Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Radiography remains the mainstay for the assessment of acute skeletal trauma with the exception of cervical spine trauma, which is now usually evaluated with CT. Properly positioned radiographs allow for accurate characterization of a large variety of appendicular skeletal injuries. Comparison radiographs of the asymptomatic side can be obtained with ease and may be useful, such as in pediatric cases and for assessment of subtle widening of the acromioclavicular interval. Localization of foreign bodies also remains as one of the important roles of radiography.
Major indications for CT include diagnosis and evaluation of fractures, particularly when presence of fractures can alter management. CT is superior to radiography in depicting the extent of fractures, the spatial relationship of the fracture fragments, and the presence of intraarticular fragments. Other indications include preoperative planning and evaluation of postoperative complications. Multiplanar reformatted (MPR) images allow for higher diagnostic accuracy than radiography or axial CT images alone. As a result, CT has largely replaced radiography in cervical spine and pelvic fracture evaluations. Its limitations include higher radiation dose and cost, although studies have demonstrated that CT is more cost effective than radiography to clear the cervical spine in high-risk patients. Evaluation of ligamentous injuries is also limited with CT.
MRI has the advantage of imaging injuries of soft tissue structures, including the labrum, ligaments, muscles, tendons, and cartilage, as well as the lack of radiation dose. It is also useful for the evaluation of occult hip fractures, particularly in older patients with osteoporosis. However, its limitations include higher cost and slower image acquisition.
At least two views of the fracture site, taken at 90 degrees to each other, are obtained. Remember, “one view equals no view.” The radiographs obtained should include joints immediately above and below the fractured area for evaluation of associated dislocations.
On radiographs and CT images, acute fractures demonstrate well-demarcated lucent fracture lines without sclerotic borders. As fractures heal, there is callus formation with fracture lines becoming less visible over time. On MRI, while lack of bone marrow edema associated with fracture deformity on fluid-sensitive sequences (such as T2-weighted and short tau inversion recovery ([STIR] images) is indicative of a chronic etiology, it is important to remember that bone marrow edema can persist for several months and thus is not always indicative of an acute etiology. Associated findings, such as soft tissue hematoma (typically high in signal intensity on T1-weighted images) and lipohemarthrosis (seen as layering fat that arises from the bone marrow and fluid/hemorrhage in the joint space, indicative of an intraarticular fracture), suggest a more acute etiology.
Closed fracture occurs when there is intact skin over the fracture site. If there is communication between the fracture site and the outside environment, it is considered an open fracture regardless of how small the overlying skin defect is.
Avulsion fracture occurs when an osseous fragment is pulled off at the site of insertion of a muscle, ligament, or tendon.
Comminuted fracture is a fracture with more than two fracture fragments.
Intraarticular fracture involves the articular surface of a bone adjacent to a joint.
Occult fracture is a fracture that is not visible on a radiograph.
Pathologic fracture is a fracture in abnormal bone weakened by a preexisting disease process such as malignancy.
Fracture displacement describes the offset of the distal fracture fragment relative to the proximal fragment. Both direction and amount of offset (usually described in terms of shaft width) are used for description.
Fracture angulation describes the direction of distal fracture fragment in relation to the proximal fragment away from expected alignment had the bone not been fractured. Medial angulation can be described as “varus,” and lateral angulation can be described as “valgus.” Alternatively, angulation can be described in terms of the direction toward which the apex of the angle between the two fracture fragments is pointing. For example, a fracture can either be described as having medial angulation of the distal fracture fragment or lateral apex angulation.
Stress fractures occur as a result of mismatch between bone strength and mechanical stress upon the bone and are subdivided into fatigue and insufficiency fractures. Fatigue fractures are the result of abnormal stresses on normal bone and are commonly seen in athletes. Insufficiency fractures are the result of normal stresses on abnormal bone, such as caused by conditions like osteoporosis, osteomalacia, or osteogenesis imperfecta. It should be noted, however, that some authors use the term stress fracture synonymously with fatigue fracture. Common sites for fatigue fractures include: pubic ramus, medial aspect of the femoral neck, tibia, calcaneus, navicular, metatarsal bones, and hallux sesamoid bones. Common sites for insufficiency fractures include: vertebra, sacrum, pubic ramus, femoral neck, and proximal diaphysis of the femur.
Dislocation is complete loss of contact between the articular surfaces of a joint. Subluxation is partial loss of congruity between the articular surfaces of a joint.
Various soft tissue injuries can be associated with fractures, which include neurovascular injuries. When a fracture is allowed to heal in an abnormal position, malunion occurs. If the fracture fragments fail to heal and fuse, the resulting complication is termed nonunion . If there is injury to the vascular supply to the bone, avascular necrosis can occur, such as from scaphoid waist and talar neck fractures. Osteomyelitis, which is infection of the bone, can also occur after a fracture, especially after an open fracture. Pseudoarthrosis refers to nonunion or false joint (as the name suggests), which is a result of failure of fracture healing. Myositis ossificans is extraosseous bone formation (heterotopic ossification) that occurs in muscles following trauma.
Os acromiale is an accessory ossification center of the acromion. Although the os acromiale is normally fused by age 25, it can remain unfused in some individuals. It is an important entity to be aware of because it may be misinterpreted as an acromial fracture. In addition, a higher prevalence of subacromial impingement and rotator cuff tears has been associated with os acromiale.
As the term suggests, AC separation is widening of the AC joint space from ligamentous injury.
Type I AC separation is stretching or partial tear of the AC ligament with no displacement seen on a radiograph. One can assess this condition radiographically by obtaining and comparing weight-bearing views of the uninjured shoulder and injured shoulder. This is a stable injury and has excellent prognosis of healing.
Type II AC separation is complete tear of the AC ligament with widening of the AC joint. Most of these injuries heal without surgery.
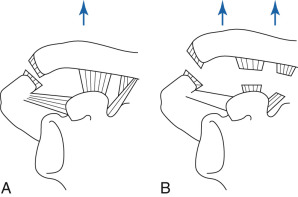
Type III AC separation is complete disruption of both the AC and coracoclavicular (CC) ligaments, resulting in abnormal widening of the AC and CC intervals. This type of injury requires internal fixation ( Figure 45-1 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here