Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
All esophagectomy techniques involve partial or complete resection of the esophagus with a new anastomosis to esophagus, stomach, or bowel. Benign indications include esophageal perforation (iatrogenic from endoscopy/biopsy/balloon dilation, traumatic or self-induced from Boerhaave syndrome), refractory strictures from peptic ulcers/radiation/caustic ingestion, and esophageal fistulas (congenital or iatrogenic from trachea or bronchi). The most common malignant causes include adenocarcinoma and squamous cell carcinoma of the esophagus.
Right-sided transthoracic esophagectomy is preferred when the upper two-thirds of the esophagus is involved given the aorta would otherwise limit access, whereas a left-sided approach can be used when the distal esophagus is involved.
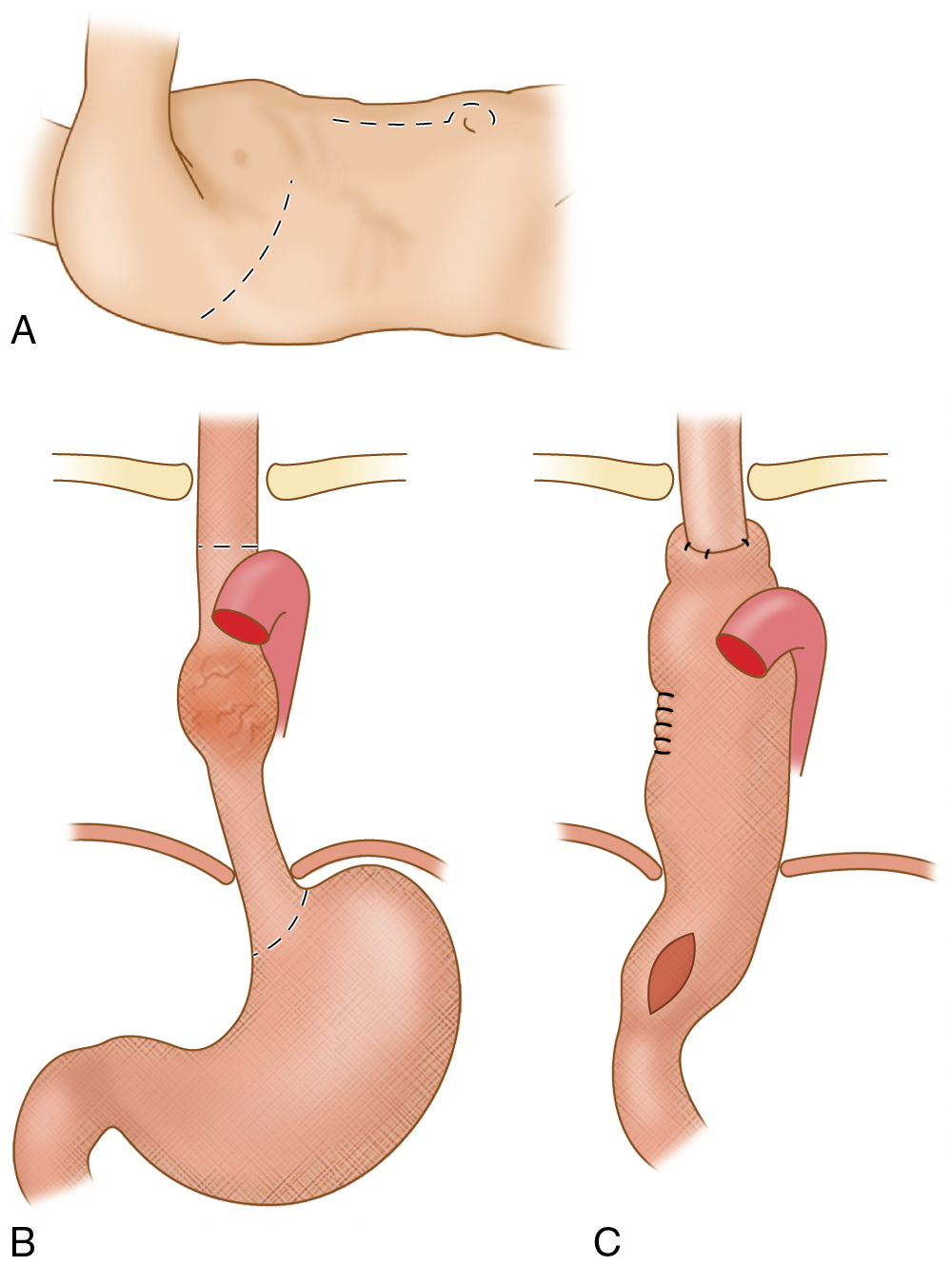
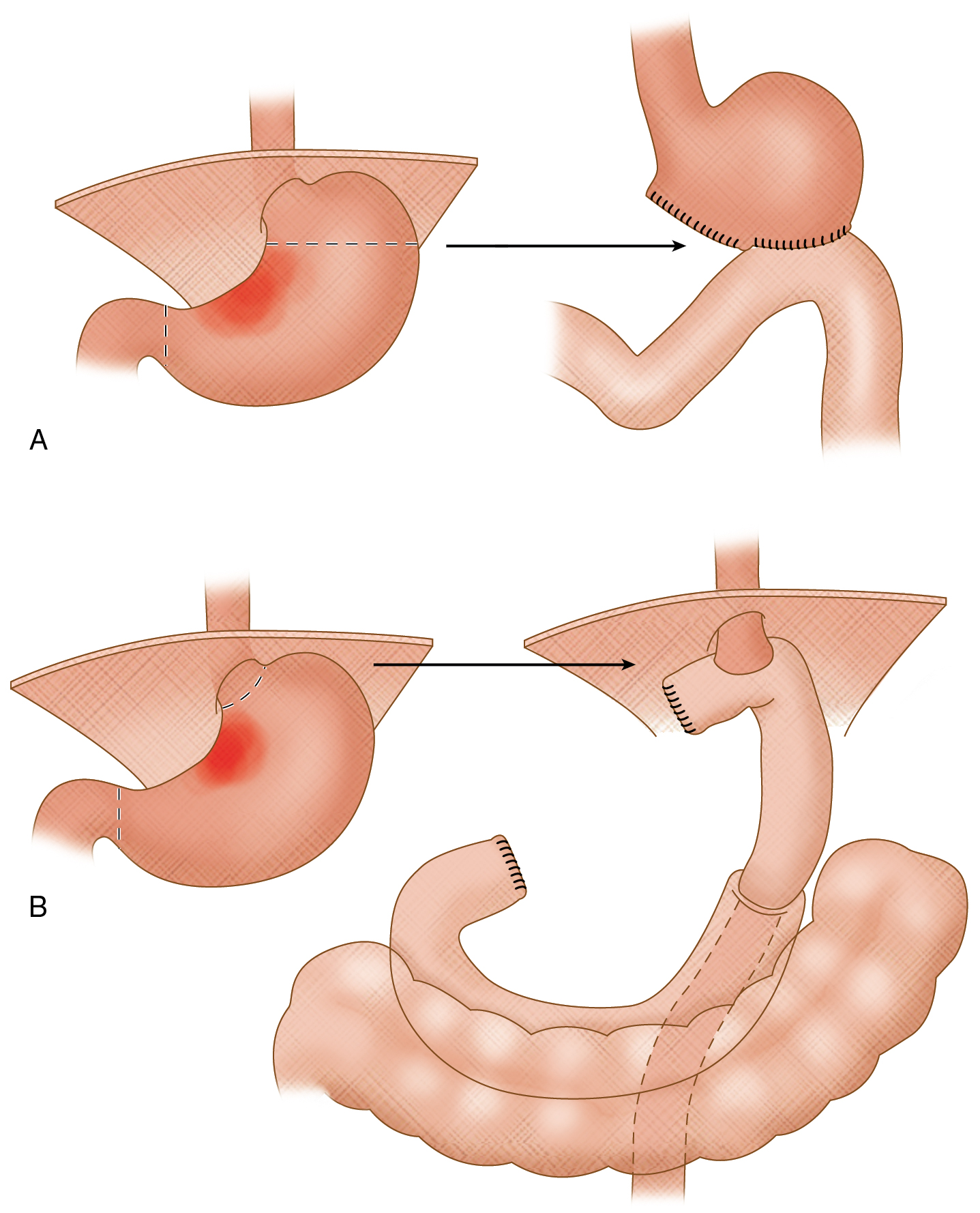
The Ivor-Lewis technique is best for pathology of the mid-esophagus and combines a laparotomy with right thoracotomy and intrathoracic anastomosis ( Fig. 7.1 ).
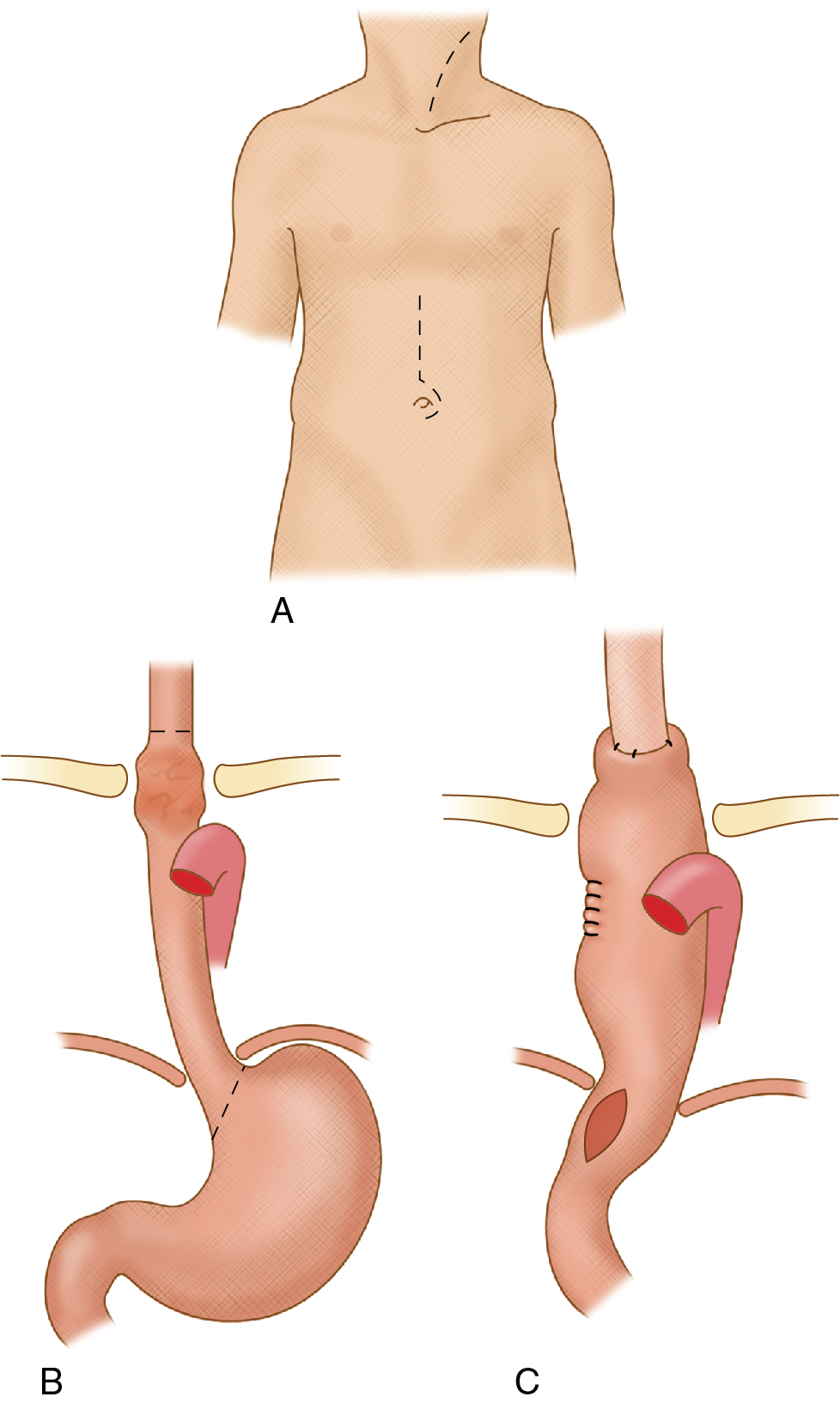
Transhiatal esophagectomy was developed because of complications from the transthoracic approach in treating long segment pathology. It involves mobilizing the esophagus through the esophageal hiatus, after which the entire esophagus is transected and the stomach is pulled up and anastomosed to the cervical esophageal remnant ( Fig. 7.2 ).
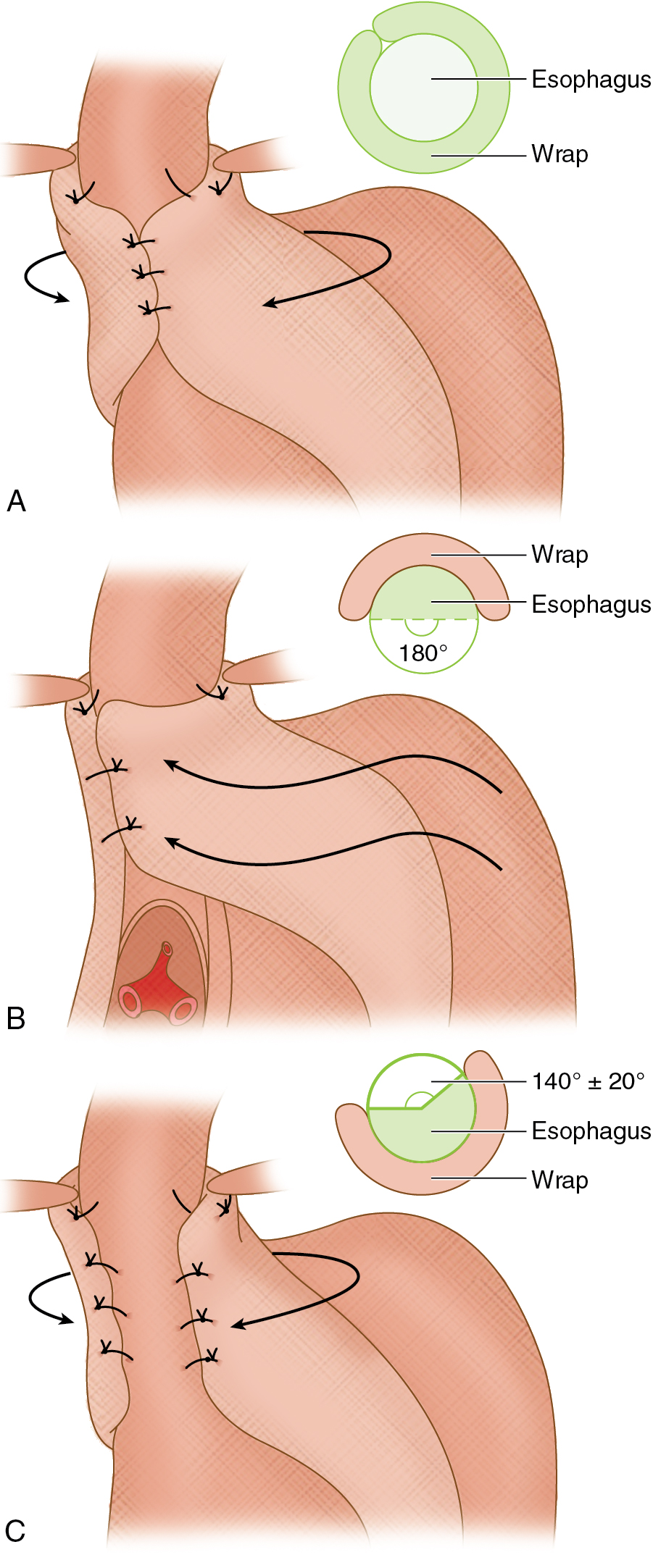
The idea behind antireflux surgery is to create a valve-mechanism to reestablish gastroesophageal junction competence ( Fig. 7.3 ). When associated with a sliding or paraesophageal hernia greater than 5 cm, this too will need to be corrected by approximating the pillars of the diaphragm crura posterior and inferior to the esophagus. In more severe cases, an anterior abdominal wall gastropexy can be performed to reduce the risk of hernia recurrence. Indications for antireflux surgery include gastroesophageal reflux disease refractory to medical treatment, severe esophagitis by endoscopy, benign stricture, or early Barrett esophagus without concerning features. Relative contraindications include severe esophageal dysmotility and achalasia. The most common techniques require a normal length esophagus, and the technique of choice then depends on the patient’s esophageal motility and gastric emptying (the fundus and upper body of the stomach are responsible for gastric emptying, and underlying gastroparesis may worsen with fundoplication, which may be prevented with concurrent pyloroplasty at the time of surgery).
The Nissen fundoplication is preferred when the esophagus and stomach are normal in motility, and can be performed via laparotomy or laparoscopically. It uses the stomach fundus and wraps it around the distal esophagus 360 degrees before being sutured in place.
Partial (i.e., Toupet) fundoplication techniques are best when there are underlying issues with esophageal and/or gastric motility. These procedures incompletely wrap the fundus around the distal esophagus to avoid worsening the underlying esophageal/gastric motility but at the same time provide some degree of reflux prevention. As such, these do not perform as well long term and have higher rates of reflux recurrence.
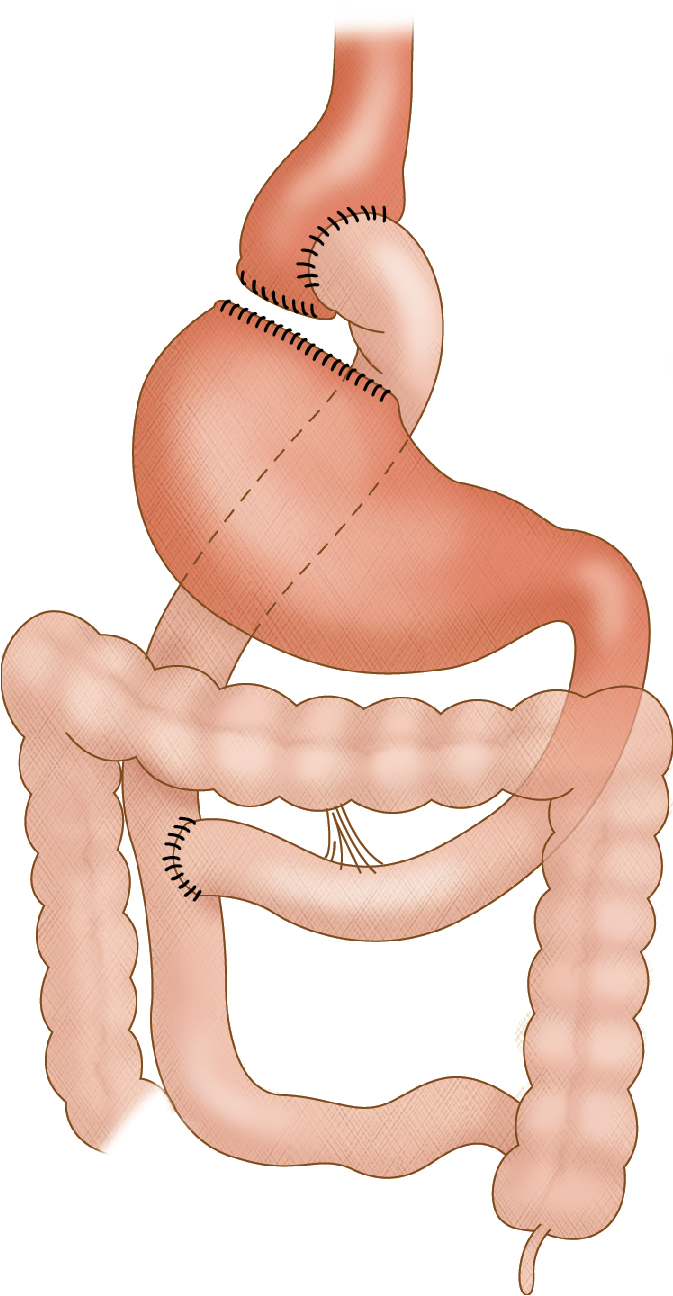
Bariatric surgeries are typically reserved for the morbidly obese (body mass index >40 kg/m 2 , or 35 kg/m 2 with comorbidities) to improve quality of life and comorbidities (such as heart disease, sleep apnea, and diabetes). Restrictive procedures, such as vertical banded gastropexy, gastric sleeve, and gastric banding serve to reduce caloric intake by limiting gastric capacity. Malabsorptive procedures, such as jejunoileal bypass and biliopancreatic diversion with duodenal switch reduce the absorption of calories by decreasing the length of the small intestine. Roux-en-Y gastric bypass combines both principles by limiting caloric intake with a gastric pouch and reducing absorption through a gastrojejunal component.
Roux-en-Y gastric bypass is typically the preferred method owing to decreased hospital stays and faster recovery. Preoperative planning for this procedure must include exclusion of underlying malignancy or inflammatory bowel disease (IBD), as well as confirming normal anatomy of the proximal gastrointestinal (GI) tract via fluoroscopy (i.e., an upper GI study). For postoperative imaging purposes, the four suture lines to consider are that of the gastric pouch (when the fundus is transected), the gastrojejunal anastomosis to the gastric pouch, the transected fundus of the remaining stomach, and the jejunojejunostomy. The Y-limb (i.e., afferent or pancreaticobiliary limb) consists of the excluded stomach, duodenum, and proximal jejunum ending at the jejunojejunostomy, and the Roux-limb (i.e., efferent or antegrade limb) includes the gastric pouch and anastomosed jejunum to the level of the jejunojejunostomy ( Fig. 7.4 ).
Gastric surgeries are performed for both benign and malignant conditions. The location of the pathology will usually dictate which type of surgery is best.
For small tumors or severe ulcerative disease in the distal two-thirds of the stomach, a partial gastrectomy (i.e., antrectomy) may be a viable option; either a Billroth I or II reanastomosis is commonly used to restore the enteric anatomy. The Billroth I procedure involves an antrectomy and an end-to-end anastomosis between the remnant stomach and the duodenum. In the Billroth II operation, after the antrectomy is performed, the duodenal stump is closed and a gastrojejunal anastomosis or a side-to-side duodenojejunal anastomosis is created.
Total gastrectomy is typically reserved for severe and diffuse ulcerative disease with complications (perforation or strictures), for tumors in the proximal third of the stomach or which are infiltrative, or for large mid-gastric tumors. For these cases, a Roux-en-Y esophagojejunostomy with end-to-side anastomosis is created, with the Y-limb including the duodenum and proximal jejunum and the Roux-limb beginning at the esophagojejunal anastomosis and continuing distally ( Fig. 7.5 ).
For patients who present with a malignancy of the pancreatic head (classically adenocarcinoma, less commonly metastases, or cholangiocarcinoma), patients who require management of pancreatic or duodenal trauma, or for refractory cases of chronic pancreatitis, a Whipple procedure (also known as a pancreaticoduodenectomy) can be performed to either extend the patient’s life expectancy or improve quality of life. If performed because of a malignancy, potential contraindications to surgery include whether or not there is more than 180-degree tumor encasement of important adjacent structures (such as the celiac trunk, superior mesenteric artery, superior mesenteric vein, or inferior mesenteric vein), or the presence of distant metastatic disease.
The procedure itself (most commonly) involves resection of the gastric antrum, entire duodenum, the pancreatic head, common bile duct, gallbladder, and first 15 cm of jejunum. From there, the new anastomoses that are reconstructed include a gastrojejunostomy (involving mid-jejunum), a pancreaticojejunostomy (end-to-side anastomosis with the proximal jejunal stump), and a choledochojejunostomy (found between the prior two anastomoses).
There are both benign and malignant reasons to perform surgery on the small bowel, colon and/or rectum. The type of surgery depends on location and extent of disease.
Some of the indications for small bowel (and colon) surgery include refractory irritable bowel disease, strictures, perforations, trauma, malignancy, obstruction, volvulus, infarction, and fistulas. Usually only the affected portion of bowel is resected, with subsequent reanastomosis of the two ends. On occasion (especially if there is extensive inflammation or concern for infection around the surgical field at the time of initial resection), a temporizing diverting ileostomy or colostomy may be performed to help the injured bowel recover before subsequent reanastomosis and ostomy takedown at a later date.
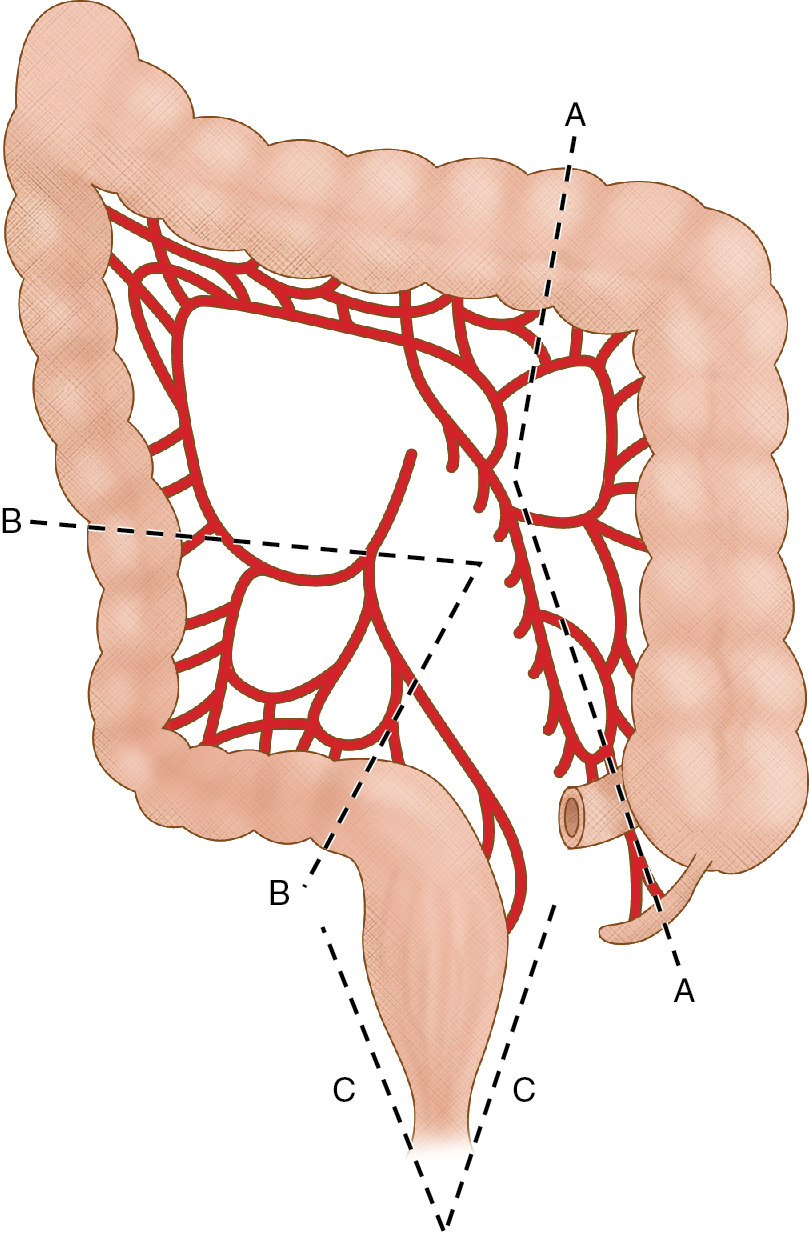
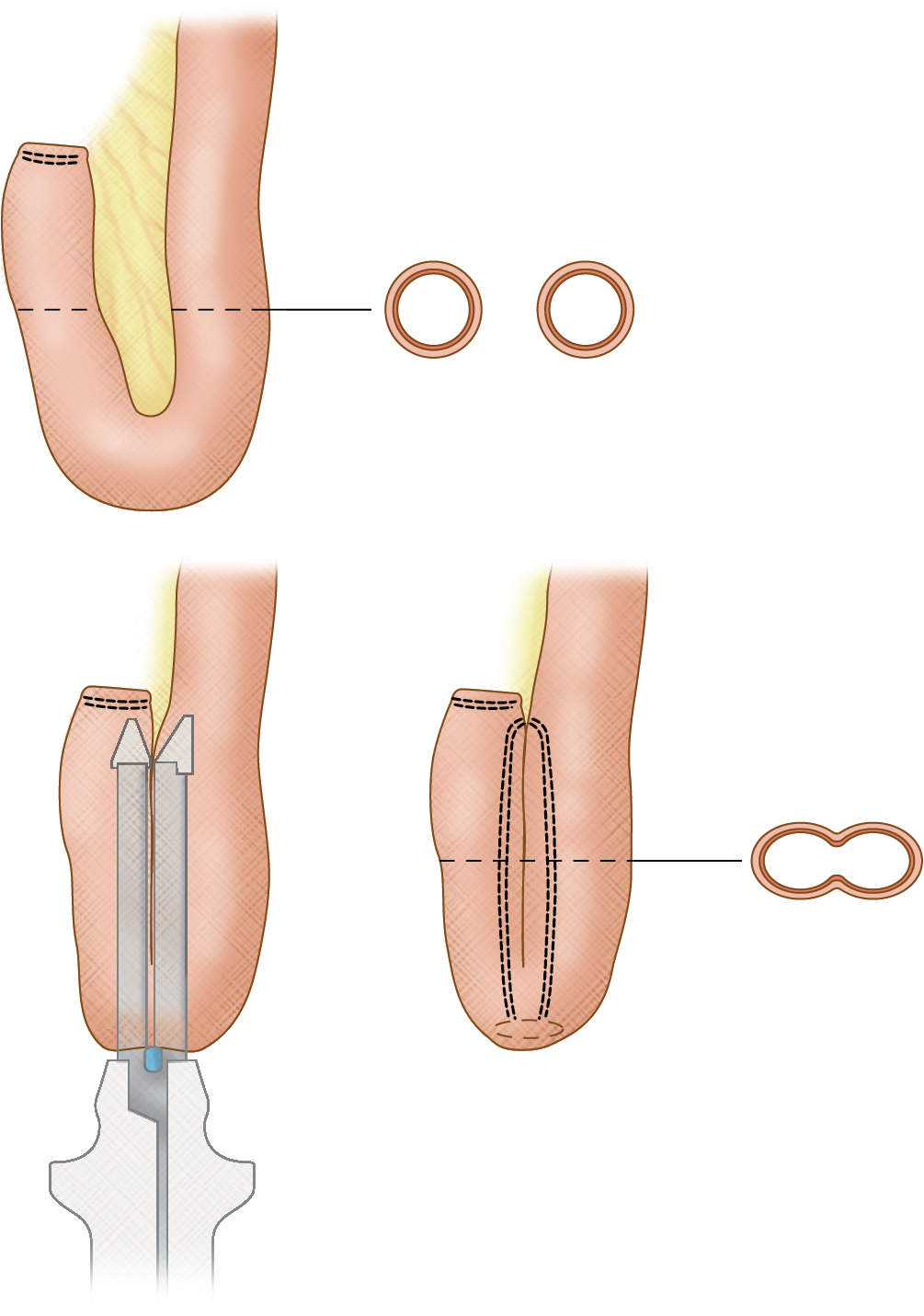
Indications for surgery particular to the colon include complicated diverticulitis, toxic megacolon, severe colitis, and refractory lower GI bleeds. Either part of or the entire colon may need to be resected depending on the etiology ( Fig. 7.6 ), and in the most extreme of cases a total proctocolectomy is performed, which removes the colon and rectum (this can be followed by an ileal J-pouch with anal anastomosis ( Fig. 7.7 ) or an end ileostomy). If only a section of colon is removed and primarily reanastomosed, a temporizing diverting loop ileostomy may also be performed to help the colon heal, and later reversed. If a section of colon needs to be bypassed, an end colostomy can be performed (and later reversed if the obstruction is relieved).
Surgeries involving the rectum are primarily for the treatment of rectal carcinoma. Magnetic resonance imaging (MRI) is used to stage the extent of local disease in the pelvis, with surgical options, including local excision, sphincter-preserving resection (i.e., low anterior resection) followed by reanastomosis, or abdominoperineal resection (most aggressive approach) followed by an end colostomy or ileostomy.
Indications for cystectomy include underlying malignancies, such as muscle invasive urothelial carcinoma (and less frequently adenocarcinoma from a urachal remnant or squamous cell carcinoma from chronic irritation), or palliation for pain/bleeding/urgency because of refractory hemorrhagic cystitis. The most commonly used bowel segments (depending on the procedure) include distal ileum, cecum, ascending colon, and occasionally sigmoid colon. In addition, there are both incontinent and continent urinary diversion procedures available necessitating special patient selection beforehand.
Incontinent diversions, such as the ileal conduit, allow continuous drainage of urine from a cutaneous stoma into a bag. Usually a short portion of distal ileum is resected, sparing the last 15 cm or so to preserve absorption of vitamin B12 and bile salts, and preserving the vascular pedicle. One end is then closed and anastomosed to the distal ureters, while the other is brought out as a cutaneous stoma (usually in the right lower quadrant).
Continent urinary diversions allow the patient to ambulate without having to wear a drainage bag. A continent cutaneous diversion creates a low-pressure reservoir (i.e., Indiana or Miami pouch) using the ascending colon, cecum, and short segment of distal ileum. The colon and cecum are detubularized and reconstructed into a “round” reservoir to which the distal ureters are then attached, and the ileal part is tapered and connects to the skin to act as a catheterizable channel while the ileocecal valve is intussuscepted to serve as the continence mechanism (alternatively, the native appendix can be used as the catheterizable channel and referred to as a Mitrofanoff procedure). If the native bladder neck can be spared after cystectomy, then an orthotopic neobladder may be an option by creating a similar reservoir as described above (typically using 50–60 cm of ileum), which is then anastomosed to the bladder neck remnant, allowing the patient to void by valsalva.
In all three procedure types, the GI tract that was left in discontinuity is reconstituted by primarily reanastomosing the ends of the resected bowel. Continent cutaneous diversions and neobladders require a much greater length of bowel than an ileal conduit, and patients will have to empty their reservoir or neobladder every 6 to 8 hours to prevent overdistention (the reconstructed bowel does not have the same innervation as the native bladder and therefore patients cannot always sense when they are “full”). Therefore patient selection is important when considering these approaches. In addition, the wall of the small or large bowel is much thinner than the native bladder wall and thus more prone to rupture. Lastly, these types of urinary diversion are also prone to stone formation, as well as any underlying bowel pathology (such as Crohn or adenocarcinoma) and should be closely inspected during routine follow-up imaging to avoid future complications.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here