Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Head and neck infections are extremely common in children.
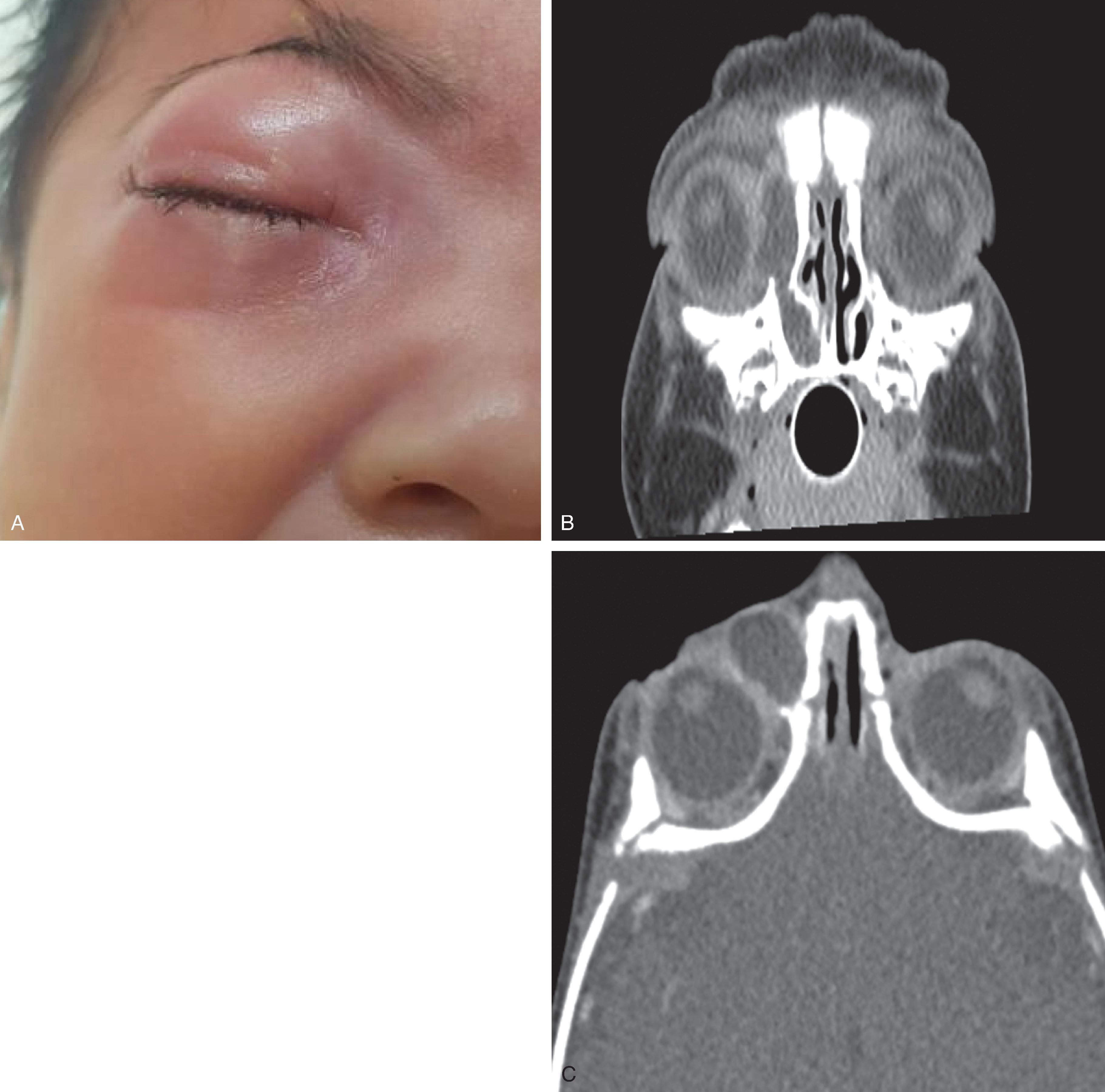
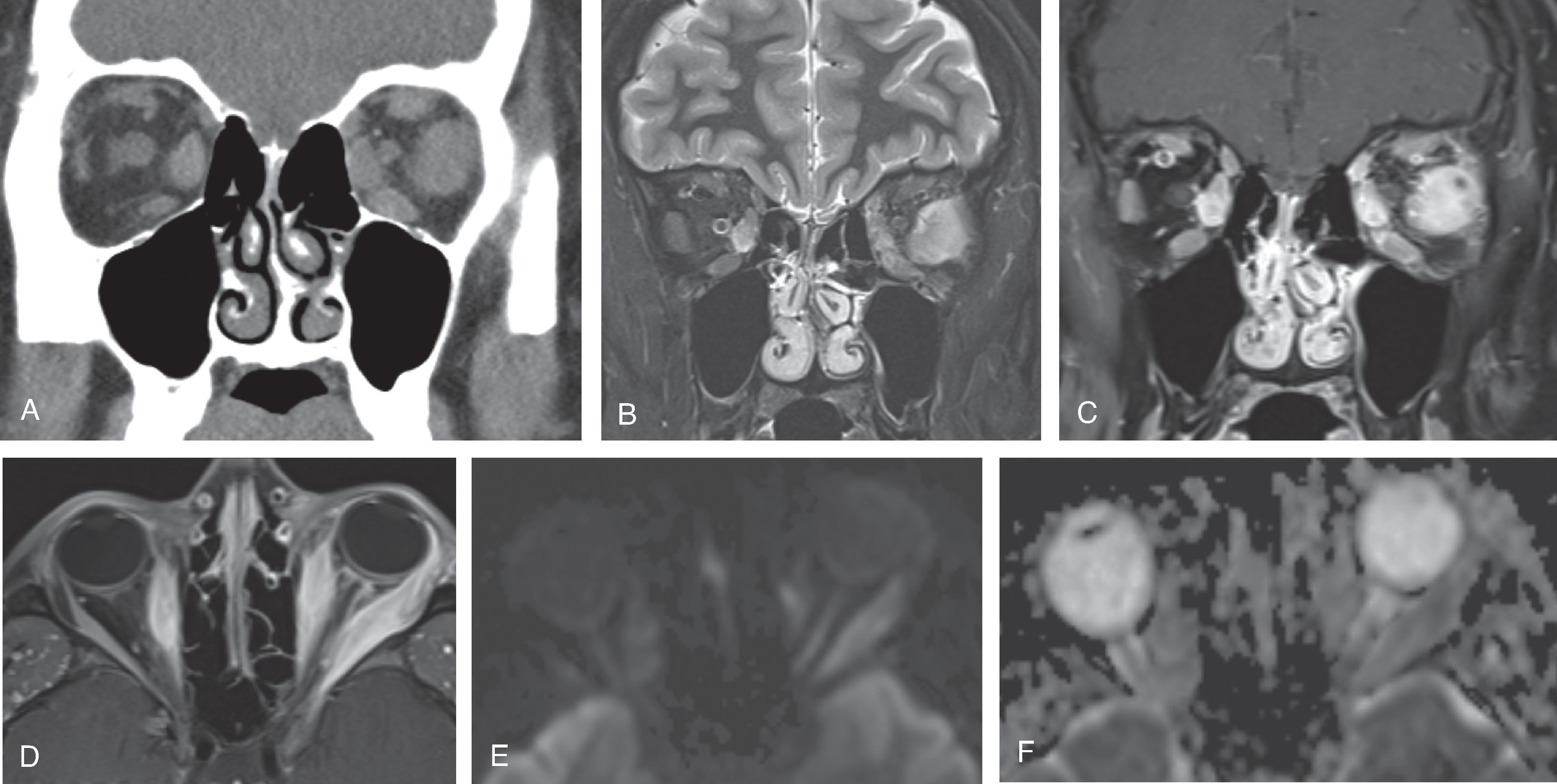
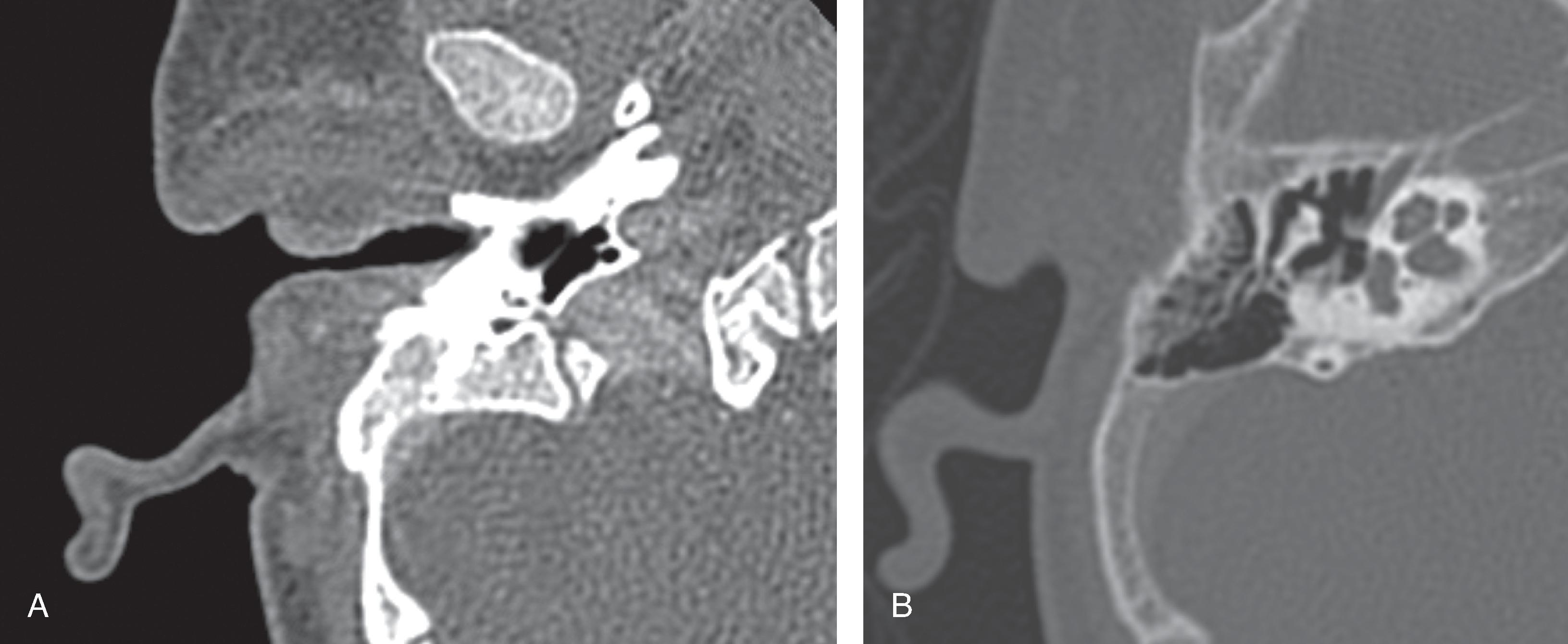
Locations of infections include the lymph nodes, salivary glands, aerodigestive tract, orbit, sinuses, and temporal bone. Consequently, an initial approach to head and neck infections and inflammatory conditions includes appropriate categorization of the anatomic site, followed by determination of extension into adjacent anatomic sites.
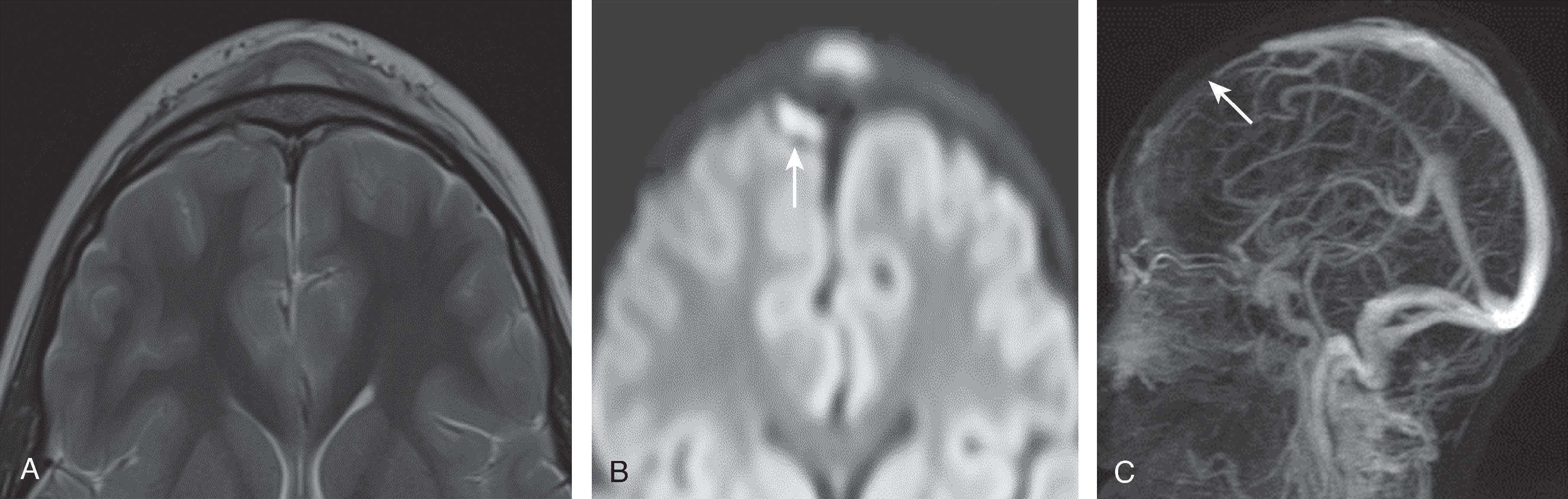
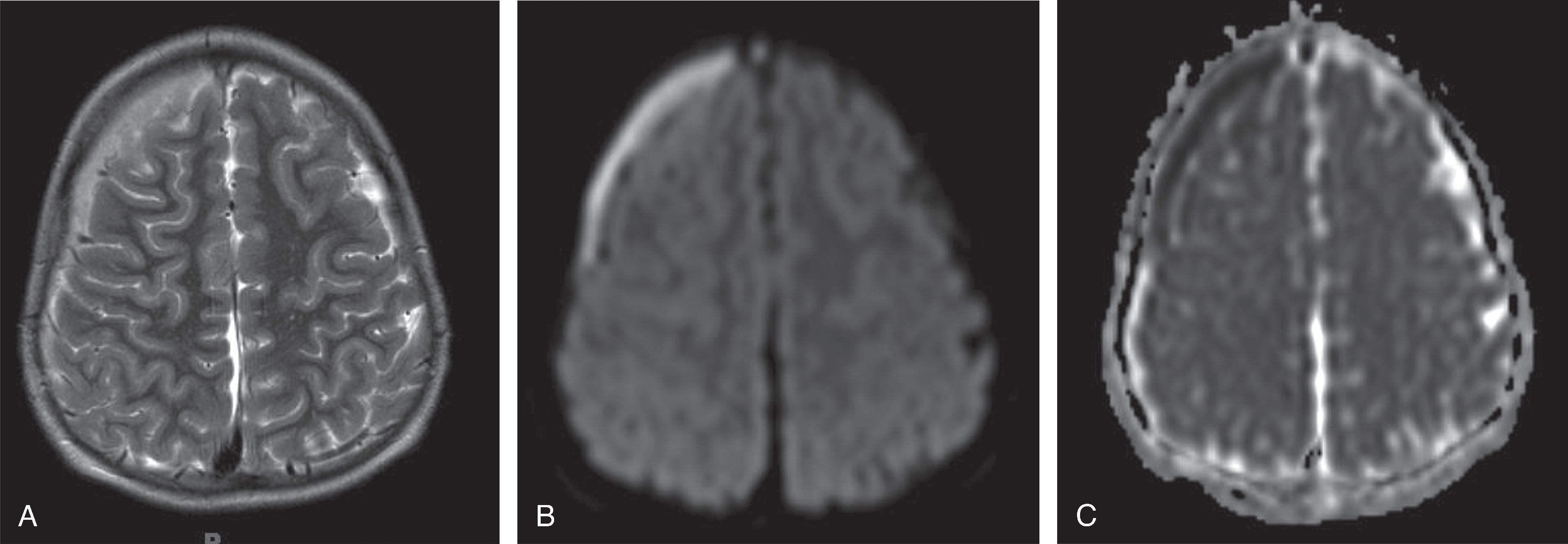
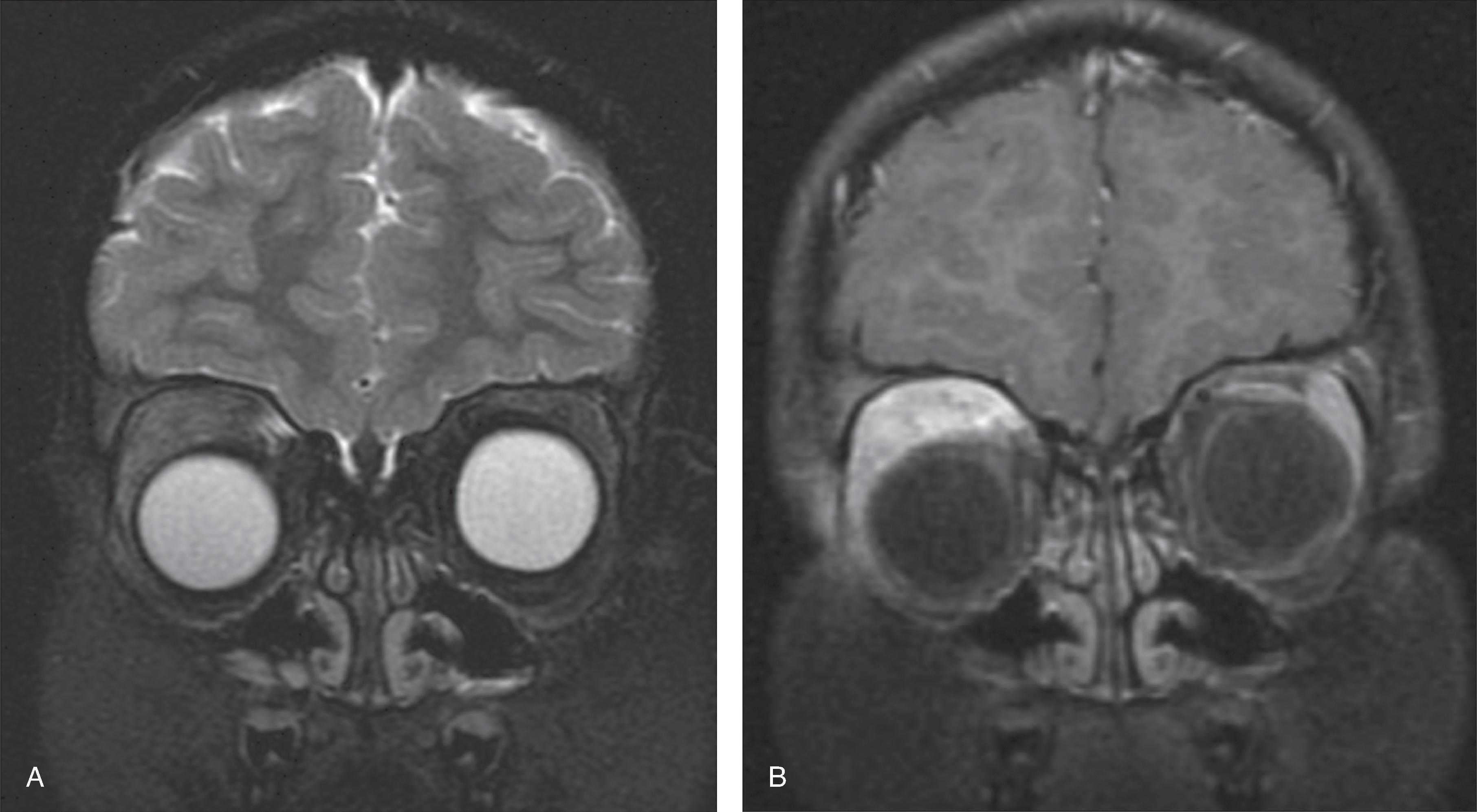
Complications from spread from one anatomical site can cause significant morbidity and mortality. In particular, infections involving the orbits, sinuses, and temporal bones have the greatest potential for intracranial spread of infection.
Imaging modalities to assess infections of the face and neck include radiographs, ultrasound, CT, and MRI. This chapter will demonstrate face and neck infection findings on these modalities.
Radiographs have a limited role, with the exception for airway infections and foreign bodies.
Ultrasound can be used for assessing for abscess and lymph nodes in the neck but has no role in evaluating infections of the sinuses and temporal bones.
Contrast-enhanced CT (CECT) imaging is often performed for infections of the neck, temporal bone, orbits, and sinuses. This is due to the fast acquisition time, high spatial resolution, and capability of visualization of all anatomic sites. Consequently, the majority of neck infections are best visualized with CT and are demonstrated in this section.
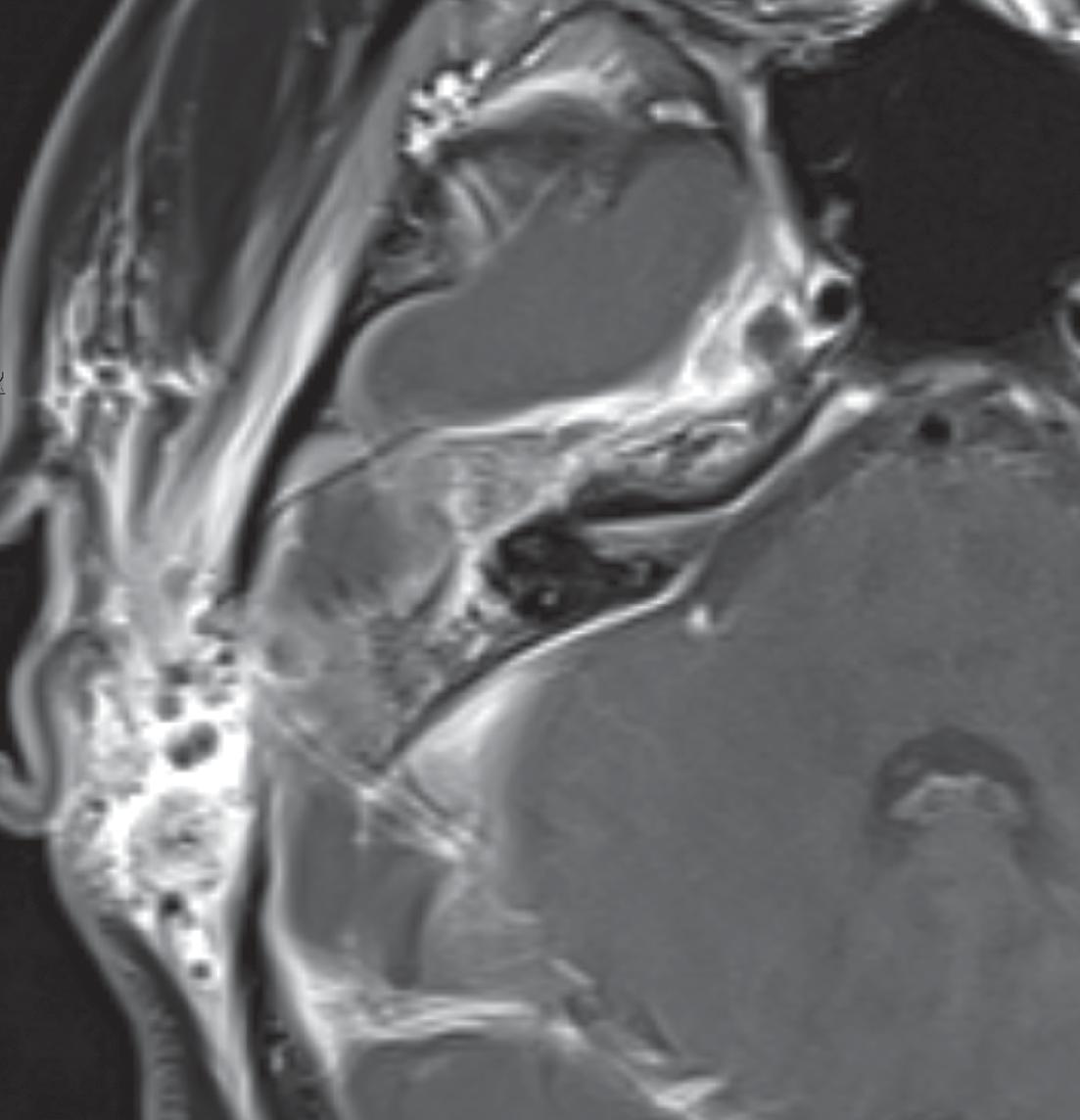
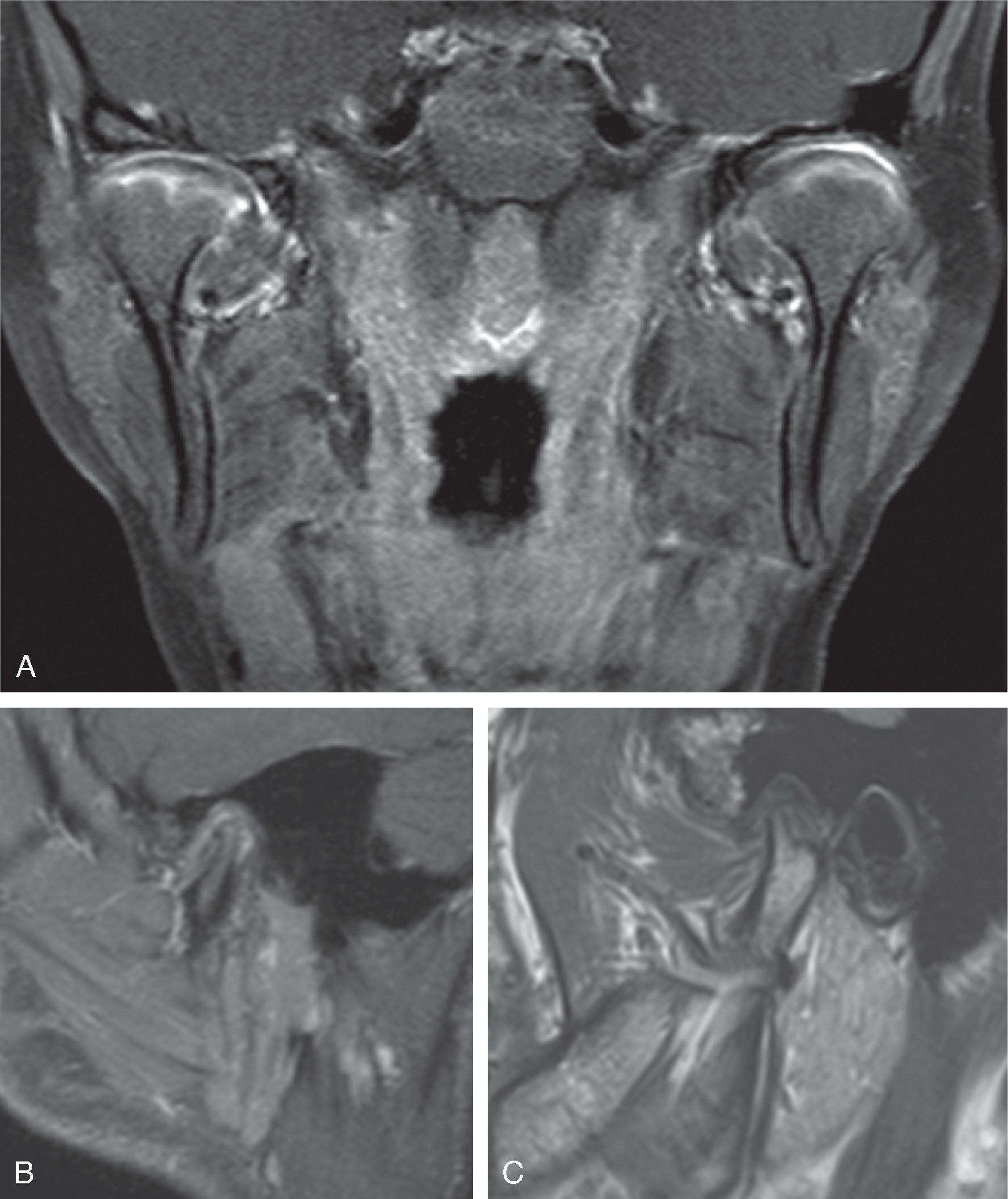
MRI is generally performed to assess complications of infections and intracranial spread of infection. MRI is also performed in the setting of specific infections such as invasive fungal sinusitis or inflammation such as juvenile idiopathic arthritis (JIA) or chronic recurrent multifocal osteomyelitis (CRMO).
This chapter will use a location-based approach for demonstrating infections of the neck that are commonly imaged.

Lymphadenitis refers to infectious enlargement and inflammation of the lymph nodes.
Suppurative lymph nodes refer to necrosis/abscess formation within a lymph node.
Viral and bacterial causes are most frequent.
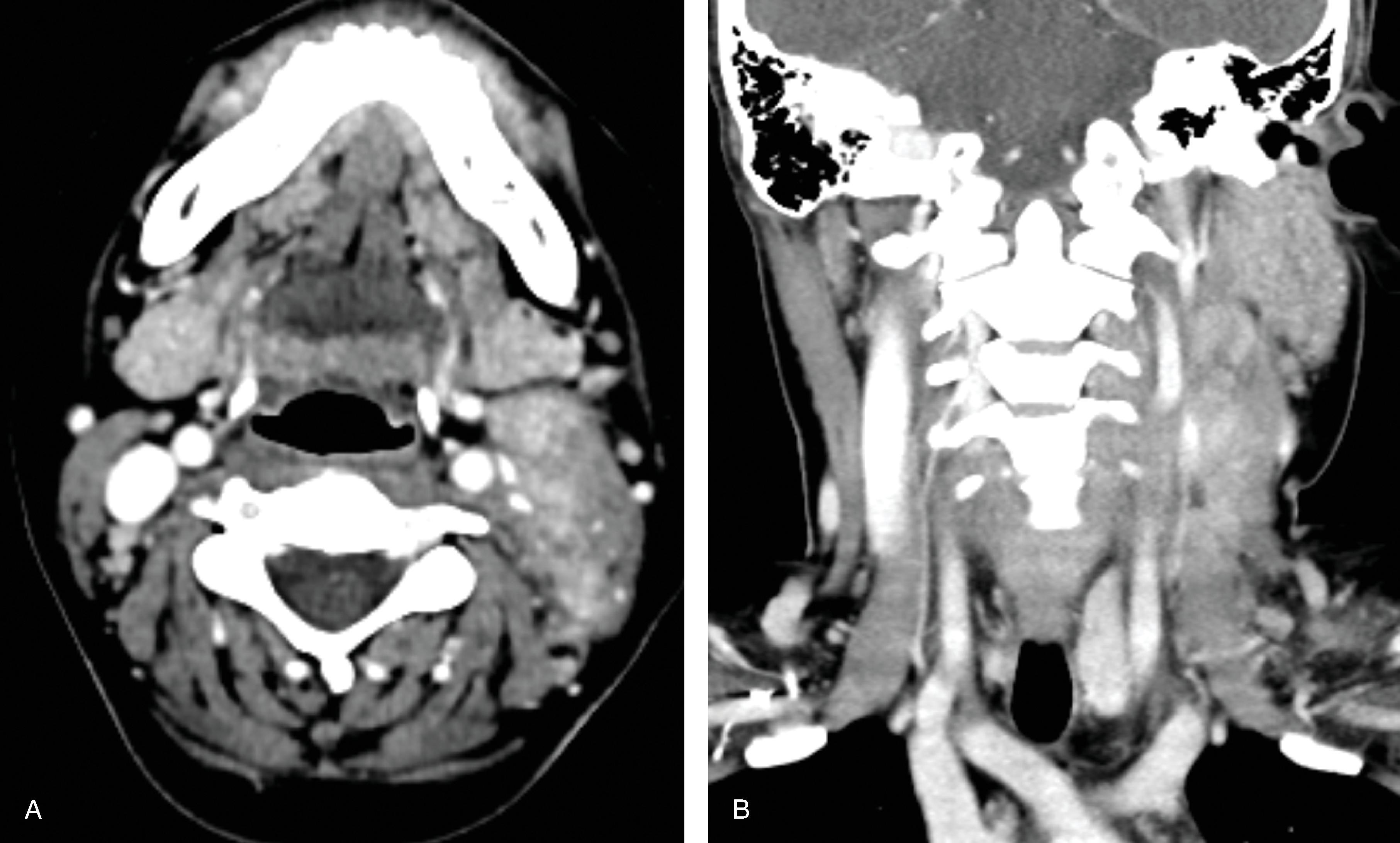
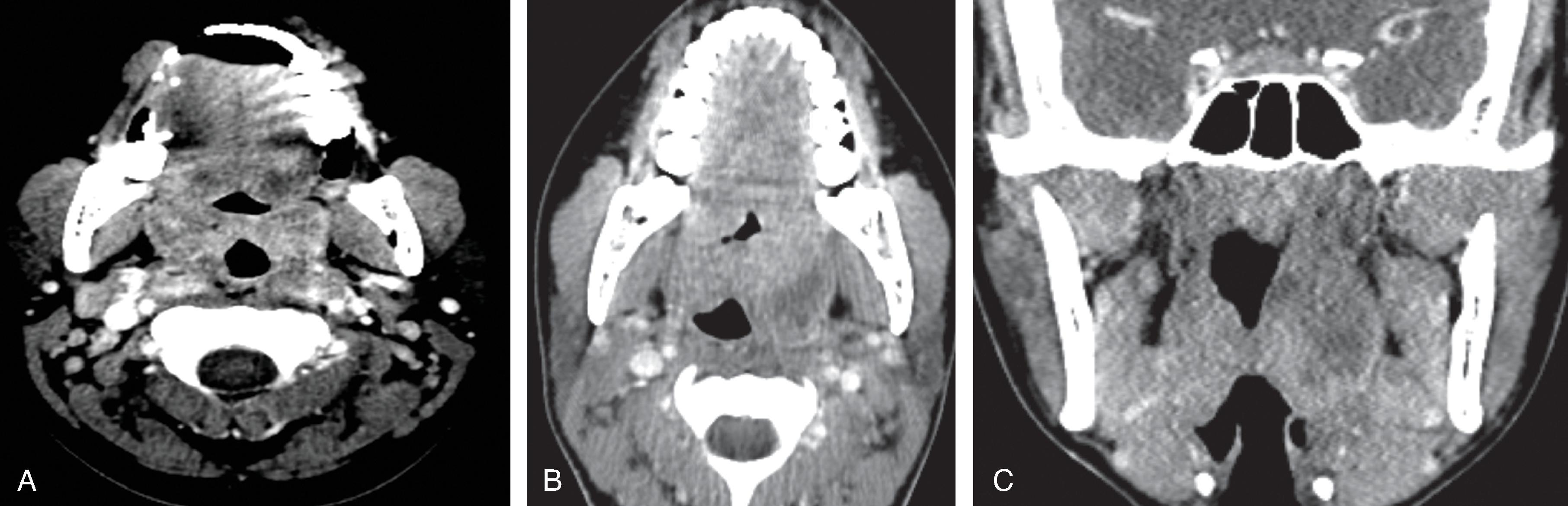









CT: Soft tissue density enlargement of the lymph nodes. Suppurative lymph nodes demonstrate central low density/necrosis.
Associated findings: Perinodal inflammation , compression, and/or occlusion of the internal jugular vein (IJV).
Differential Diagnosis:Lymphoma, and nasopharyngeal carcinoma: Consider these diagnoses for non-suppurative lymphadenopathy that does not resolve after appropriate treatment and consider biopsy to exclude malignancy
Epstein-Barr virus (EBV) is the causative agent spread by human to human contact. 90% to 95% of adults are EBV seropositive. Most cases are subclinical. Peak incidence of infection is 15 to 24 years of age.
Clinical triad includes lymphadenopathy, fever, and pharyngitis . Additional signs and symptoms include fatigue, rash, splenomegaly, atypical lymphocytosis, aseptic meningitis, Guillain-Barre syndrome, encephalomyelitis, transverse myelitis, and optic neuritis. Rare “Alice in Wonderland” syndrome can be triggered by EBV infection and results in distortion of visual perception, body image, and experience of time. Lymphadenopathy peaks in the first week and gradually decreases over the next 2 to 3 weeks. Fatigue may last for 6 months in a minority of patients.
Diagnosis is made with heterophile antibody test in a patient with appropriate clinical presentation. False-negative heterophile antibody tests can occur in early infection and young children and may require EBV-specific antibody testing for diagnosis.
Treatment with acetaminophen or nonsteroidal antiinflammatory medications.
Soft tissue density enlargement of jugular chain lymph nodes; enlarged, striated hyperenhancement of palatine tonsils; and splenomegaly are the most common imaging findings.
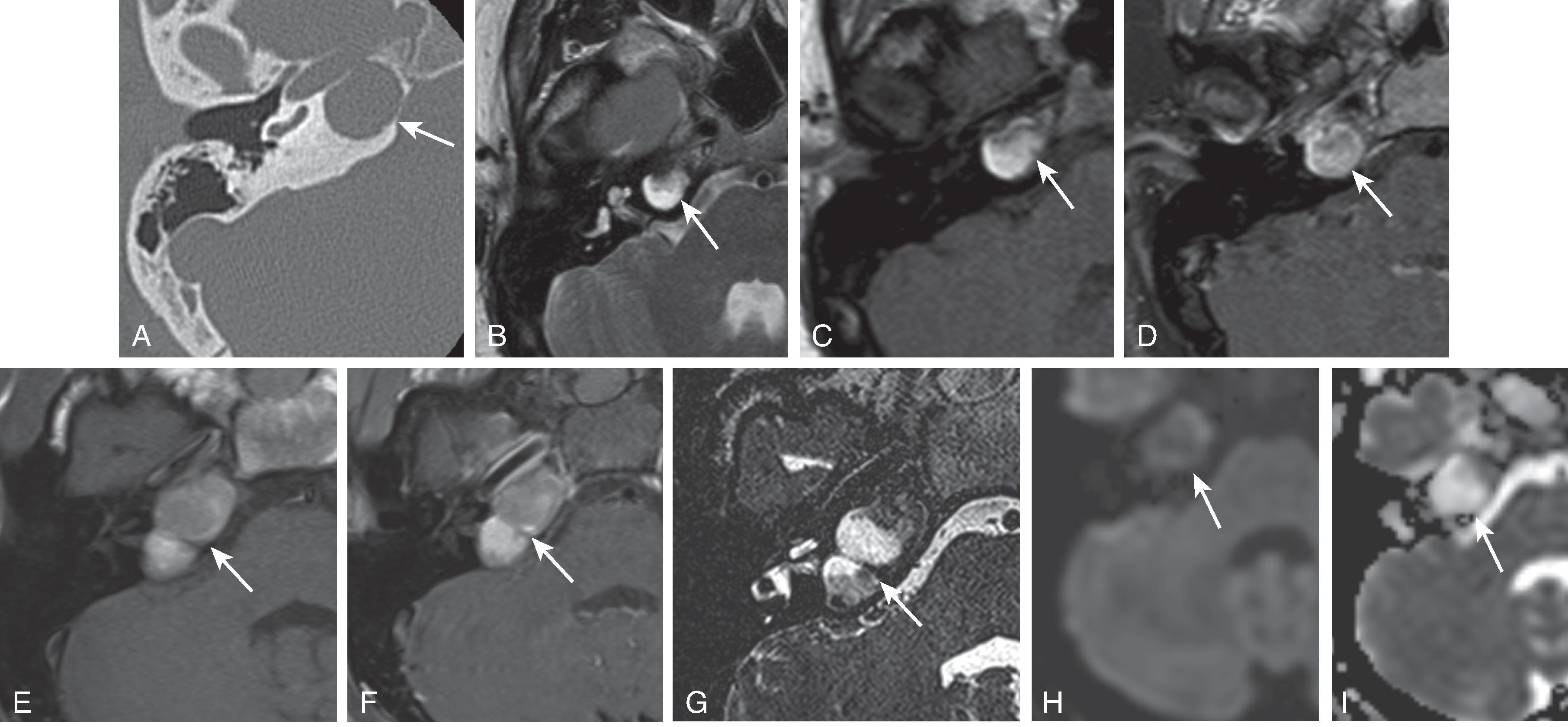
In children, most commonly due to non-tuberculous mycobacterium occurring in children aged 2 to 4 years. Associated violaceous skin discoloration. Frequently involves the parotid space and posterior triangle.
Cat scratch disease is a chronic granulomatous infection due to Bartonella henselae . Typically involves the parotid gland, midcervical, and submandibular nodes. Cat scratch disease can also be seen in conjunction with enhancement of the optic nerve/globe junction due to an obliterative vasculitis.
Lymphadenopathy, and/or suppurative lymph nodes in 50% of patients
Sinus tract formation in 10% of patients
Chronic stage demonstrates multiple calcified lymph nodes
A rare self-limiting histiocytic necrotizing lymphadenitis of unknown origin.
Mean age is 24 years, with age range 12 to 40 years.
Presents with painful cervical lymphadenopathy and prolonged fever.
Diagnosis made through biopsy. No laboratory tests available for diagnosis.
Cases of associated hemophagocytic lymphohistiocytosis have been reported.
Unilateral (60%–80%) lateral neck lymph nodes (levels 2–5) and less commonly remaining nodal locations of the body
Appearance on contrast CT: Hyperenhancement of the lymph nodes relative to muscle density; perinodal inflammation in 93%; homogeneous and necrotic lymph nodes ; small to medium sized nodal enlargement (mean node size 2.3 cm; range 1.8–3.1 cm)
Majority of cases of tonsillitis are viral infections and self-limiting.
30% of tonsillitis cases are bacterial and most commonly due to beta-hemolytic Streptococcus , Streptococcus pneumoniae , Staphylococcus aureus , and Haemophilus influenzae.
Potential etiology of peritonsillar abscess is progression of acute exudative tonsillitis to abscess formation versus inflammation of Weber glands (minor salivary glands located in the soft palate superior to the tonsil, which are responsible for clearing tonsillar debris and digesting food particles).
Symptoms: Fever, sore throat, stiff neck, dysphagia.
Treatment: Drainage (typically abscesses >1 cm), antibiotics, supportive care, and possible steroids.
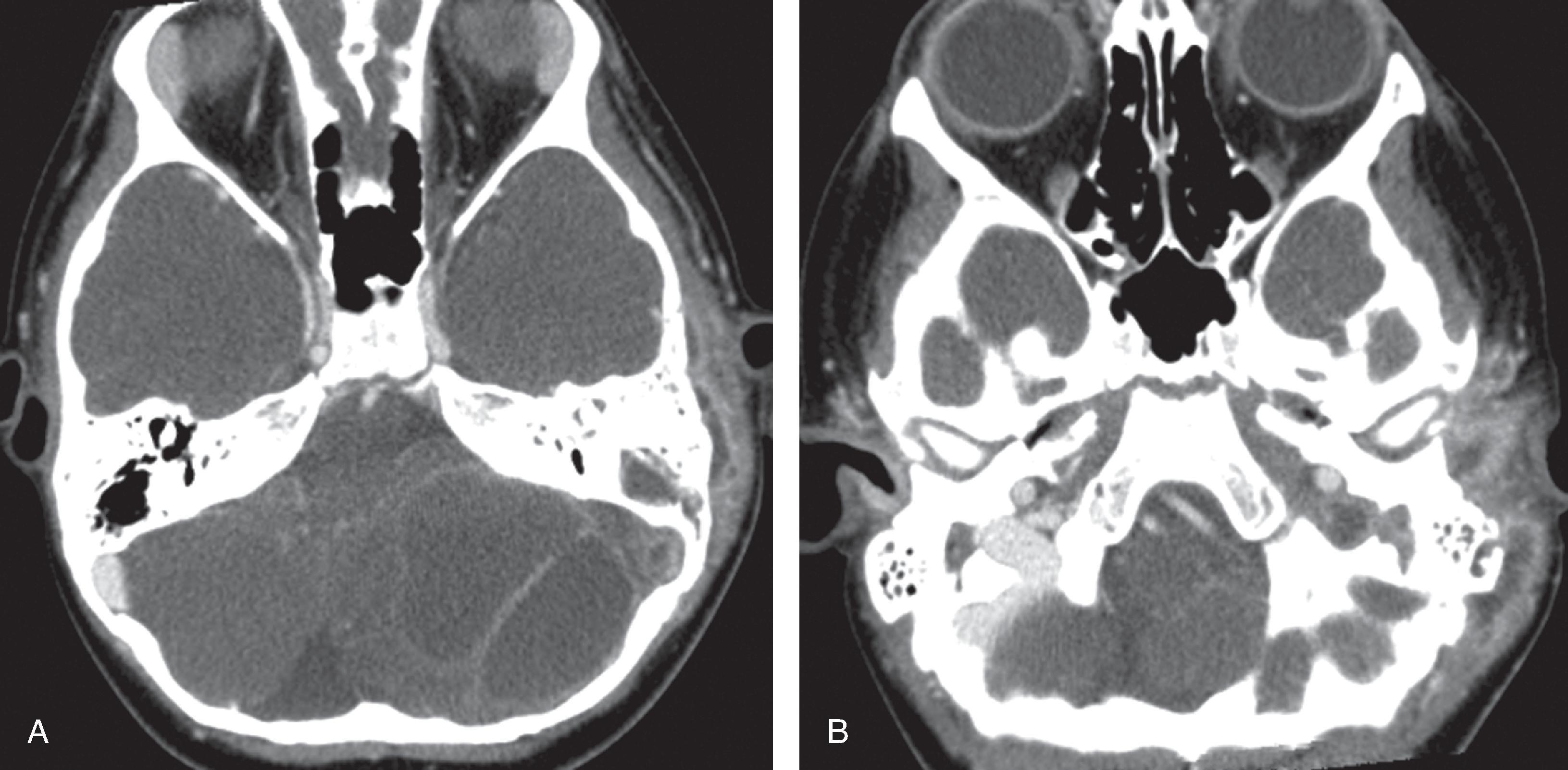
CT: Tonsillitis demonstrates enlarged, hyperenhancing striated palatine tonsils. Peritonsillar abscess is a peripherally enhancing fluid collection involving the palatine tonsil.
Complications: Airway obstruction, aspiration pneumonia, deep neck cellulitis and/or mediastinitis, jugular thrombosis, and hemorrhage from carotid artery wall erosion.
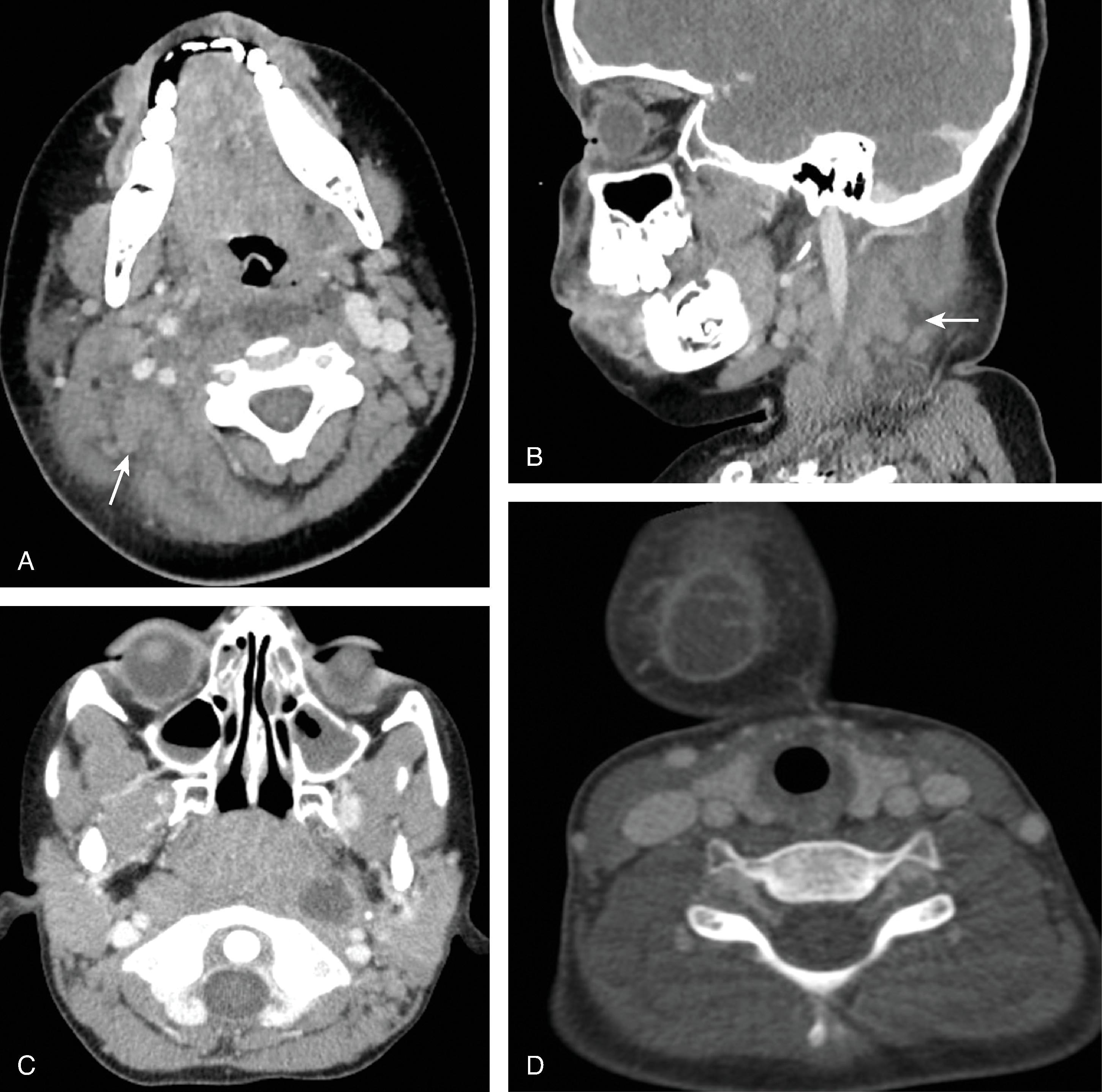
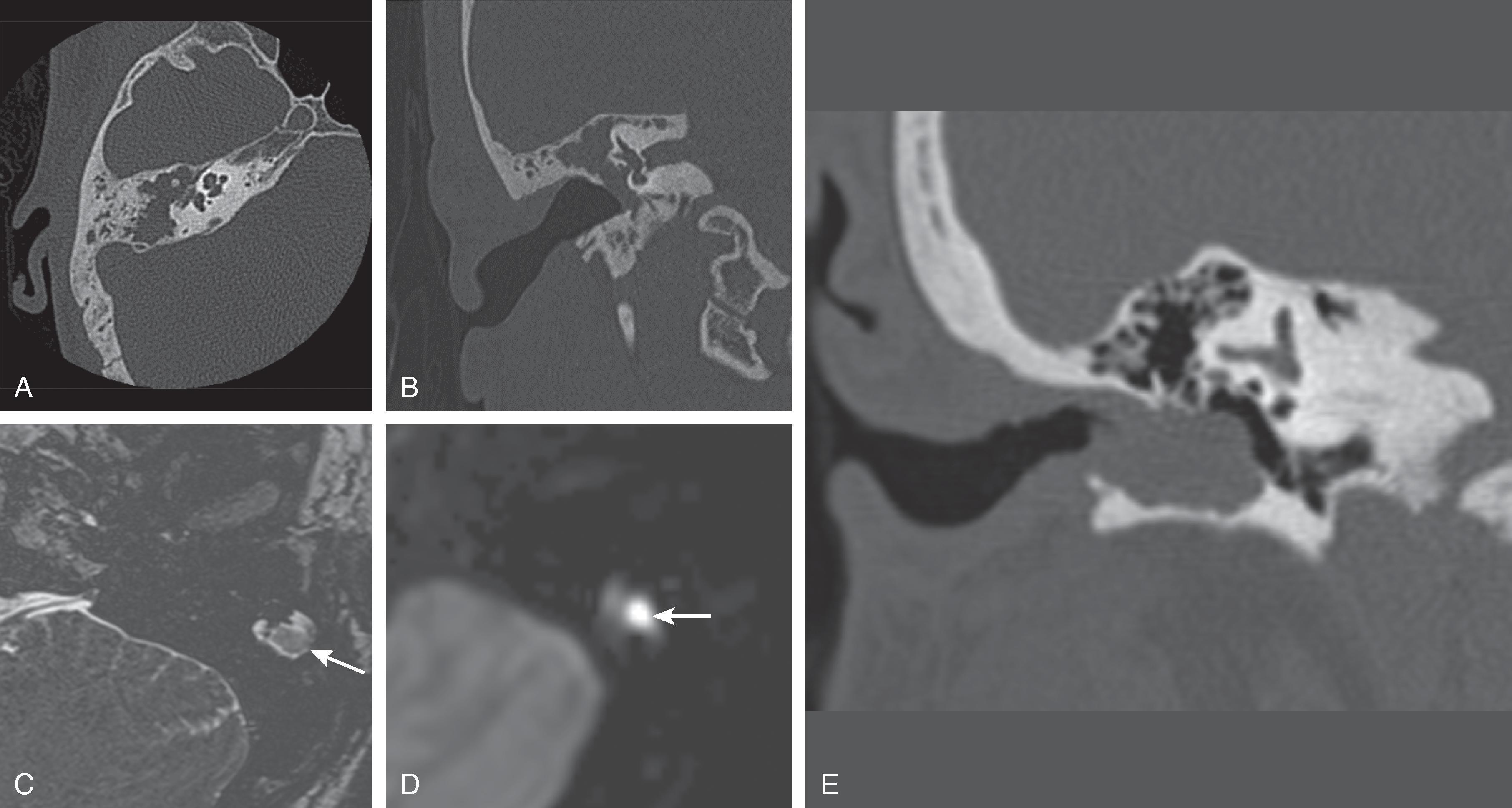
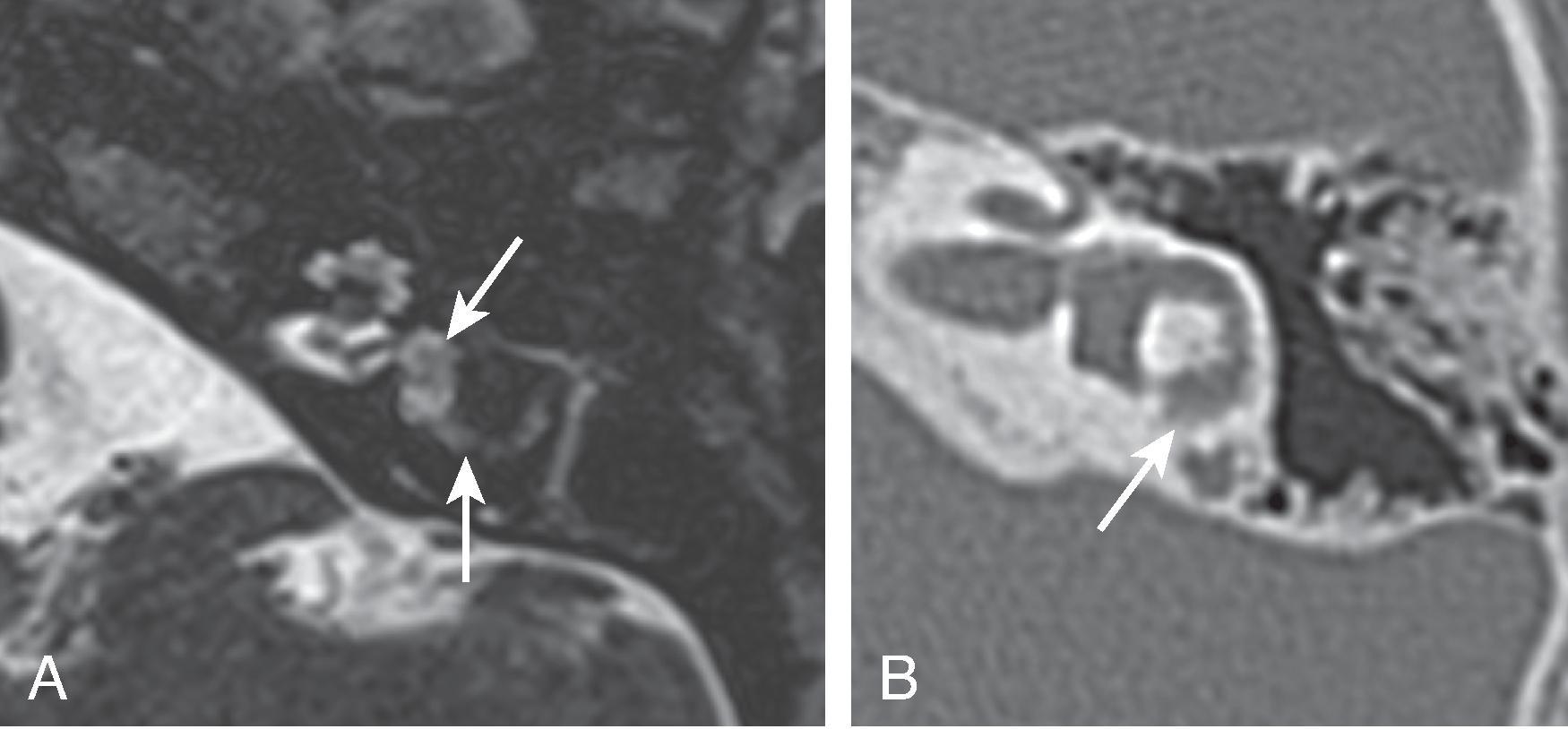
Rare complication of an oropharyngeal infection.
Typically found in previously healthy teenagers.
Results in septic dissemination with abscess formation in other parts of the body, most commonly the lungs, osteomyelitis, and arterial vasospasm or occlusion.
Typically caused by Fusobacterium infection, which is an anaerobic Gram-negative bacterium found in normal oral flora.
High morbidity/mortality associated if it is not treated in a timely manner.
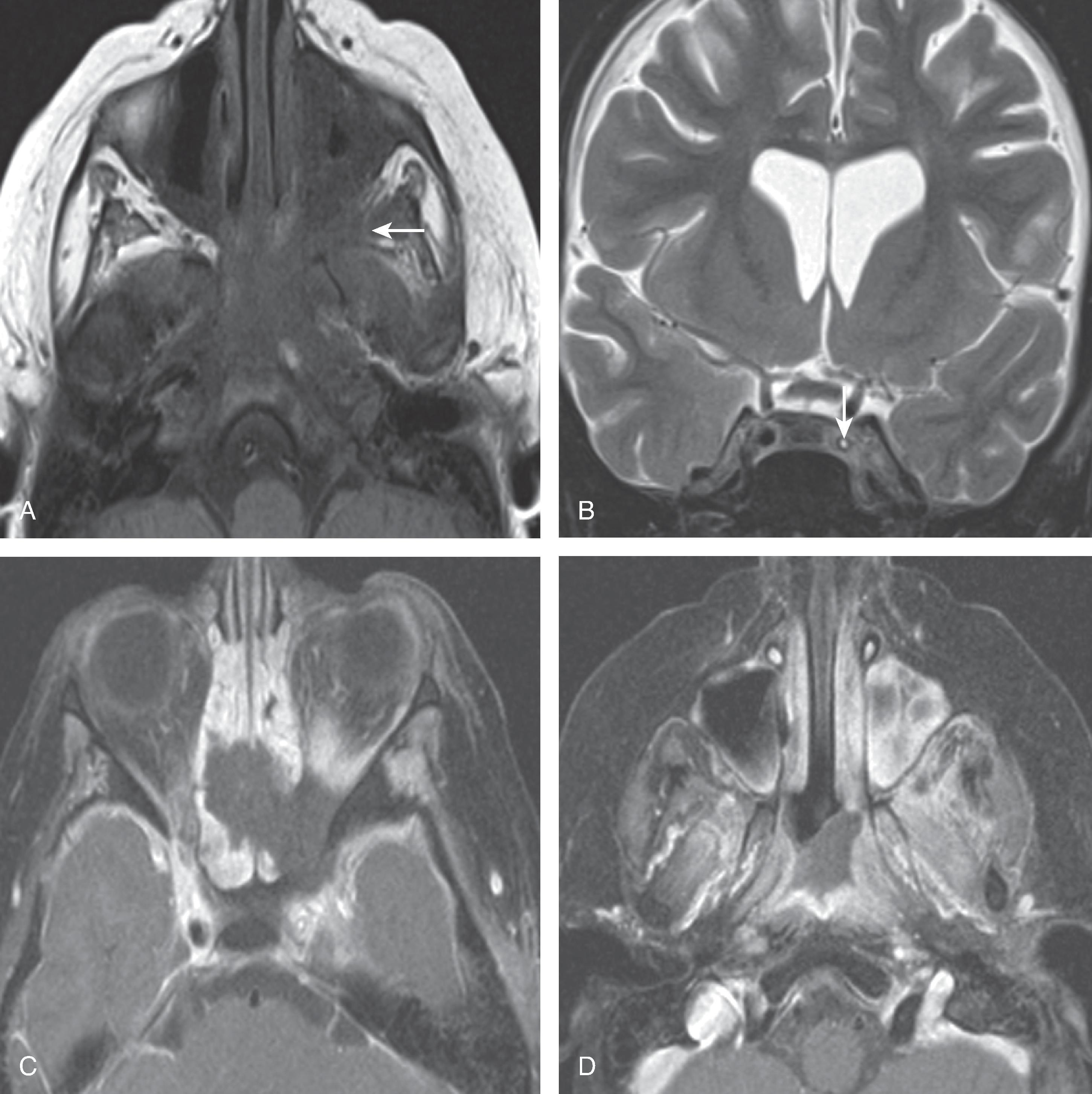
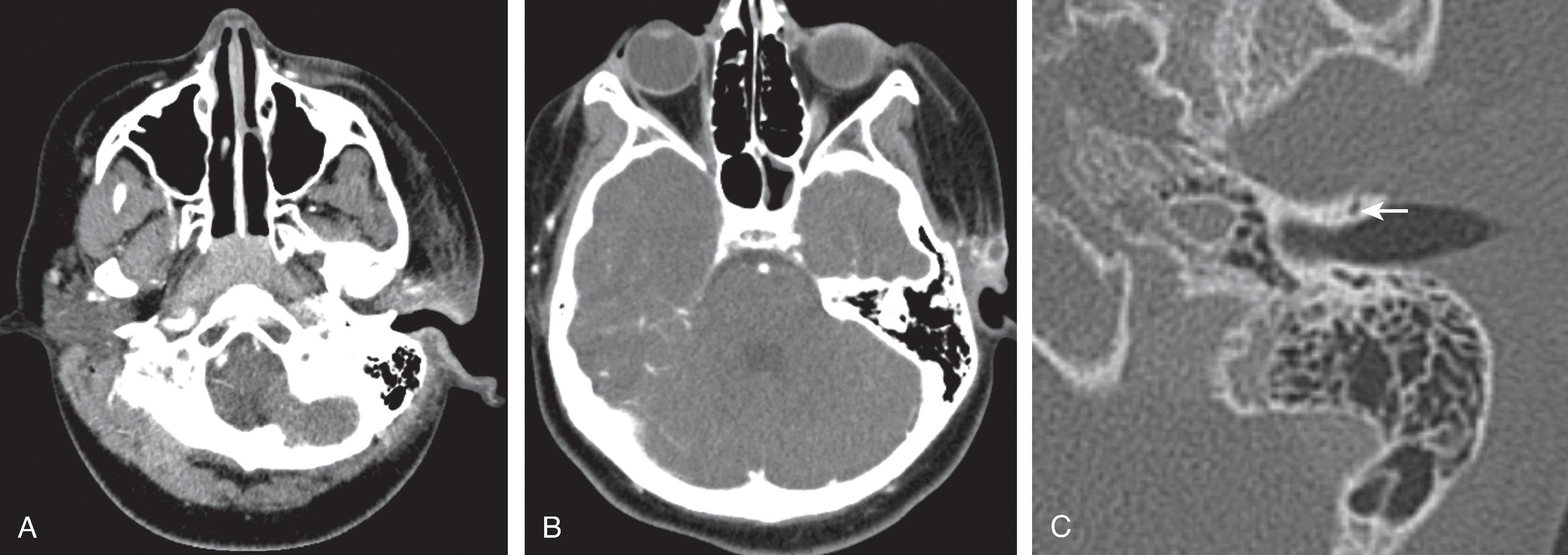
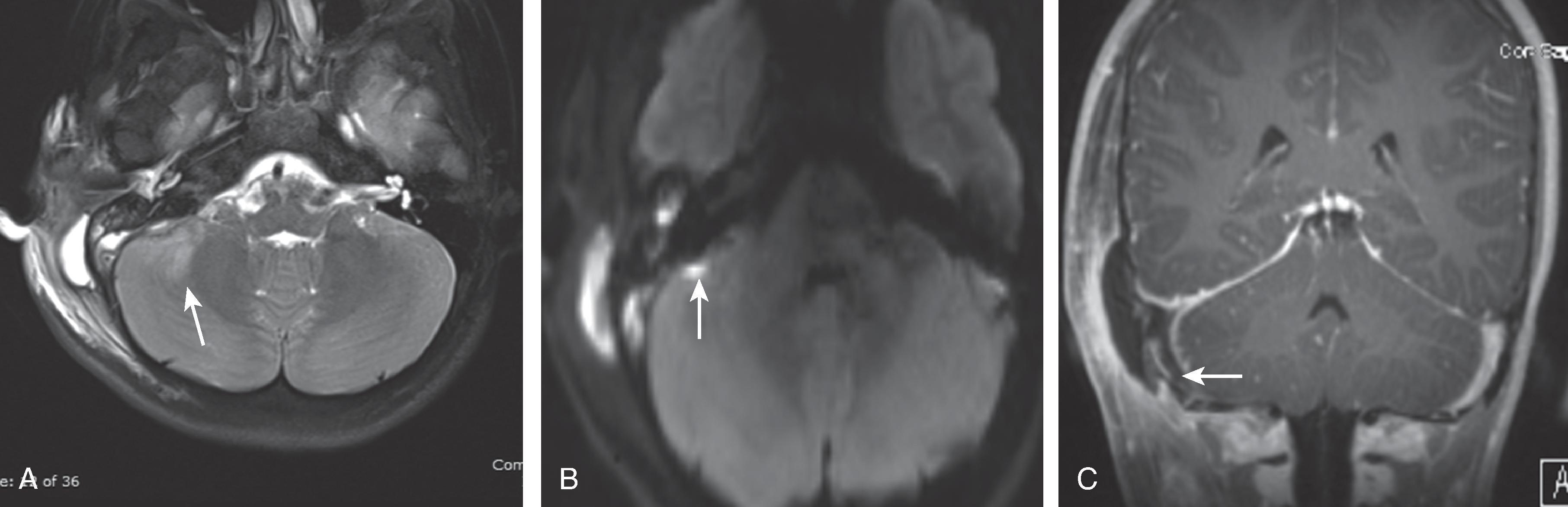
The infection spreads from the peritonsillar space to result in internal jugular vein (IJV) thrombosis .
IJV involvement can be resultant septic emboli to the lungs or brain, thus causing an abscess. There may also be spread into the retropharyngeal space, resulting in osteomyelitis of the spine.
Treatment is high-dose IV antibiotics. Anticoagulation is used in up to 27% of patients; however, the role of this treatment is not clear at this time.
Triad of pharyngitis, ipsilateral IJV thrombosis, and associated cavitary pulmonary nodules
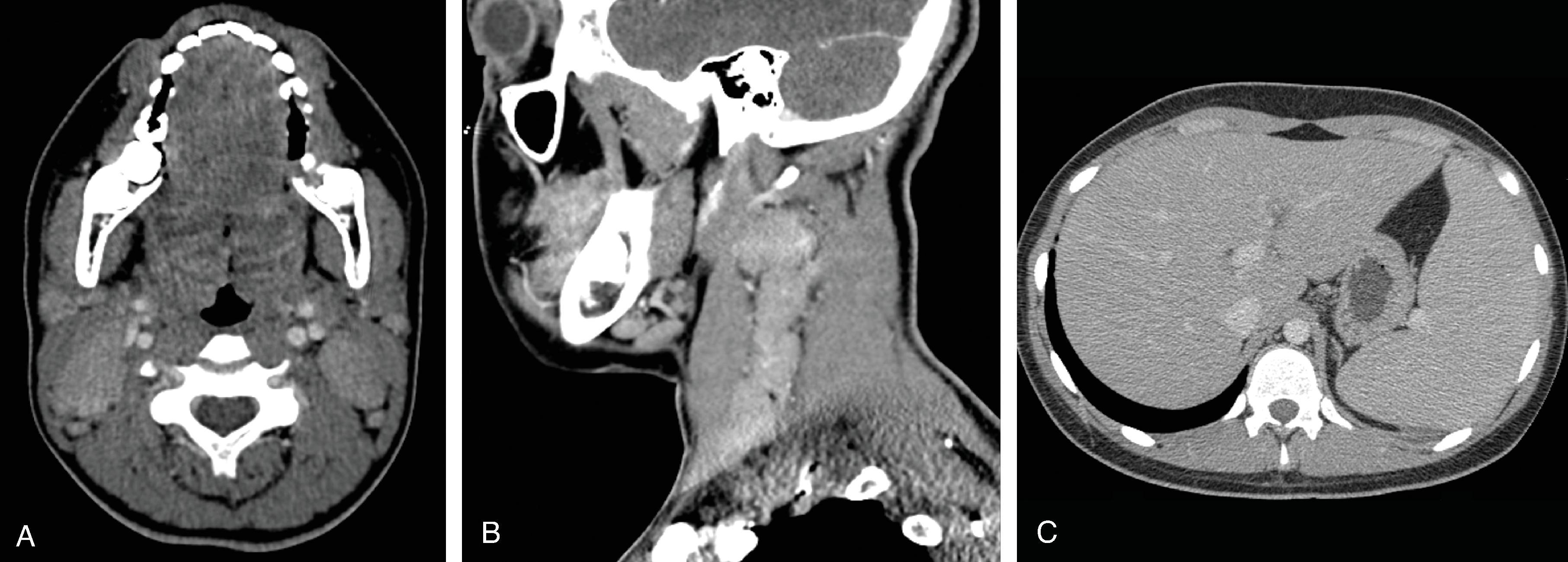
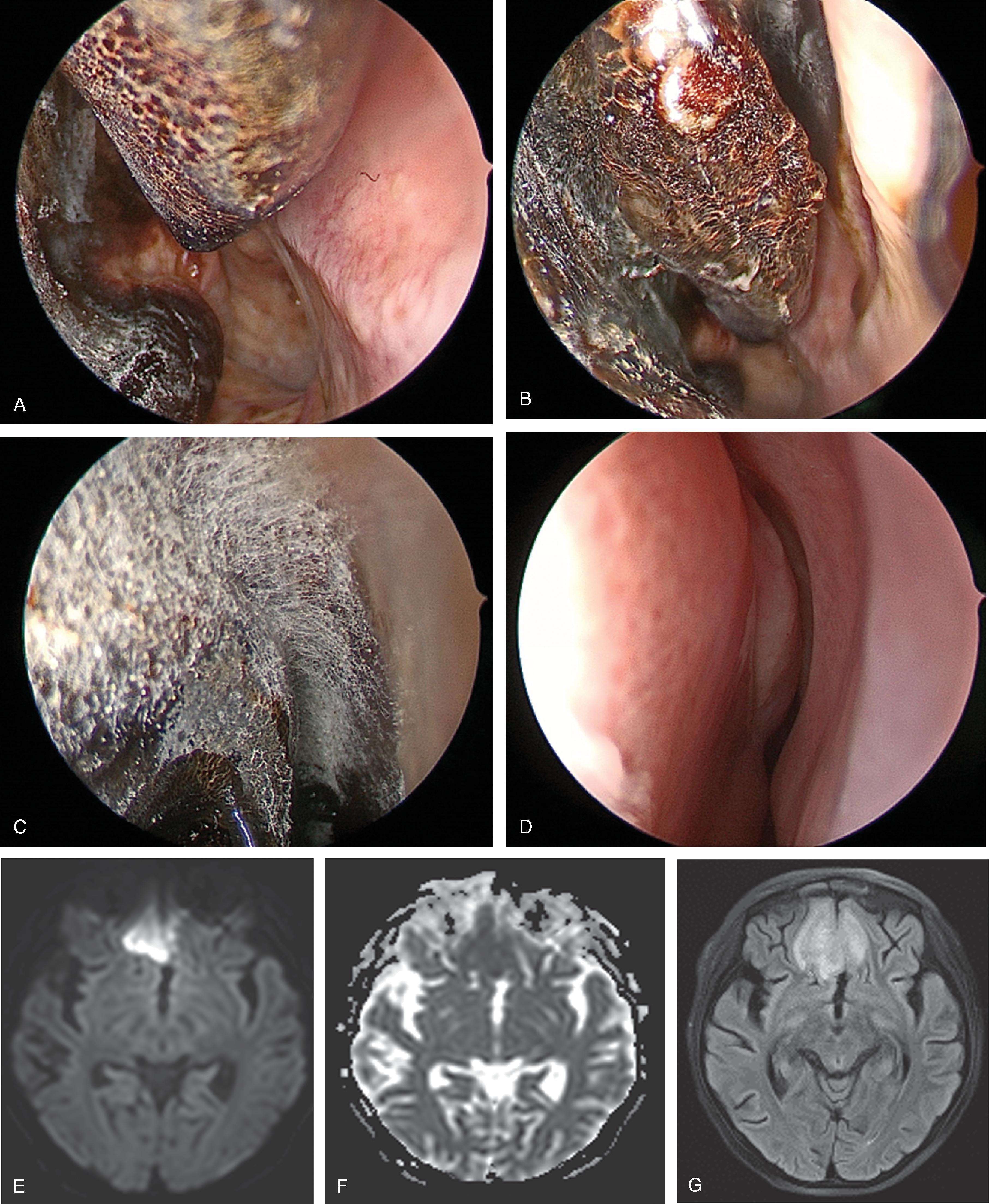
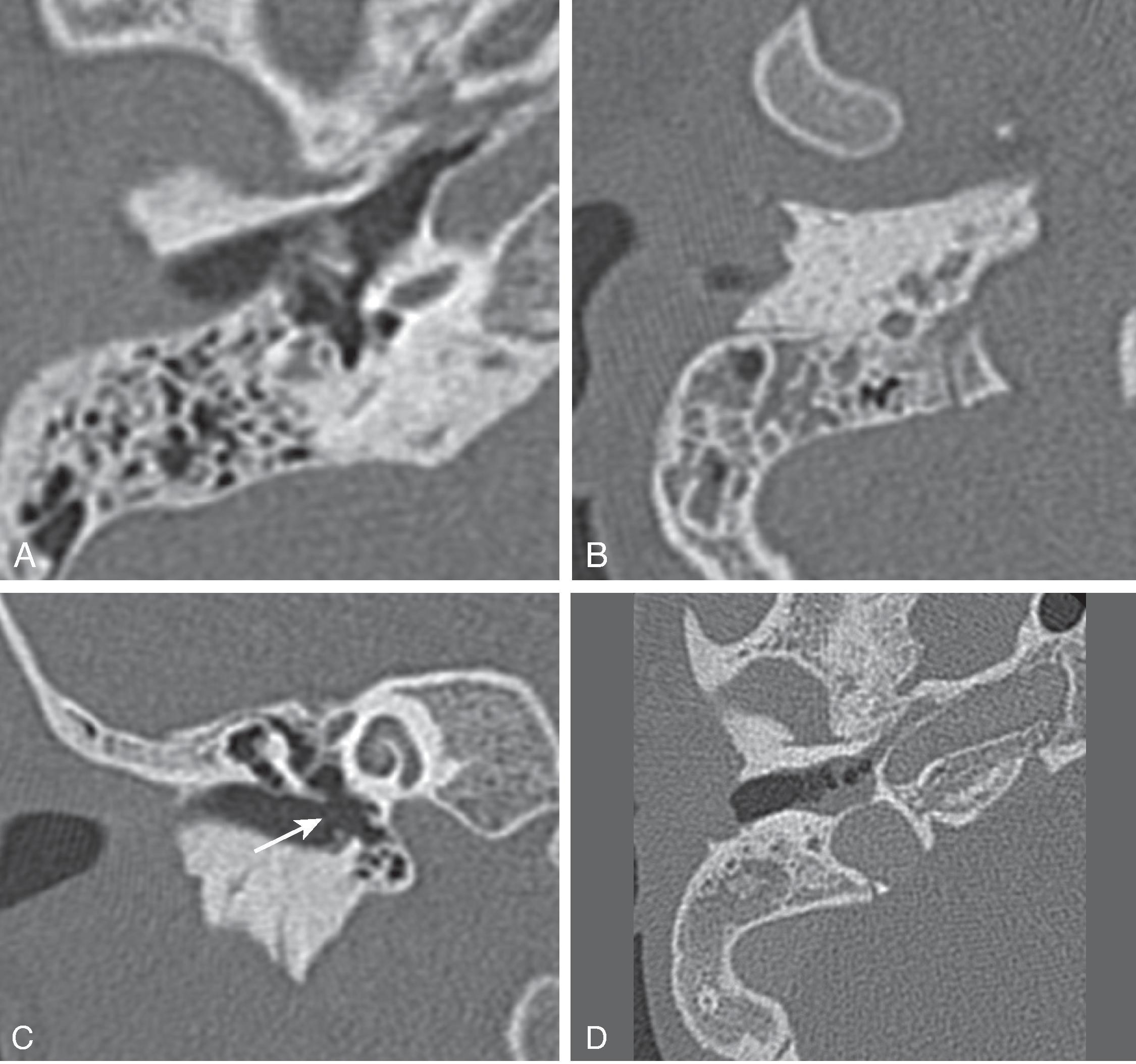
The source of infection is often from rupture of a suppurative retropharyngeal lymph node.
Potentially life threatening due to effect of airway.
Surgical drainage often necessary.
Typical features of an abscess i.e. peripheral rim enhancement with central low density
Usually associated with lymphadenopathy in the lateral neck
Can extend into the mediastinum as well as cause IJV thrombophlebitis, or carotid pseudoaneurysm
<insert fig 15.8 >
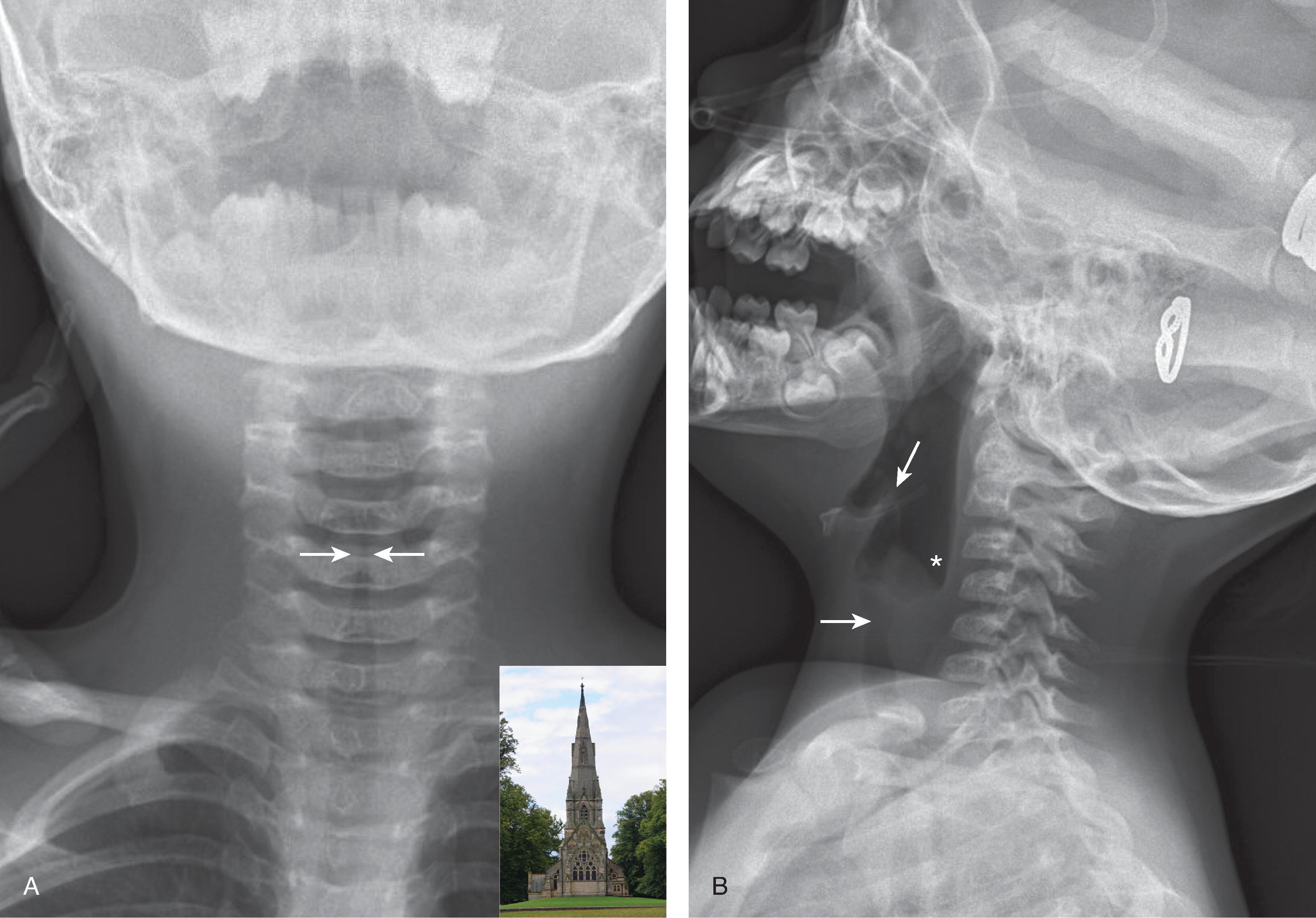
Most common cause of upper airway obstruction in children aged 6 months to 3 years.
The most common etiologic agents for viral croup are parainfluenza and influenza, which induce an inflammatory response resulting in subglottic edema and airway narrowing.
Clinically, it is characterized by low-grade fever, inspiratory stridor, a characteristic barking cough, and hoarseness.
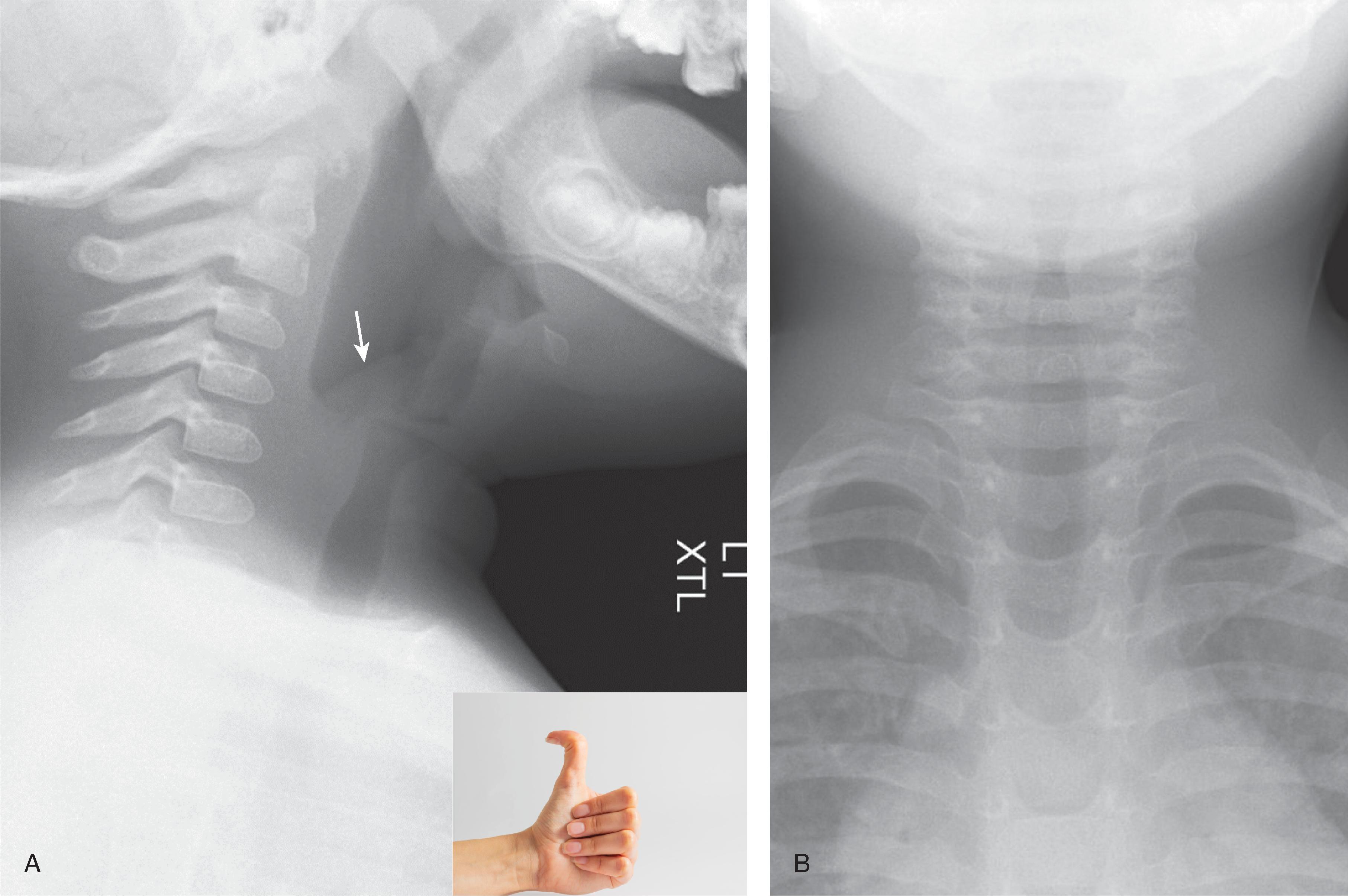
Typically a clinical diagnosis, but airway studies are often obtained for diagnostic confirmation and exclusion of other causes of acute-onset stridor, such as epiglottis.
Characteristic “steeple” shape below the vocal cords on a frontal radiograph.
Epiglottis, aryepiglottic folds, and prevertebral spaces are normal in croup.
Potential life-threatening cause of upper airway obstruction in children.
Characterized by inflammation/swelling of the epiglottis and aryepiglottic folds but can also extend to involve the false cords and subglottic region.
The agents that can result in epiglottis are H. influenzae , Streptococcus and Staphylococcus , Morazella , and Pseudomonas .
With the increasing immunizations, the incidence of H. influenzae has dramatically decreased and so has epiglottitis.
Typically occurs in children between 3 and 6 years of age.
Patients typically appear toxic with acute stridor, dysphagia, fever, restlessness, drooling, and increased respiratory distress while lying down.
Typically diagnosed with radiography. Endoscopy is obtained for confirmation.
Lateral radiograph demonstrates marked swelling/enlargement of the epiglottis (‘thumb print’ sign).
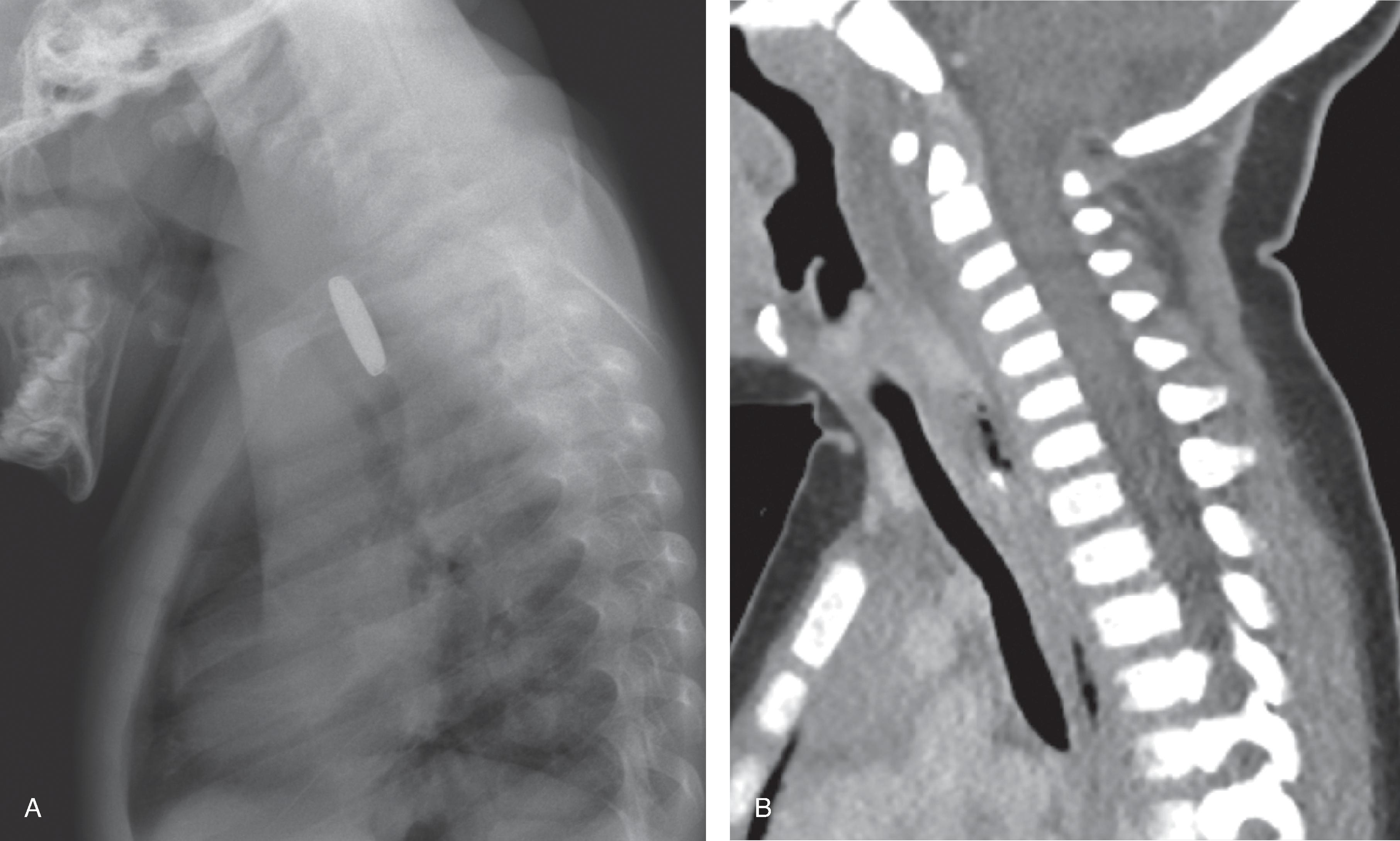
Foreign body ingestion is common in infants and young children.
Button batteries can cause rapid-onset full thickness burns and esophageal perforation, occuring within 2 hours of ingestion .
AP and lateral radiographs can confirm a battery rather than a coin by the double rim on AP projection and step off on the lateral projection.
Batteries lodged in the esophagus should be removed as soon as possible. The majority of batteries found beyond the gastroesophageal junction will pass spontaneously unless swallowed with one or more magnets.
Complications of battery ingestion include fistulas (aortoesophageal, trachea-esophageal), esophageal and tracheal stenosis, vocal cord paralysis, cellulitis, and discitis and osteomyelitis
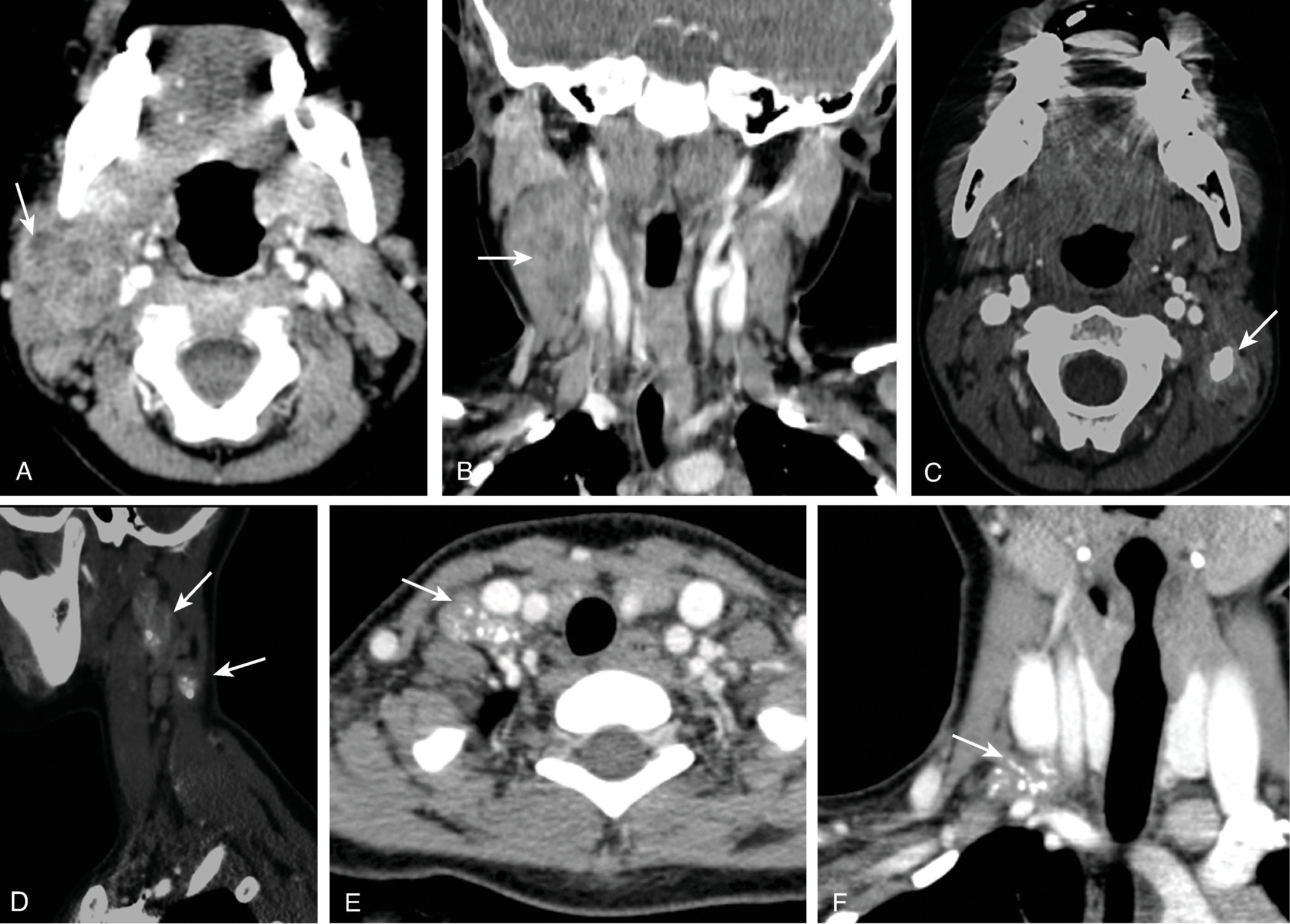
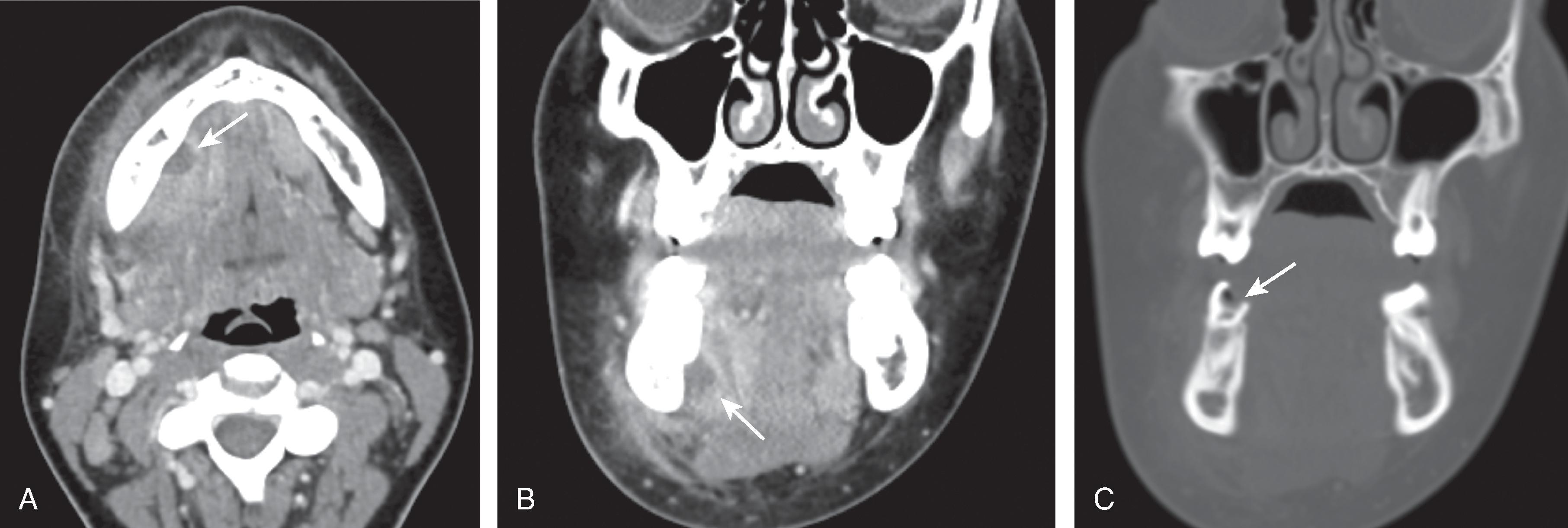
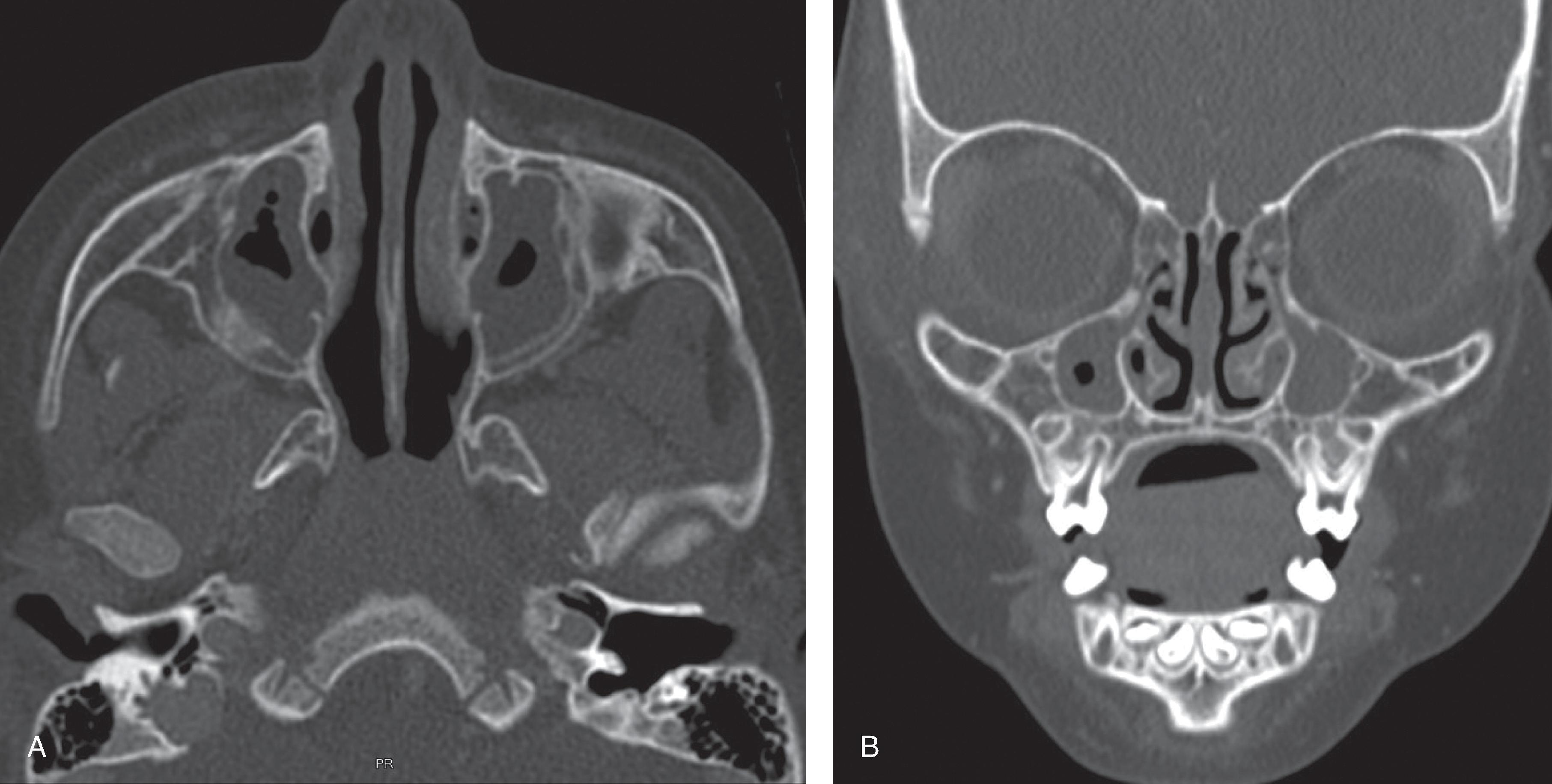
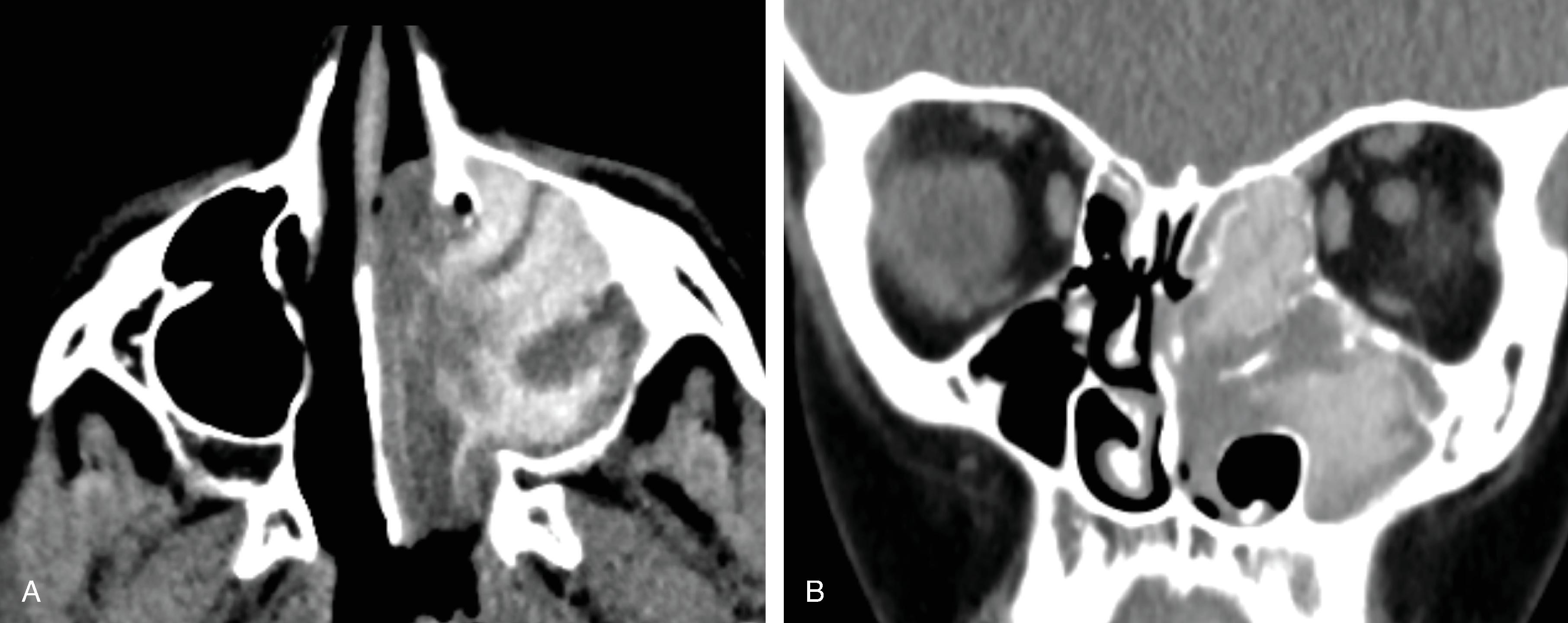
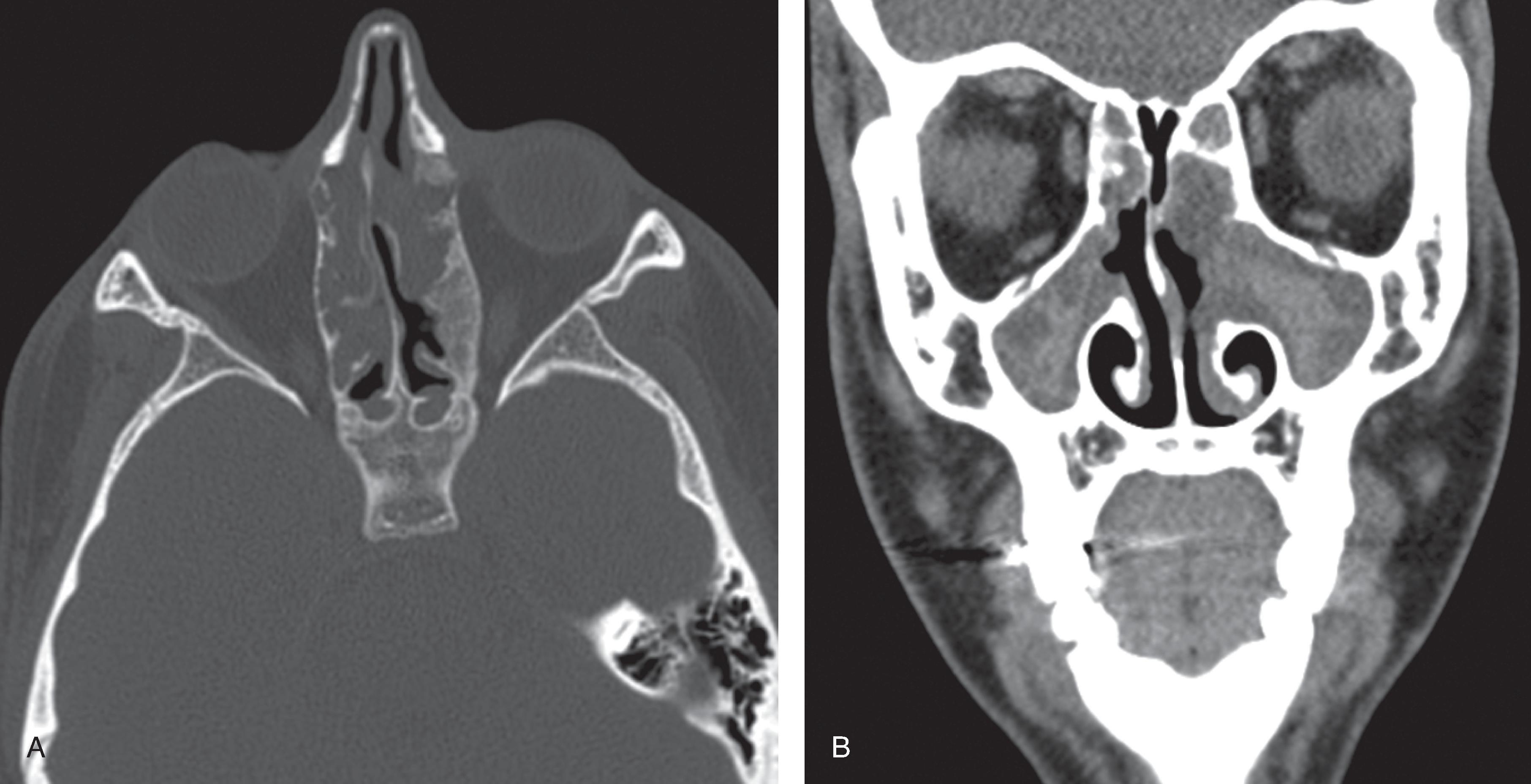
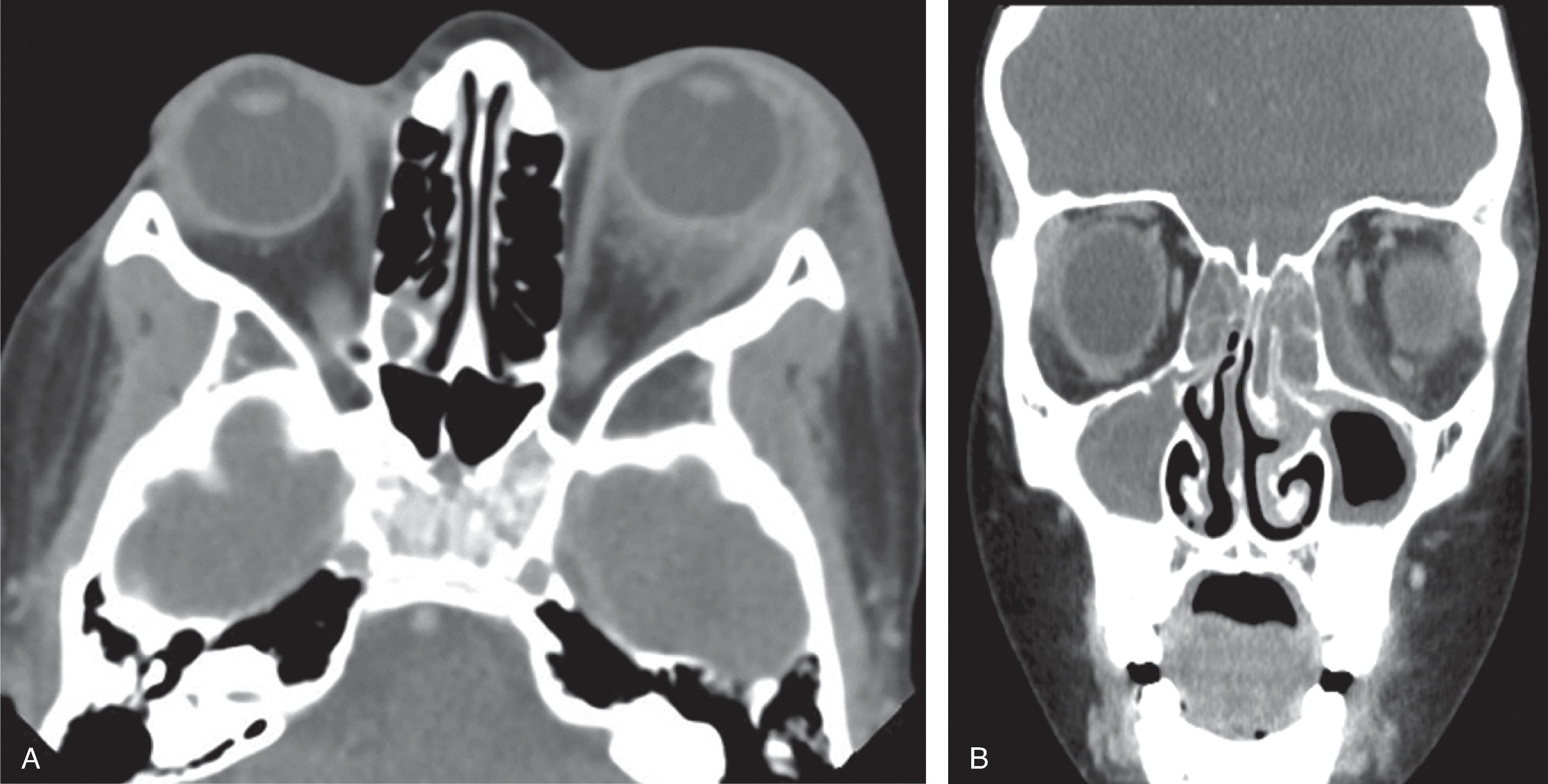
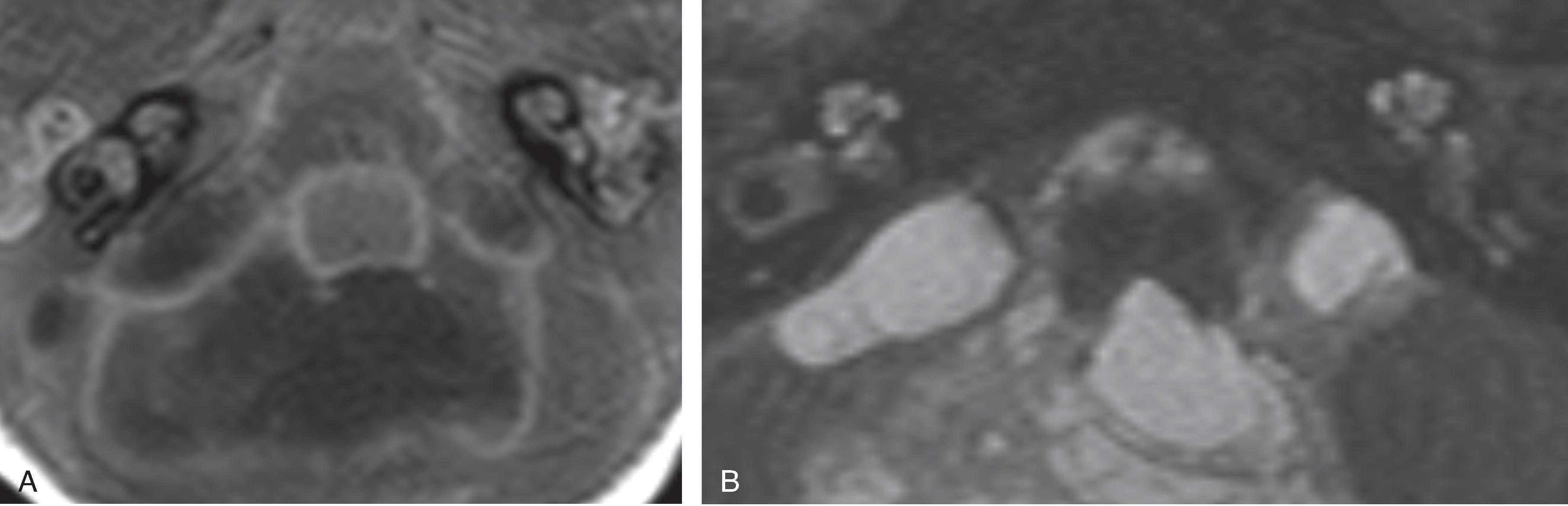
Oral cavity infections are a common health care problem in children and are most commonly from odontogenic origin . Breakdown of tooth enamel allows for oropharyngeal bacteria to enter the tooth cavity, track into the root canal and into the mandible or maxilla, and lead to a periodontal infection. Subsequent acute infection leads to cellulitis, dentoalveolar abscess, fascia infection or necrotizing fasciitis, and potentially hematogenous spread. Chronic infection can lead to periapical cyst or granuloma, osteomyelitis, or fistula.
Oral cavity infections are polymicrobial consisting of anaerobic and aerobic bacteria.
Symptoms include odynophagia, facial pain, swelling, and erythema. Ludwig’s angina is a rare, rapidly progressive gangrenous floor of mouth cellulitis and edema that can progress to airway obstruction.
Early treatment is important to prevent systemic spread of infection. Treatment includes pain control, antibiotics, early tooth extraction, and incision and drainage of abscess when present.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here