Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Early reports of leukemia-free survival, following human leukocyte antigen (HLA)-identical sibling hematopoietic cell transplantation (HCT) for refractory acute leukemia, was reported in the 1970s. Since then, allogeneic HCT has evolved into an effective and increasingly safe, curative, and intent therapeutic modality for hematologic malignancies. The indications and applicability of HCT for specific diseases change over time, especially as non-transplant treatment options and our understanding of disease biology improve. For example, in chronic myelogenous leukemia (CML), molecularly targeted therapy has almost completely replaced HCT since the early 2000s. At the same time, developments in HCT, such as the advent of reduced intensity conditioning (RIC), the use of mismatched, haploidentical-related donor and cord blood grafts, and improvements in supportive care, have increased the scope and applicability of allogeneic HCT. Allogeneic HCT is increasingly used in older patients, ethnic minorities, those for whom fully HLA-matched donors are not available, and those in whom fully HLA-matched donors are used as a salvage strategy after relapse. Transplant-related mortality (also referred to as non-relapse mortality [NRM]), despite declining over the years, remains an important challenge; posttransplant relapse has emerged as a major therapeutic focus. General principles, indications, donor selection, and optimal timing of allogeneic HCT for hematologic malignancies in adults and post-HCT outcomes are discussed in this chapter.
Allogeneic HCT involves administration of a conditioning (or preparative) regimen of chemotherapy (with or without radiation) and immunosuppressive medications, followed by infusion of donor hematopoietic progenitor cells. Most patients then receive several months of immune suppression therapy to prevent or treat graft-versus-host disease (GVHD). The purpose of the conditioning regimen is twofold: to eradicate malignant cells and to eliminate host immune cells (capable of rejecting even HLA-identical sibling donor cells). The ability to restore hematopoiesis with donor hematopoietic progenitor cells permits the administration of substantially higher (myeloablative) doses of cytotoxic therapy, than is otherwise possible. Additionally graft-versus-malignancy (GVM) effects, conferred by alloreactive donor immune cells, contribute substantially to cancer eradication and relapse prevention.
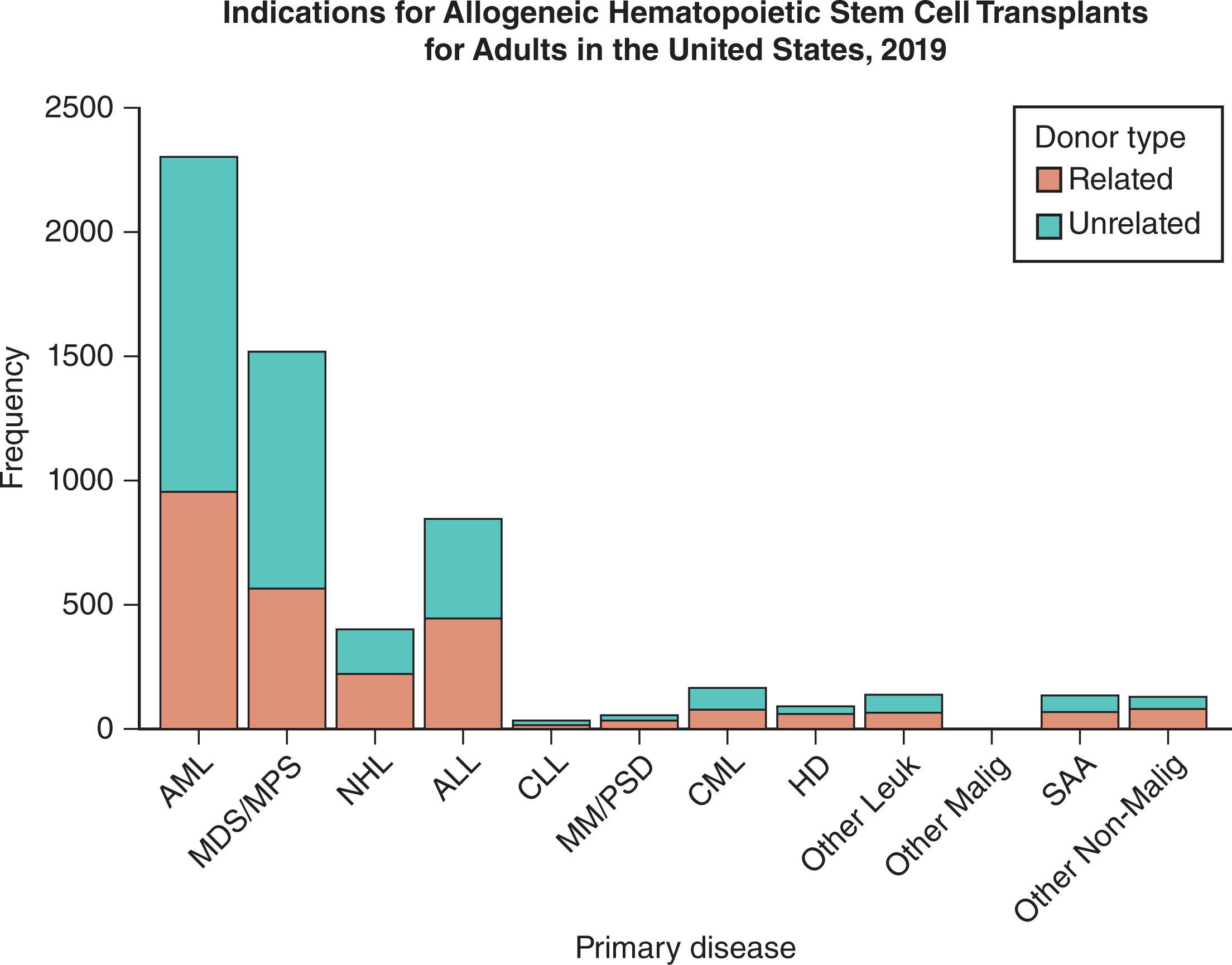
The Center for International Blood and Marrow Transplant Research (CIBMTR) collects data on HCT outcomes from over 500 worldwide participating centers and on all allogeneic transplants in the United States. Approximately 83,700 allogeneic HCT were performed in the United States between 2010 and 2018. In 2018, approximately 2371 matched sibling donors, 4309 unrelated adult donors, 1503 haploidentical donors (defined as a related donor with two or more antigen mismatches), and 466 cord blood transplants were performed in the United States, including approximately 7500 in adult patients. Hematologic malignancies are the most common indications for allogeneic HCT. Acute myeloid leukemia (AML), myelodysplastic syndrome/myeloproliferative neoplasms (MDS/MPN), and acute lymphoblastic leukemia (ALL) currently constitute the three most common indications of allogeneic HCT ( Fig. 105.1 ).
In recent years, improved supportive care and the use of RIC have led to an increase in allogeneic HCT for older adults. Only 4% of allogeneic HCT-recipients, from 1987 to 1992, were older than 50 years. In 2018, 45% were older than 55 years and 20% were 65 years or older. The use of allogeneic HCT in patients 70 years and older in the United States increased substantially in the past decade, from 5 (0.1%) in 2000, to 283 (3.85%) in 2013. Allogeneic transplantation, in patients without HLA-identical siblings, was facilitated by establishment of large unrelated donor registries around the globe. From 1987 to 1992, less than 10% of HCTs, for hematologic malignancies, used unrelated donors; in 2018, this figure was approximately 80%. Increased utilization of HCT among older adults, increasing use of unrelated donors, and more recently, haploidentical-related donors have been the main reasons for the steady growth in allogeneic HCT over the last decade. In 2011, approximately 300 haploidentical-related donor transplants were reported to the CIBMTR, compared with nearly 1500 transplants in 2018. The number of cord blood transplants declined concomitantly from a high of 816 in 2011, to approximately 500 in 2018. Over the years in the United States, the increase in the number of allogeneic HCT has been most striking in African Americans, while the number of allogeneic HCT for all indications increased by 7% from 2010 to 2018 for White people, the growth was 63% for African Americans, and 21% for Hispanics. A threefold increase occurred between 2010 and 2018 in haploidentical HCT; in 2018, approximately 20% of haploidentical HCT were performed in African Americans.
Historically, conditioning regimens included myeloablative doses of cytotoxic drugs—with or without radiation—intended to provide disease control and induce host immunosuppression (to prevent graft rejection). Myeloablative conditioning (MAC) regimens for hematologic malignancies often involve a combination of cyclophosphamide (commonly 60 mg/kg/day for 2 days) and either busulfan (typically 3.2 mg/kg/day intravenously for 4 days or a similar pharmacokinetic guided dose) or, historically, conditioning regimens included total body irradiation (TBI) (5 to 15 Gy, single or fractionated doses). Posttransplant survival rates are broadly similar with either of the above approaches, although an advantage for pharmacokinetic-guided busulfan regimens has been shown for myeloid malignancies. In a variety of regimens, other drugs such as fludarabine, etoposide, melphalan, and thiotepa are sometimes added to or substituted for cyclophosphamide and/or busulfan in efforts to provide better, generally disease-specific, antineoplastic activity. An Italian phase III randomized study in AML patients compared the two common MAC regimens (intravenous busulfan plus cyclophosphamide [BU CY], with busulfan plus fludarabine [Flu BU]) and demonstrated lower NRM (with busulfan plus fludarabine), without affecting relapse risk. In a study randomizing AML patients to high-dose cyclophosphamide and either 12 Gy or 15.75 Gy TBI as conditioning, a lower relapse risk in the 15.75 Gy TBI group was offset by higher NRM risk leading to similar OS. A more recent CIBMTR study also reported that higher doses of TBI over the standard dose (12 Gy) were associated with worse NRM and offered no survival benefit.
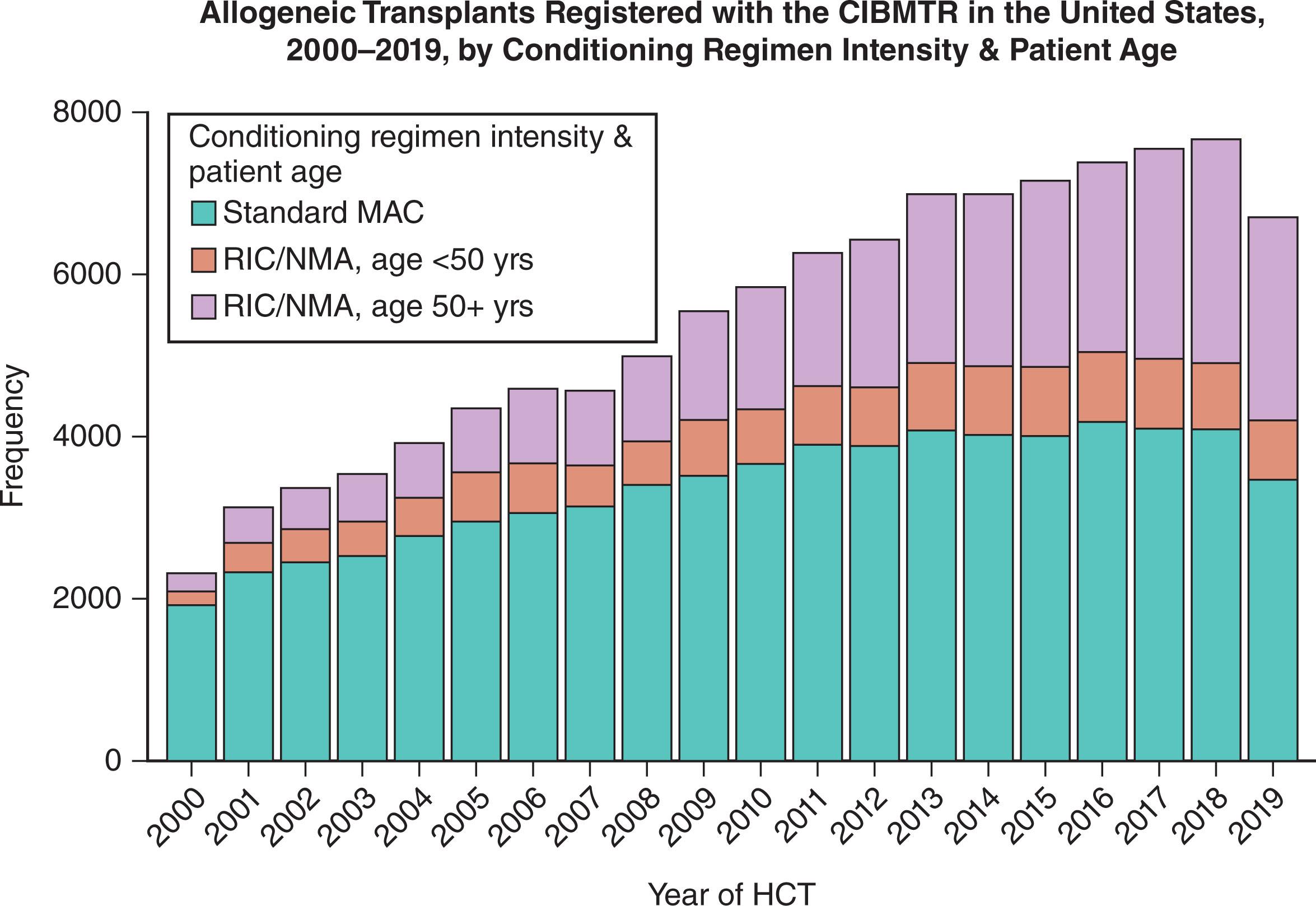
Toxicity associated with MAC regimens can be minimized and efficacy can be improved with careful pharmacokinetic monitoring of certain drugs, for example, busulfan. Another strategy for lowering NRM is reducing the dose-intensity of the conditioning regimen. This approach uses lower doses of cytotoxic drugs and/or radiation to facilitate donor cell engraftment and relies more on GVM effects to eradicate malignant cells. The lower doses of cytotoxic agents produce less host tissue damage and inflammatory cytokine secretion, resulting in lower rates of regimen-related morbidity and mortality. In patients ineligible for traditional MAC regimens, the use of RIC regimens has greatly increased the applicability of allogeneic HCT because of age or comorbidities. The development of RIC regimens has led to a substantial increase in the utilization of HCT in older patients ( Fig. 105.2 ).
Consensus criteria developed by the CIBMTR and the European Society for Blood and Marrow Transplantation (EBMT) distinguish between myeloablative, reduced intensity and nonmyeloablative regimens based on the likelihood of the regimen to produce toxicity in the recipient marrow ( Table 105.1 ). MAC regimens produce profound pancytopenia and are usually fatal in the absence of stem cell rescue. Nonmyeloablative regimens cause brief and often less severe pancytopenia, and in the absence of donor stem cell rescue, autologous hematopoietic recovery is likely to occur. RIC regimens are an intermediate category that does not fit well in either of the above, since they produce pancytopenia that may recover without stem cell rescue. RIC regimens induce less immune compromise in the immediate post-HCT setting as the duration and depth of neutropenia are reduced and host-derived immunocompetent cells are not immediately eliminated.
| Myeloablative Conditioning |
| Profound Cytopenia, Not Likely to Recover Without Hematopoietic Cell Rescue |
|
| Nonmyeloablative Conditioning |
| Minimal Cytopenia, Autologous Recovery of Hematopoiesis Likely Even Without Transplant |
|
| Reduced Intensity Conditioning |
|
It is generally accepted that RIC regimens allow HCT in some patients who are ineligible or not offered HCT with MAC. For example, in the United States, the proportion of transplants performed in patients 60 years and older increased from less than 5% before 2000, to ~34% in 2018. Two-thirds of the latter patients received RIC regimens. However, RIC regimens are increasingly used in patients of all ages who receive both related and unrelated donor transplants, as is shown in Fig. 105.2 . Despite the growing popularity of RIC regimens, large retrospective database studies from the EBMT and CIBMTR (summarized in Table 105.2 ) have generally failed to show a definite survival advantage resulting from the use of such conditioning regimens. Although RIC regimens allow a potent graft-versus-leukemia response to occur with lower toxicity, there are concerns about a higher risk of disease relapse following RIC regimens. Since the distribution of conditioning regimens in registry studies reflects physician choice or patient selection bias, retrospective data are of limited value and randomized trials have addressed this question. The prospective US Bone Marrow Transplant Clinical Trial Network (BMT CTN) 0901 trial randomized patients with myeloid malignancies eligible for myeloablative conditioning to RIC versus MAC regimens. In this trial, a superior relapse-free survival was evident for MAC after enrolling 272 out of the planned 356 patients, leading to early closure of the study. Notably, an overall survival (OS) advantage did not emerge. A prospective randomized European trial (RICMAC) showed similar 2-year, relapse-free, and overall survival for busulfan-based RIC versus MAC in patients with MDS and secondary AML.
| Group | Disease | Donor | RIC vs. MAC ( N ) | NRM RIC vs. MAC | Relapse | Comments |
|---|---|---|---|---|---|---|
| EBMT | MDS or sAML, >50 years | UD 39% | 833 vs. 500 | 32% vs. 44% at 4 years | 41% vs. 33% | Survival 31% at 4 years. RIC predicted for greater relapse but lower NRM. |
| EBMT | AML, >50 years | Sibling | 315 vs. 407 | 18% vs. 32% at 2 years | 41% vs. 34% | No difference in leukemia-free and overall survival between RIC and. MAC. |
| EBMT | MM | MUD 12% | 320 vs. 196 | 24% vs. 37% at 2 years | 27% vs. 54% | NRM was lower after RIC but relapse risk was double. |
| EBMT | AML | Sibling | 215 vs. 621 | 22% vs. 32% at 3 years | 45% vs. 27% | Relapse rate higher and NRM lower in RIC but OS similar (41% vs. 45%) in both groups. |
| EBMT | CLL | MUD 22% | 73 vs. 82 | 19% vs. 26% | 28% vs. 11% | Similar NRM but higher relapse risk observed after RIC. |
| EBMT | HL | MUD 13% | 89 vs. 79 | 23% vs. 46% at 1 year | 57% vs. 30% | Relapse rate was higher and NRM lower in RIC but OS was similar. |
| CIBMTR | Follicular NHL | Sibling | 88 vs. 120 | 23% in both at 1 year | 17% vs. 8% | RIC associated with higher risk of relapse but similar NRM while lower KPS impacted on NRM. OS was similar. |
| EBMT | ALL | Sibling | 127 vs. 449 | 21% vs. 29% | 32% vs. 38% | NRM lower after RIC but higher relapse rate. Leukemia-free survival similar to MAC. |
| EBMT | AML | MUD | 401 vs. 1154 | <50 years: 25% vs. 27%;≥50 years: 25% vs. 39% at 2 years | <50 years: 38% vs. 30%;≥50 years: 42% vs. 29% | RIC (vs. MAC) was associated with higher relapse <50 years and decreased NRM ≥50 years. Leukemia-free survival was similar after both RIC and MAC, regardless of age. |
| CIBMTR | AML/MDS | MUD/Sibling | 1448 vs. 3731 | 3-year NRM similar | Lower risk of relapse in myeloablative | Overall and disease-free survival was highest for myeloablative group. |
| CIBMTR | CML, 18–60 years | MUD/Sibling | 191 vs. 1204 | 29% vs. 32% at 5 years | 25% vs. 26% | Similar leukemia-free and overall survival and lower chronic GVHD risk with RIC vs. MAC in TKI era. |
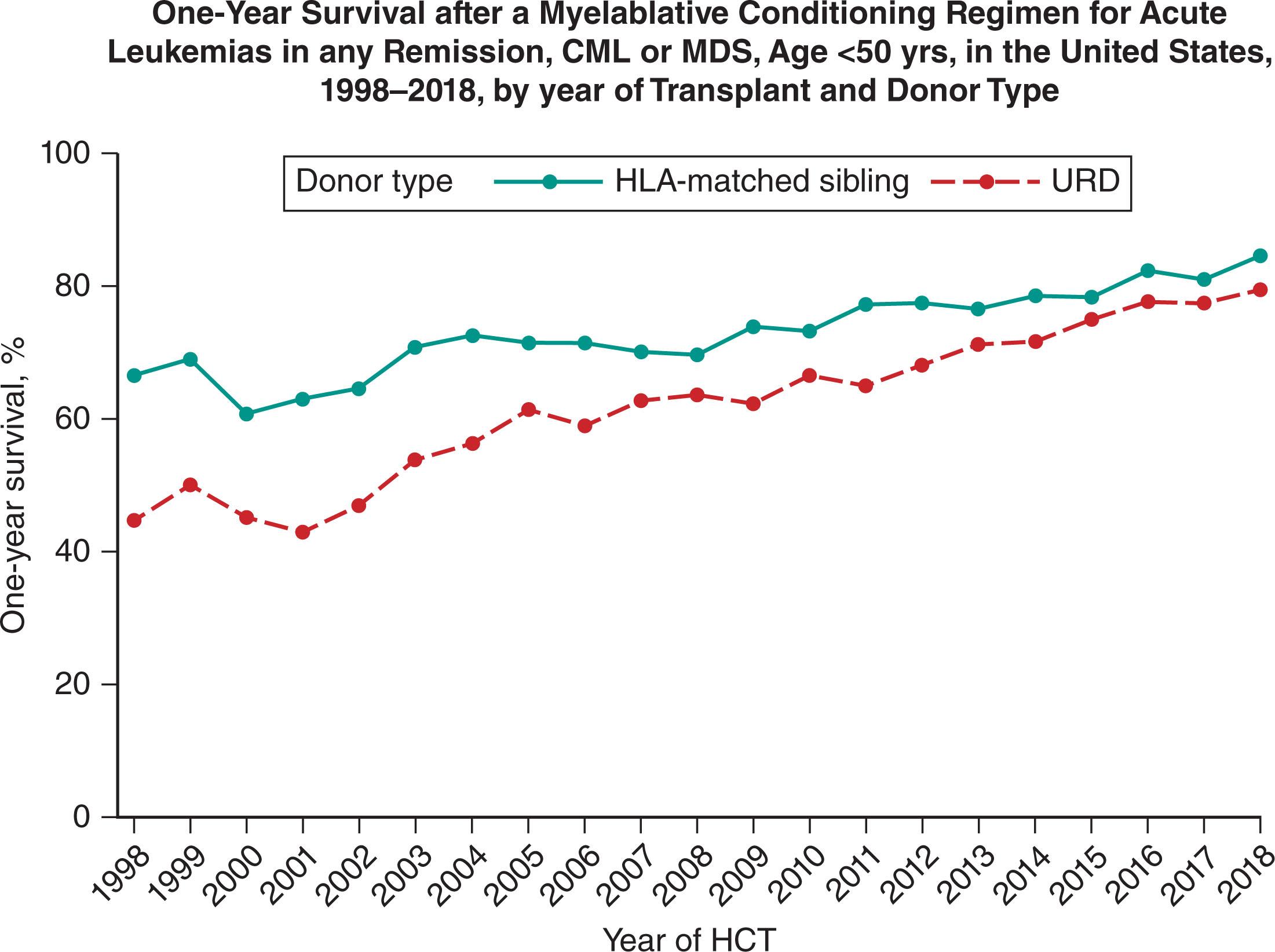
NRM rates are generally lower after HLA-identical sibling than after unrelated donor or alternative donor transplants because of less graft failure, faster immune reconstitution, and less GVHD. However, considerable progress has been made in reducing NRM rates after both HLA-identical sibling and alternative donor HCT. For matched sibling donor HCT (for AML in CR1), the incidence of NRM at 1 year decreased from 23% from 1985 to 1989, to about 11% from 2000 to 2004, and down to 6.3% in 2018. The 1-year incidence of NRM for unrelated donor HCT (for AML in CR1) from 1990 to 1994 was 34%, which decreased to 26% from 2000 to 2004, and down to 9.5% in 2018. Among alternative donor transplants, those from more closely HLA-matched donors tend to have lower risks of GVHD and NRM. Donor-recipient HLA mismatching is associated with increased risk of posttransplant complications, including graft rejection, acute and chronic GVHD, and mortality; risks increase progressively with multiple HLA mismatches. With modern molecular HLA typing techniques (allowing selection of more closely HLA-matched donors) and current GVHD prevention strategies, the difference in outcomes between HLA-matched sibling and unrelated donor transplantation has narrowed ( Fig. 105.3 ). Adoption of molecularly defined, HLA matching techniques, calcineurin inhibitor–based GVHD prophylaxis, fungal prophylaxis with azoles, leukocyte reduction of blood products, newer assays for viral reactivation, pharmacokinetic testing of conditioning agents, and posttransplant cyclophosphamide for induction of allogeneic tolerance are some of the major innovations that have impacted NRM.
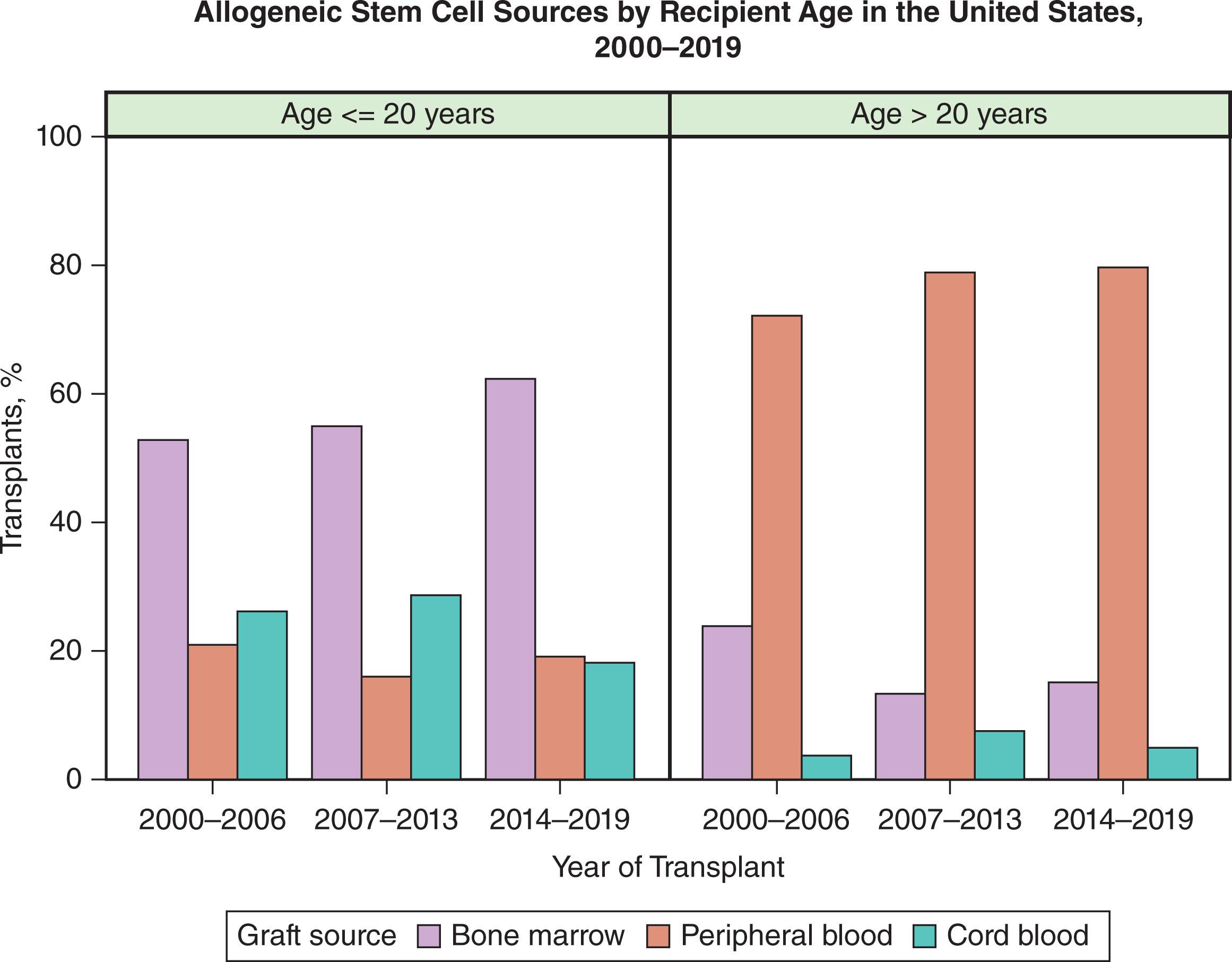
The sources of hematopoietic cells for transplantation, historically bone marrow from donors, now also include peripheral blood hematopoietic cells, collected by leukapheresis and umbilical cord blood. The composition of grafts from bone marrow, peripheral blood, and cord blood varies in terms of the proportion of pluripotent stem cells, the proportion of lineage-committed late progenitor cells, and in the proportion and characteristics of immune-reactive cells. Bone marrow is the primary source of allogeneic donor cells for transplantation in children, and peripheral blood is the primary source in adults ( Fig. 105.4 ).
Several randomized trials have compared matched-sibling bone marrow versus peripheral blood grafts in patients with hematologic malignancy, following MAC regimens. In general, these studies showed no difference in the rates of acute GVHD between the two graft sources and showed no difference between higher risk of chronic GVHD with peripheral blood grafts. While survival outcomes were similar in most studies, the US and Canadian randomized studies reported a disease-free and overall survival advantage, respectively, favoring peripheral blood grafts. A meta-analysis, using individual patient-level data from nine randomized trials of related donor peripheral blood versus bone marrow transplants suggested that patients receiving peripheral blood grafts had faster hematopoietic recovery, a lower relapse rate if transplanted for hematologic malignancy, and higher overall and disease-free survival if transplanted for advanced-stage disease. However, peripheral blood was also associated with a significantly increased risk of extensive chronic GVHD. Among unrelated donor transplant recipients, the prospective randomized BMT-CTN 0201 trial showed a higher risk of chronic GVHD in patients receiving peripheral blood grafts (53% versus 41% for marrow grafts). Notably, survival and the incidence of relapse and acute GVHD were similar, while graft failure was more common among recipients of marrow grafts. The relative importance of graft sources in patients receiving lower-intensity conditioning is not known, but a CIBMTR study comparing unrelated bone marrow versus peripheral blood grafts, following RIC, showed no difference between the two sources in terms of rates of acute or chronic GVHD, relapse risk, and survival outcomes.
While donor-derived alloimmunity in the form of a graft versus tumor effect leads to tumor control, the same phenomenon directed against normal host tissues leads to GVHD, which is a major determinant of NRM after allogeneic transplantation. The major criterion for selecting an allogeneic donor is the degree of histocompatibility between the donor and recipient because the risks of both graft rejection and GVHD increase with the degree of genetic disparity. Alloreactivity is reduced by matching recipients and donors at loci in the major histocompatibility complex (MHC), including HLA that is encoded by class I ( HLA-A , HLA-B , and HLA-C ) and class II ( HLA-DR , HLA-DQ , and HLA-DP ) genes. HLA molecules were originally defined by serology, but DNA-based, high-resolution testing is now routine. Even in the setting of MHC-matched, donor-recipient pairs, minor histocompatibility antigen (MiHA) (cell surface peptides found in association with class I or II MHC molecules) differences that are detectable by T cells can stimulate an MHC-restricted, alloreactive response, resulting in GVHD. The optimal donor is a sibling sharing HLA class I and HLA class II alleles, but matched sibling donors are available for only about 30% of patients.
For unrelated donor HCT, the primary driver for successful outcome is the degree of donor-recipient HLA matching. In 1986, the National Marrow Donor Program (NMDP; “Be the Match Registry”) was established as a repository for HLA typing information so that unrelated donors and recipients could be adequately matched. The NMDP HapLogic donor search considers over 20 million donors (87% typed for HLA-A, HLA-B, and HLA-DR) and additionally provides a match report of an additional 13 million donors listed in World Marrow Donor Association Search and Match. Such a large number of donors is necessary because great diversity exists in the HLA system, with over 5500 class I alleles ( HLA-A, -B , and -C ) and over 1600 class II alleles ( HLA-DRB1 and -DQB1 ), resulting in several million potential HLA combinations. The likelihood of finding an optimal adult unrelated donor (i.e., a donor matched at high resolution at HLA-A, HLA-B, HLA-C , and -DRB1 alleles or a “8/8 match”) varies among racial and ethnic groups, depending on the size and composition of unrelated donor registries. Within the US population, the highest likelihood for finding an optimal donor is 75% for White people of European descent, and the lowest is 16% among Black people of South or Central American descent. The development of large donor registries has expanded access to transplantation, as well as increasing the likelihood that a recipient will find a well-matched donor. However, this also means that patients who do not find a suitably matched donor in the large registry pool have rare HLA genotypes for whom waiting for a fully matched donor from among new additions recruited to the donor pool is not recommended. Such patients should proceed to alternative donor transplantation with partially matched sources; haploidentical or cord blood donor grafts.
The adoption of high-resolution HLA typing for matching and selection of unrelated donors, have been associated with improved outcomes. A study examining unrelated donor characteristics predictive of outcomes reported that after adjusting for the disease and comorbidities, when the donor was a 10/10 match (matched for HLA-A, -B, -C, -DRB1 , and -DQB1 ). Age is the most important factor, after donor-recipient HLA match: survival was significantly improved if the donor was young (aged 18 to 32 years). A 5.5% increase occurred in the hazard for overall mortality for every 10-year increment in donor age. If multiple 8/8 matched unrelated donors are available, other factors could be considered, such as donor age, matching at DPB1 or permissive DPB1 mismatching, avoidance of donor allotypes targeted by donor-specific antibodies in the recipient, and blood group or CMV-status matching. With current high-resolution HLA typing and donor selection, unrelated donor transplants have survival comparable to that of matched sibling donor setting.
For patients lacking a matched sibling or 8/8 matched unrelated donors, the options are a mismatched and unrelated donor, a haploidentical-related donor, or a cord-blood unit (collectively denoted as “alternative donors”). Each choice has benefits and disadvantages ( Table 105.3 ). As a source of donor hematopoietic cells, umbilical cord blood offers several advantages. It is readily available as cryopreserved units, entails no risk to the donor and the HLA-matching criteria for cord blood transplantation need not be as stringent as for adult donor transplantation. Hence, mismatched cord blood units, at one or two HLA loci, are available for almost all patients less than 20 years of age and for more than 80% of patients ≥20 years of age, regardless of racial and ethnic background. Drawbacks of cord blood transplantation include procurement costs, such as the fixed and often limited dose of hematopoietic cells (based on recipient body weight) in each cord blood unit and relatively high rates of NRM. However, double cord blood transplantation, with each unit sharing at least 4/6 HLA antigens with the recipient, has been shown to overcome the problem of dose and extend the use of cord blood transplant to adult patients. Other approaches to facilitate engraftment with limited cord blood cell doses, including ex vivo cell expansion techniques, are in clinical trials.
| Mismatched Unrelated Donor | Haploidentical Donor | Cord | |
|---|---|---|---|
| Availability | Over 80% | Over 95% | Over 80% |
| Time to procure | 1–4 months | Immediate | 2–5 days |
| Engraftment | Over 95% | Over 95% | Over 90% with slower engraftment |
| GVHD | Moderate | More genetic disparity but moderate with most modern regimens | Moderate—may be less acute but chronic similar |
| Availability donor for posttransplant immune therapy | Usually, but takes 2–4 weeks | Yes | No |
| Relative cost | Moderate | Low if unmanipulated product. Moderate if ex vivo selection | Moderate (1 unit) or high (2 units) |
| Risk of relapse | Moderate | Higher with regimens that are effective in preventing GVHD | Moderate |
HLA haploidentical-related donor HCT is another option for patients without matched siblings or unrelated donors. Haploidentical donors are usually parents, siblings, or children of patients who are mismatched at ≥2 loci HLA-A, HLA-B, HLA-C , and HLA-DRB1 . Historically, T-cell-replete haploidentical HCT was prohibited by severe GVHD and NRM, approaching 50%. Haploidentical HCT have been made significantly safer by the administration of high-dose cyclophosphamide after transplantation (posttransplant CY), which promotes tolerance by elimination of alloreactive host and donor T cells, leading to suppression of graft rejection and GVHD, without toxicity to donor hematopoietic cells. Immediate and near-universal donor availability and theoretically lower costs are advantages of haploidentical grafts. Several retrospective registry analyses suggest haploidentical HCT, performed using T-cell-replete grafts and post-transplant cyclophosphamide, achieves outcomes comparable with those of transplantation performed using matched related or unrelated donors. An increased risk of NRM has been suggested in patients receiving haploidentical HCT, using posttransplant CY compared with matched sibling donor HCT and calcineurin-inhibitor-based or posttransplant cyclophosphamide-based GVHD prophylaxis. These data caution against using haploidentical-related donors in lieu of adult, matched-related donors outside of a clinical trial.
In patients lacking adult, 8/8-matched (sibling or unrelated) donors, the choice between cord blood versus haploidentical HCT has been a matter of much debate. The phase III randomized BMT-CTN 1101 study compared double umbilical cord blood versus haploidentical marrow grafts and reported that NRM and overall survival at 2 years were superior in patients who received haploidentical marrow transplantation, while there was no significant difference in the primary endpoint of progression-free survival between the two types of transplant. Other techniques for facilitating haploidentical transplants have been developed around the world that involve combinations of selective T-cell depletion ex vivo, mega dose infusion of CD34 progenitors, or induction of immune tolerance with G-CSF and anti-thymocyte globulin (ATG).
In a minority of patients, especially those with donor-specific, anti-HLA antibodies (DSAs), appropriate cord and haploidentical donors may be unavailable. Unrelated donor grafts, mismatched at more than one allele, have now emerged as an alternative source in the context of post-transplant CY-based GVHD prophylaxis, similar to haploidentical-related donor HCT. A single-center study among recipients of nonmyeloablative conditioning for HCT from mismatched unrelated donors (majority at two or more loci), using posttransplant CY/sirolimus and mycophenolate as GVHD prophylaxis, demonstrated a promising 2-year NRM and overall survival of 6% and 67%, respectively.
The combination of a calcineurin inhibitor, such as cyclosporine, tacrolimus, or methotrexate, has been the mainstay of GVHD prevention, after allogeneic HCT. For RIC regimens, an acceptable alternative is a combination of a calcineurin inhibitor and mycophenolate mofetil. Despite GVHD prophylaxis, over 50% of allogeneic HCT recipients will develop acute and/or chronic GVHD. Studies have demonstrated that in vivo T-cell depletion with anti-thymocyte ATG can reduce chronic GVHD, though the effect on survival has been questioned. Prospective phase III randomized trials have compared the use of ATG as part of GVHD prophylaxis in unrelated and related donor HCT and generally suggest lower rates of acute and/or chronic GVHD, without an impact on relapse, survival, or NRM. Comparisons are difficult due to differences in clinical trial designs, potency, dosage of ATG preparations due to different production methods, and absolute lymphocyte count at the time of ATG administration.
Administration of cyclophosphamide after HCT has moved from early use in the haploidentical HCT setting to the HLA-matched, related and unrelated donor HCT settings. A prospective phase III randomized HOVON-96 trial done with recipients of matched-donor grafts in the RIC setting reported a significant reduction in both acute and chronic GVHD and 1-year GVHD-free and relapse-free survival with the use of post-transplant cyclophosphamide, without any difference in progression-free and overall survival. The control arm in this study utilized cyclosporine and mycophenolate, which precludes comparison with the more common methotrexate-based GVHD prophylaxis approach, after RIC transplantation. A phase II randomized BMT CTN 1203 trial also suggested improved GVHD-free and relapse-free survival, along with lower risk of severe acute and chronic GVHD for post-transplant, CY-based GVHD prophylaxis regimen in RIC HCT, compared with non-randomized contemporaneous controls. A large randomized trial of post-transplant cyclophosphamide versus the current standard of tacrolimus and methotrexate is now enrolling patients (BMT CTN 1703).
At the time of transplant, disease remission status is a strong predictor of survival post transplantation for hematologic malignancies. Evaluation of measurable or minimal residual disease (MRD) status, using sensitive techniques (multiparameter flow cytometry, sequencing), is one of the most important established prognostic tools in ALL and is now emerging to be an important predictive and prognostic marker in other hematologic malignancies, such as AML, myeloma, and B-cell lymphomas. In ALL, MRD is present in up to 30% to 50% patients in a traditional CR. Consideration of MRD impacts several clinical decisions in HCT. Among these are: assessing the suitability of proceeding to HCT versus additional consolidative therapy in patients who achieve a traditional CR but with residual MRD, the intensity of conditioning regimen used for HCT (RIC versus MAC), the role of pre-emptive posttransplant therapy to address relapse risk, and the need for HCT in those with an MRD-negative remission.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here