Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cross-sectional imaging modalities such as computed tomography (CT), magnetic resonance imaging (MRI), and ultrasonography are commonly used for diagnosis of pancreatic diseases. CT has been the most commonly used technique because it can provide high-resolution images of the pancreas and depict even small lesions and calcifications. With the advent of multidetector computed tomography (MDCT) technology, acquisition speed and image quality have significantly improved. The development of 64-, 128-, 256-, and 320-slice scanners provides images with isotropic voxels on different phases of enhancement. MRI combined with magnetic resonance cholangiopancreatography (MRCP) has a growing role in imaging of the pancreas and biliary ducts. MRCP allows evaluation of the pancreatic parenchyma, biliary and pancreatic ducts, and vessels during the course of a single examination. The lack of ionizing radiation is an important advantage of MRI, making it an excellent choice for serial imaging. Transabdominal ultrasonography is often the primary diagnostic imaging modality in patients with suspected pancreatic/biliary disease. Contrast-enhanced ultrasonography may improve accuracy in detecting pancreatic diseases but is not widely used in the United States. Even with the use of contrast agents, ultrasonography has inherent limitations. Visualization of the entire pancreas is often not possible because of overlying gas or due to patient obesity, and the quality of the examination is dependent on the experience of the operator. This chapter reviews the MDCT, MRI, and ultrasound imaging features of congenital, inflammatory, and neoplastic diseases of the pancreas, and the role of interventional radiologic procedures in their management. There is also ongoing research regarding the utility of dual-energy CT (with its reduced radiation dosage to imaged patients) in the detection of focal pancreatic lesions.
Pancreas divisum is the most frequent congenital pancreatic abnormality. This entity may be asymptomatic; however, it is frequently associated with acute or chronic pancreatitis. It is very difficult to diagnose pancreas divisum on CT because the pancreatic duct is difficult to visualize in its entirety, especially when it is normal in size.
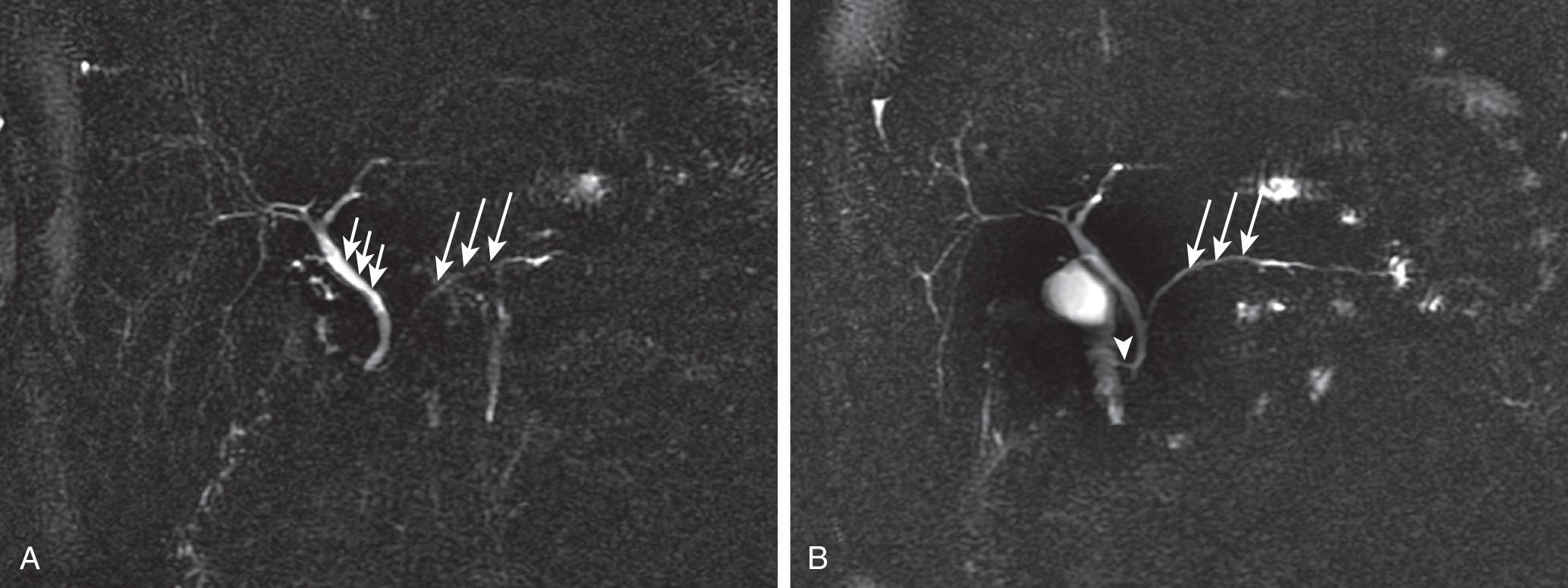
On the other hand, MRCP highlights the ducts and allows visualization of the separate entries of the dorsal and ventral pancreatic ducts into the duodenum in patients with pancreas divisum. Because pancreas divisum is a key consideration in individuals with pancreatitis of unknown etiology, MRI plays an important role in the imaging evaluation of these patients. Occasionally, the pancreatic duct is not visualized as a result of its small size or secondary to edema of the pancreas. In these cases, MRCP following secretin administration can improve delineation of the pancreatic ductal anatomy ( Fig. 95.1 ).
In anomalous pancreaticobiliary ductal junction, the main pancreatic and common bile ducts join within the duodenal wall and form a common channel (usually measuring more than 15 mm) proximal to the sphincter of Oddi. Because anomalous pancreaticobiliary ductal junction is associated with pancreatitis and biliary carcinogenesis, its recognition is critical. Although endoscopic retrograde cholangiopancreatography is the most reliable method for evaluation, endoscopic sonography and MRCP are also useful for diagnosis. MRCP noninvasively detects the anomalous union between the common bile duct and the pancreatic duct. MRCP can also reveal associated choledochal cysts, biliary dilation, pancreatitis, or biliary malignancy (e.g., common bile duct or gallbladder carcinoma).
The distribution of fatty infiltration of the pancreas is generally diffuse but may also be focal and mimic a hypoattenuating mass on CT. In these cases, MRI can provide the correct diagnosis via employment of the chemical shift technique, which unambiguously demonstrates fatty infiltration of the parenchyma.
On CT, diffuse fatty infiltration appears as separation or replacement of lobules of parenchymal tissue by intermixed, low-attenuating areas. Fatty focal infiltration is seen as hypoattenuating, nonenhancing fat interdigitating between normal pancreatic tissues. The focal sparing of fatty infiltration appears as a hyperdense, platelike, or triangular area, compared to the fat-infiltrated areas of the pancreas. On MRI, areas of focal fatty infiltration demonstrate loss of signal intensity on opposed-phase gradient-echo T1-weighted images compared to in-phase T1-weighted images; this is caused by the presence of intracellular lipids in these focal areas. Unlike pancreatic adenocarcinoma, focal fatty infiltration does not cause upstream pancreatic parenchymal atrophy, ductal dilation, or displacement of adjacent vessels.
Annular pancreas is a rare congenital abnormality that may require surgical treatment, depending on the degree of duodenal obstruction. CT and MRI demonstrate the normal pancreatic tissue encircling and encasing the second portion of the duodenum. Immediate postcontrast images can be helpful in differentiating pancreatic tissue from the duodenum because of its relatively early and avid enhancement and to better demonstrate corresponding circumferential thickening of the duodenal wall. In addition, MRCP is able to depict the course and drainage of the pancreaticobiliary duct system. Contour abnormalities are particularly common in the uncinate process and tail of the pancreas, but can also involve the body. Visualization of a normal duct crossing the area of contour abnormality is a very helpful imaging sign to exclude inflammation or neoplasm.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here