense pruritus is classically accentuated at night and by a hot bath or shower. Pruritus may be present before any overt physical signs appear. Cutaneous lesions are symmetrical, typically involving the interdigital web spaces of the hands, flexural aspect of the wrists, axillae, posterior auricular area, waist (including the umbilicus), ankles, feet, and buttocks. In men, penile and scrotal lesions are common, while in women, the areolae, nipples, and vulvar area are often affected. In infants, the elderly and immunocompromised hosts, all skin surfaces are susceptible, including the scalp and face .
Typically, small erythematous papules are present in association with a variable degree of excoriation ( Fig. 84.3 ). Vesicles, indurated nodules, eczematous dermatitis, and secondary bacterial infection are also common. The pathognomonic sign is the burrow, representing the tunnel that a female mite excavates while laying eggs. Clinically, the burrow is wavy, thread-like, grayish-white, and 1–10 mm in length. Many patients, however, do not have obvious burrows on inspection, especially in warm climates.

Acral vesiculopustules can represent a clue to the diagnosis of scabies in infants. Crusted scabies often manifests with marked hyperkeratosis that favors acral sites including subungual areas ( Fig. 84.4 ), but involvement may be widespread. Areas of affected skin have been referred to as pachyderma. Secondary bacterial infections with Staphylococcus aureus or Streptococcus pyogenes sometimes develop. In resource-poor countries with endemic scabies, post-streptococcal glomerulonephritis is a significant issue. Peripheral eosinophilia can be the primary sign of scabies in patients with disorders of keratinization.

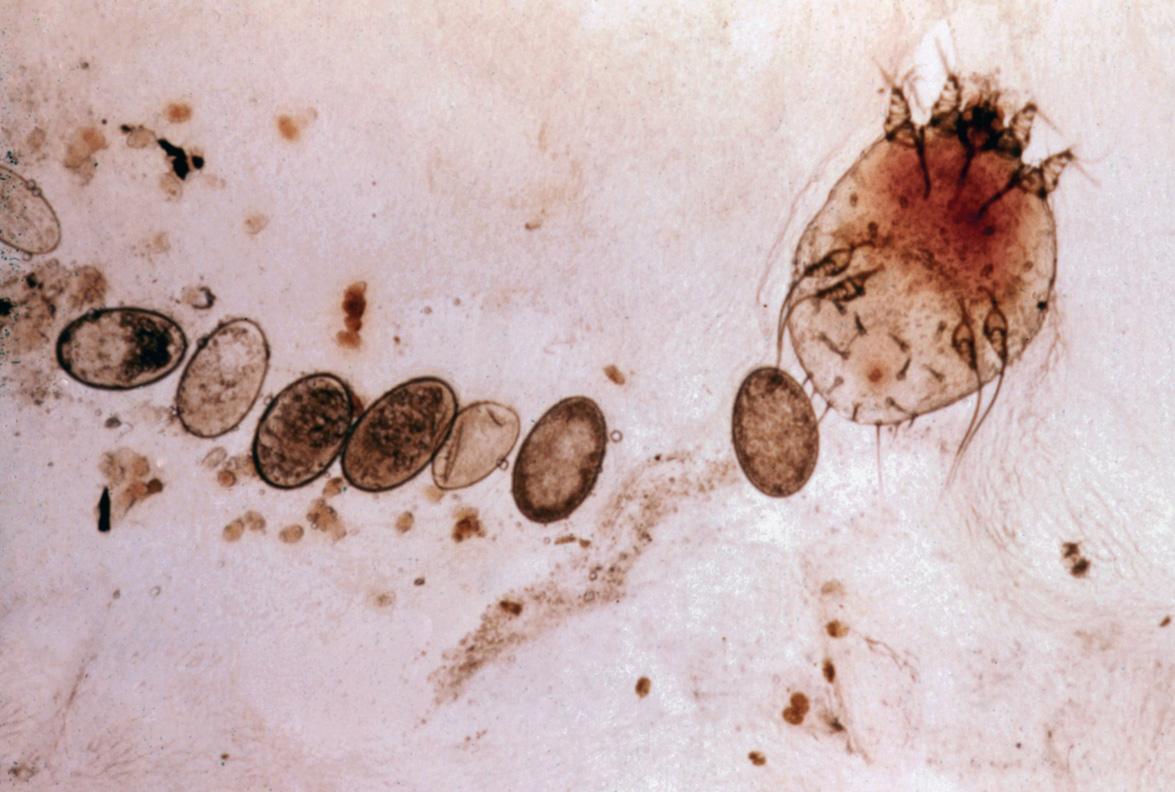
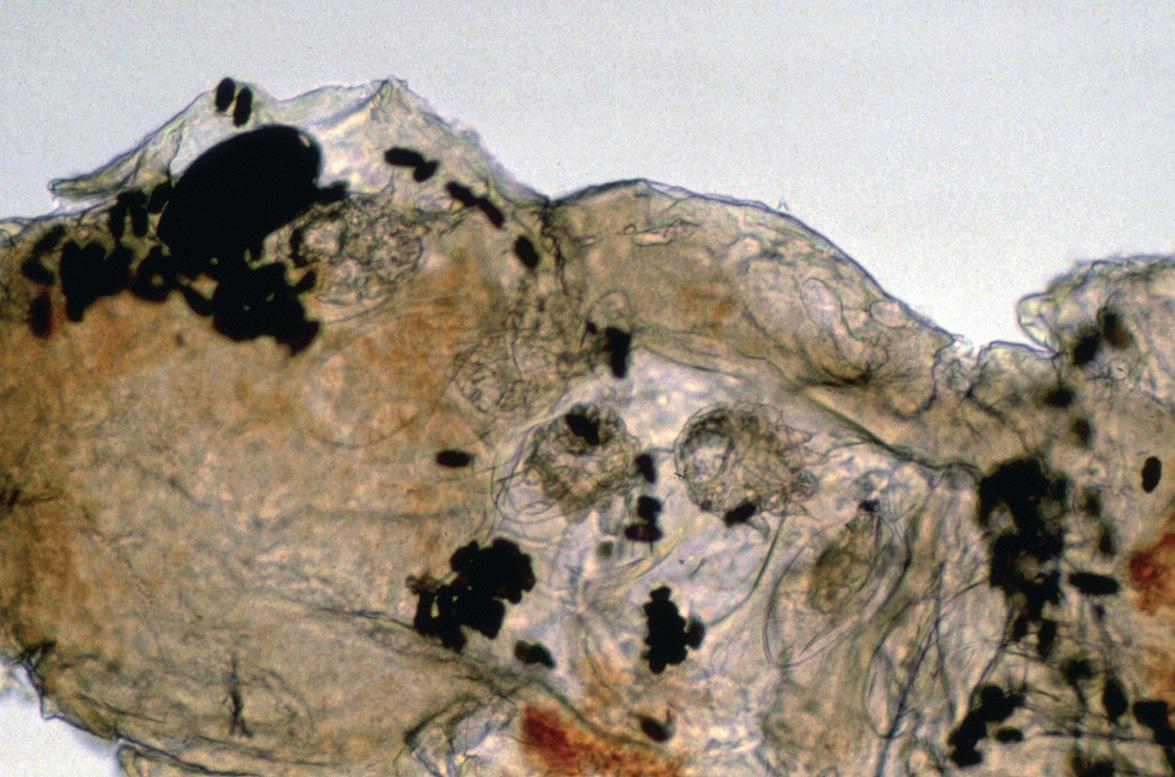
Confirmation of the diagnosis can be achieved by light microscopic examination of mineral oil preparations of skin scrapings (from infested areas) for adult mites, eggs, and/or fecal pellets (scybala; Fig. 84.5 ). A scalpel or curette may be used to obtain the skin sample . Microscopic examination of transparent adhesive tape following its application to infested areas of skin represents another diagnostic technique . Dermoscopy and confocal microscopy can prove useful for direct in vivo visualization of mites and eggs (see Fig. 0.43 ). A skin biopsy may confirm the clinical diagnosis, but only if the specimen obtained happens to contain the mite or its eggs. Often, however, the diagnosis simply rests on the clinical impression and response to treatment. The diagnostic potential of a serologic test that detects IgE specific for a recombinant S. scabiei antigen is under investigation .
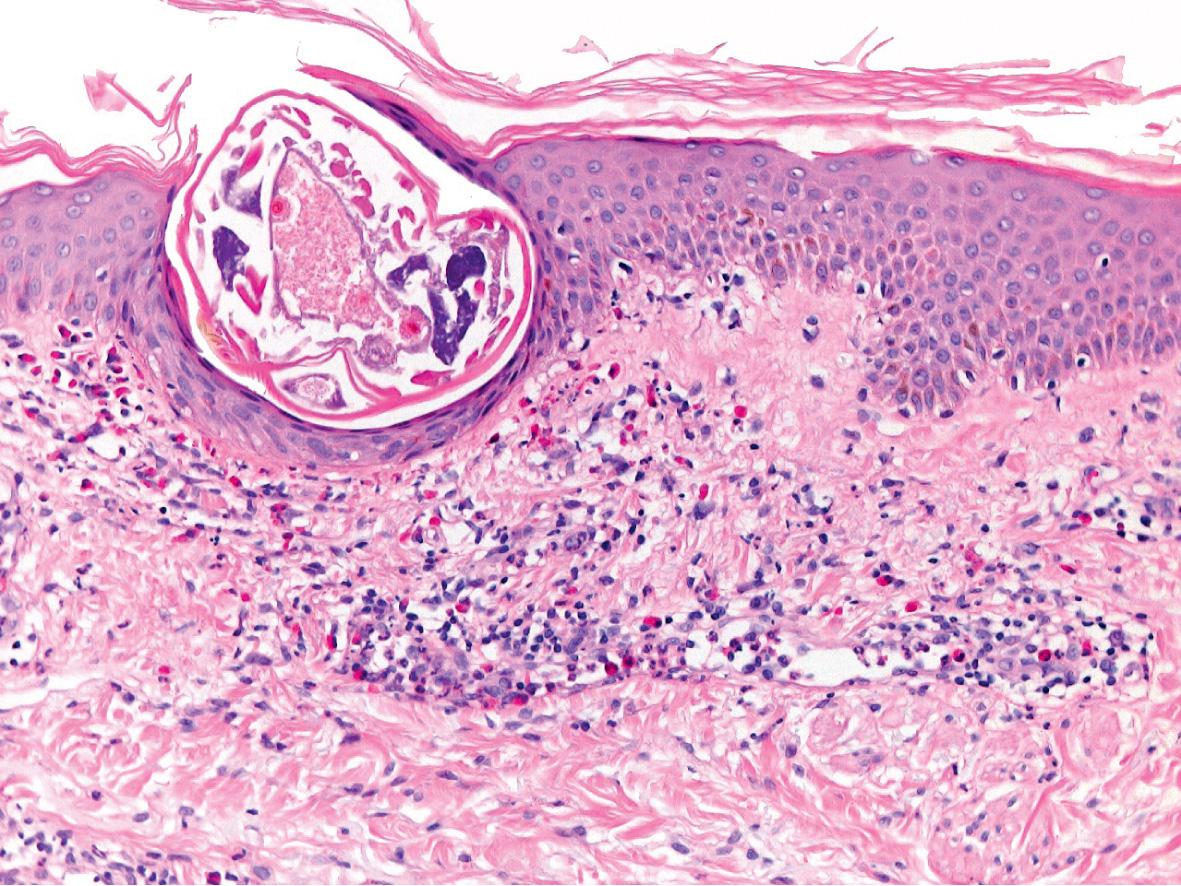
A patchy to diffuse infiltrate with prominent eosinophils as well as lymphocytes and histiocytes is noted in the reticular dermis. A transected scabies mite may occasionally be seen within the epidermis ( Fig. 84.6 ). Pink “pigtail”-like structures attached to the stratum corneum, which represent fragments of the adult mite exoskeleton, can serve as a clue to the diagnosis of scabies when entire mites, scybala, and eggs are not identified .
Unless burrows or (via dermoscopy) mites and eggs are noted clinically, a wide variety of pruritic skin diseases should be considered in the differential diagnosis. These include atopic, allergic contact, autosensitization (“id” reaction), and nummular dermatitis as well as arthropod bites, pyoderma, dermatitis herpetiformis, and bullous pemphigoid. Occasionally, scabies can mimic Langerhans cell histiocytosis clinically and histologically, as a dense infiltrate of Langerhans cells may be present. The clinical and histologic features of infantile scabies may also resemble findings in the inflammatory stage of incontinentia pigmenti. Acropustulosis of infancy can both mimic scabies and follow scabies as a hypersensitivity phenomenon.
Two topical treatments 1 week apart with a prescription antiscabetic medication are recommended ( Table 84.1 ). The topical preparation is applied overnight to the entire body surface, from head to toe, in infants and the elderly. In other age groups, the face and scalp can be excluded from treatment. Special attention should be paid to the interdigital spaces, intergluteal cleft, umbilicus, and subungual areas. To reduce the potential for reinfestation by fomite transmission, at the time of each treatment, clothing, linens, and towels used within the previous week can be either washed in hot water and dried on high heat or stored in a bag for 10 days. The relatively common occurrence of asymptomatic mite carriers in households necessitates that all family members and other close contacts be treated simultaneously, even if they have not developed any pruritus or clinical signs. Pets cannot harbor human mites and do not have to be treated. Secondary bacterial infections need to be treated with appropriate antibiotics.
| TOPICAL AND ORAL TREATMENTS FOR SCABIES | |||||
|---|---|---|---|---|---|
| Therapy | Administration | Concerns | Efficacy & resistance | Use in infants | FDA pregnancy category |
| Permethrin cream (5%) | Topically overnight on days 1 and 8 | Allergic contact dermatitis in individuals with sensitivity to formaldehyde | Good, but some signs of tolerance developing | FDA approved for infants ≥2 months of age | B |
| Lindane lotion or cream (1%) | Topically overnight on days 1 and 8 | Potential CNS toxicity, especially in individuals weighing <110 pounds (50 kg), the elderly and those with crusted scabies, other skin conditions or a history of seizures | Poor, resistance very common | Not recommended for infants, children or breastfeeding mothers; contraindicated in premature infants | C (but not recommended) |
| Crotamiton lotion or cream (10%) | Topically overnight for 3–5 days | Irritant contact dermatitis, especially in areas of denuded skin | Very poor; has antipruritic properties and may be used for postscabetic pruritus | Not established, but considered safe | C |
| Sulfur ointment (5–10%) | Topically overnight for 3 successive days | Toxicity studies not performed | Good | Not established, but considered safe | Not rated, but considered safe |
| Ivermectin (available as 3 mg tablets) | Oral dose of 200–400 mcg/kg on day 1 and repeat on day 8 or 14 * , ** | Potential CNS toxicity in infants and young children | Excellent | Safety not established for children weighing <33 pounds (15 kg) or breastfeeding mothers | C (but generally not recommended for scabies in pregnant women) |
* Administration of second dose at 2 weeks recommended by CDC ( www.cdc.gov ).
** For patients with crusted scabies who fail treatment despite appropriate environmental measures, consider both topical permethrin 5% every 2–3 days for 1 to 2 weeks and oral ivermectin (200 mcg/kg/dose) administered as three doses (days 1, 2 and 8) or as five doses (days 1, 2, 8, 9, and 15), depending upon the severity of the infection .
Following successful treatment, pruritus and skin lesions can persist for 2–4 weeks or longer, especially for acral vesiculopustules in infants and nodules. This is referred to as “postscabetic” pruritus or dermatitis. Patients should be informed that such reactions do not imply treatment failure, but rather represent the body's response to dead mites that are eventually sloughed off (within 2 weeks) along with normal epidermal exfoliation. Many patients, however, experience relief from pruritus within 3 days. The second application of topical medication is performed in order to reduce the potential for reinfestation from fomites as well as to ensure killing of any nymphs that may have survived within the semi-protective environment of the egg and subsequently hatched (see Fig. 84.2 ).
Permethrin is a synthetic pyrethroid formulated in a 5% cream that is currently the standard topical scabicide. Like other pyrethroids, it inhibits sodium transport in arthropod neurons, thereby causing paralysis. Adverse reactions are rare and are usually related to brief stinging on application. Prolonged in vitro survival of S. scabiei var. hominis following permethrin exposure has been noted, but clinical resistance has not been documented.
Lindane (gamma-hexachlorocyclohexane), an organochlorine agent, is marketed in a 1% lotion and cream. CNS side effects may occur from increased percutaneous absorption through damaged skin, misuse, overuse, or accidental ingestion. Because of the potential for CNS toxicity, lindane is contraindicated in premature infants, individuals with crusted scabies or pre-existing skin conditions (e.g. extensive atopic dermatitis) that may increase its systemic absorption, and patients with an uncontrolled seizure disorder. Worldwide, the development of lindane-resistant scabies is increasing . Potential toxicity, relatively poor efficacy, widespread resistance, and issues related to environmental contamination make lindane an inferior treatment choice compared to permethrin or ivermectin. In 2003, the US Food and Drug Administration (FDA) issued a “black box” warning for lindane products, stating that they should be used with caution in infants, children, other individuals who weigh <110 pounds (50 kg), and the elderly due to an increased risk of neurotoxicity .
An alternative scabicide is crotamiton, which is formulated in a 10% lotion and cream. Although it has an antipruritic effect, crotamiton can cause irritation of denuded skin and is less effective than the other prescription options .
Another alternative therapy for scabies is three consecutive overnight applications of 5–10% sulfur in a petrolatum base. A pharmacist must compound the medication, and toxicity studies have not been performed. Sulfur is messy, malodorous, and irritating to the skin and can stain clothing. However, its efficacy has been reported to be as high as 60–96% with three consecutive 24-hour applications .
Ivermectin is a macrocyclic lactone produced by Streptomyces avermitilis . Although not FDA-approved for scabies, ivermectin represents an effective treatment for this and other ectoparasitic infestations . By blocking transmission across nerve synapses that utilize glutamate or γ-aminobutyric acid (GABA), ivermectin causes paralysis of peripheral motor function in insects and acarines . Although GABA and glutamate are neurotransmitters within the human cerebral cortex, after early infancy, the blood–brain barrier prevents CNS penetration of the drug. Ivermectin is not recommended for children who weigh <33 pounds (15 kg), pregnant women, or breastfeeding mothers because of the lack of safety data in these groups .
In clinical studies, ivermectin has proven to be extremely safe. Over 18 million people >5 years of age have been treated annually with ivermectin in the World Health Organization (WHO) Onchocerciasis Eradication Program. An increased death rate in elderly patients who received ivermectin in a single retrospective study was determined to be causally unrelated to the medication by the WHO, medical examiners, and the scientific community.
For treatment of scabies, an oral ivermectin dose of 200–400 mcg/kg is usually administered twice, 1–2 weeks apart . Although there is only one report to date of clinical resistance to this agent by the scabies mite , increased in vitro survival times of mites exposed to ivermectin have been described in communities with a high prevalence of scabies . In areas with endemic disease, mass administration of oral ivermectin or topical permethrin can help to control scabies and reduce the prevalence of impetigo . Topical ivermectin in a 1% concentration (recently FDA-approved for the treatment of rosacea) also appears to be effective for scabies, but further study is warranted before recommending its routine use for this indication . In patients with subungual disease, addition of a topical scabicide is recommended because a systemic medication will not penetrate into thickened keratotic debris. A combination of oral ivermectin and topical permethrin is often required to treat patients with crusted scabies (see Table 84.1 ), and use of a topical keratolytic agent (e.g. salicylic or lactic acid) can help to decrease the associated hyperkeratosis.
▪ Pediculosis capitis ▪ “Cooties”
This worldwide infestation is caused by bloodsucking, wingless, six-legged insects that live only on the hairs of the scalp
Diagnosis is usually confirmed by the presence of 0.8 mm eggs (“nits”) firmly attached to scalp hairs
Head lice are spread by head-to-head contact as well as by fomite transmission
Resistance to traditional over-the-counter preparations (pyrethrins, permethrin) is growing
Newer treatments, including topical ivermectin, are now available
Lice are bloodsucking, wingless insects belonging to the suborder Anoplura. Twelve million cases per year occur in the US alone, and resistance to traditional treatments is increasing. Prescription products (e.g. topical malathion, topical or oral ivermectin) are often needed to treat resistant cases, requiring greater physician involvement.
Head lice have infested mankind for thousands of years. Nits have been found on the hair of Egyptian and Peruvian mummies .
Head lice are found worldwide with no strict limitations based upon age, sex, race, or socioeconomic class. Children 3–11 years of age have the highest incidence, with prevalences as high as 60% in some countries . Infestation with head lice is more frequent in girls, probably due to their tendency to have longer hair as well as to exchange brushes, barrettes and other hair accessories. Head lice are distinctly uncommon in African-Americans, as head lice in the US are unable to properly position themselves to lay eggs on coarse curly hair .
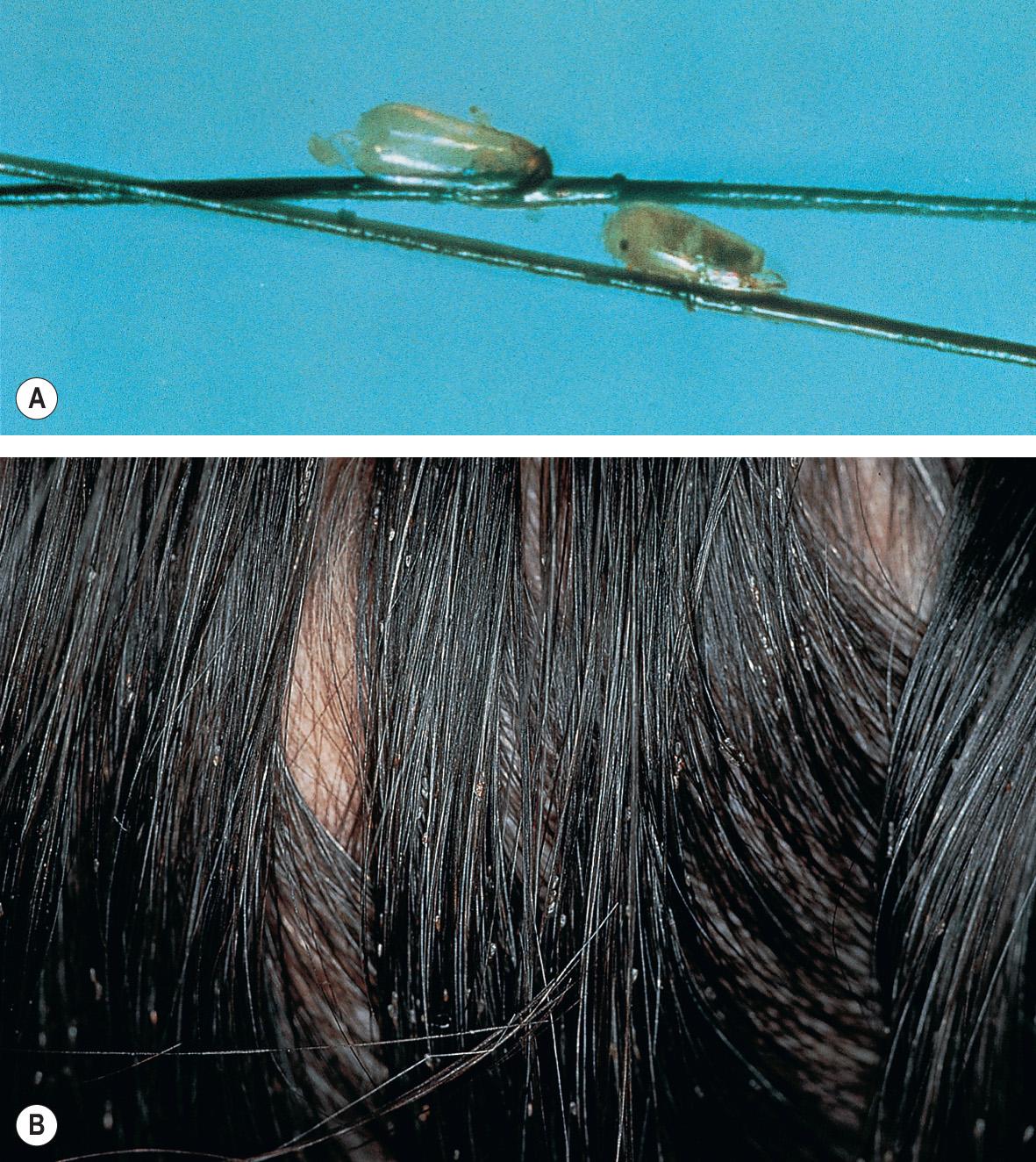
The head louse, Pediculus capitis , is a highly host-specific insect approximately the size of a sesame seed (2–3 mm; Fig. 84.7 ). These obligate human parasites feed on the blood of the host approximately every 4–6 hours. The female louse lives for 30 days, during which time she lays between 5 and 10 eggs a day on hair shafts ( Fig. 84.8 ). The oval egg capsules (nits) measure 0.8 mm in length and are usually laid close to the scalp for warmth; in general, eggs located within 1 cm of the scalp are unhatched. In warm climates, however, viable nits may be found 15 cm or more from the scalp, especially in the area above the nape of the neck. The nits are cemented to individual hairs by means of a proteinaceous matrix that closely resembles the amino acid constituents of the human hair shaft itself . Head lice rarely live for more than 36 hours away from the host without a blood meal; however, given an appropriate temperature (82–90°F/28–32°C) and level of humidity (70–90%), nits can survive and hatch after 10 days away from the host. Transmission occurs via direct head-to-head contact or by fomites such as combs, brushes, blow-dryers, hair accessories, bedding, helmets, and other headgear .

Skin findings of head lice infestation are limited to the scalp, behind the ears, and the nape of the neck. The classic symptom of intense pruritus varies among patients. It may take 2–6 weeks following an initial infestation before pruritus is evident, reflecting a delayed immunologic response to components of the lice saliva or excreta. In repeat infestations, pruritus develops within the first 24–48 hours. However, some individuals are asymptomatic “carriers”. Although excoriations, erythema, pyoderma, and scaliness of the scalp and posterior neck are common findings, definitive diagnosis is made by the identification of nits and/or adult lice on the scalp hair. Viable eggs are usually tan to brown in color, whereas hatched eggs are clear to white ( Fig. 84.9 ).
Patients occasionally present with a low-grade fever and lymphadenopathy due to a secondary bacterial infection. Head lice can carry S. aureus and Str. pyogenes on their surfaces and are a common cause of pyoderma of the scalp .
The epidermis and dermis may display nonspecific inflammation.
Although several dermatoses, such as seborrheic dermatitis and psoriasis, can cause pruritus of the scalp, the finding of nits or adult lice is diagnostic. Nits are more firmly adherent to the hair shaft than dandruff, dried hair products (e.g. sprays, gels) or hair casts, and they must be differentiated from other causes of hair shaft nodules such as piedra (white or black) and trichorrhexis nodosa (see Fig. 77.1 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here