Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
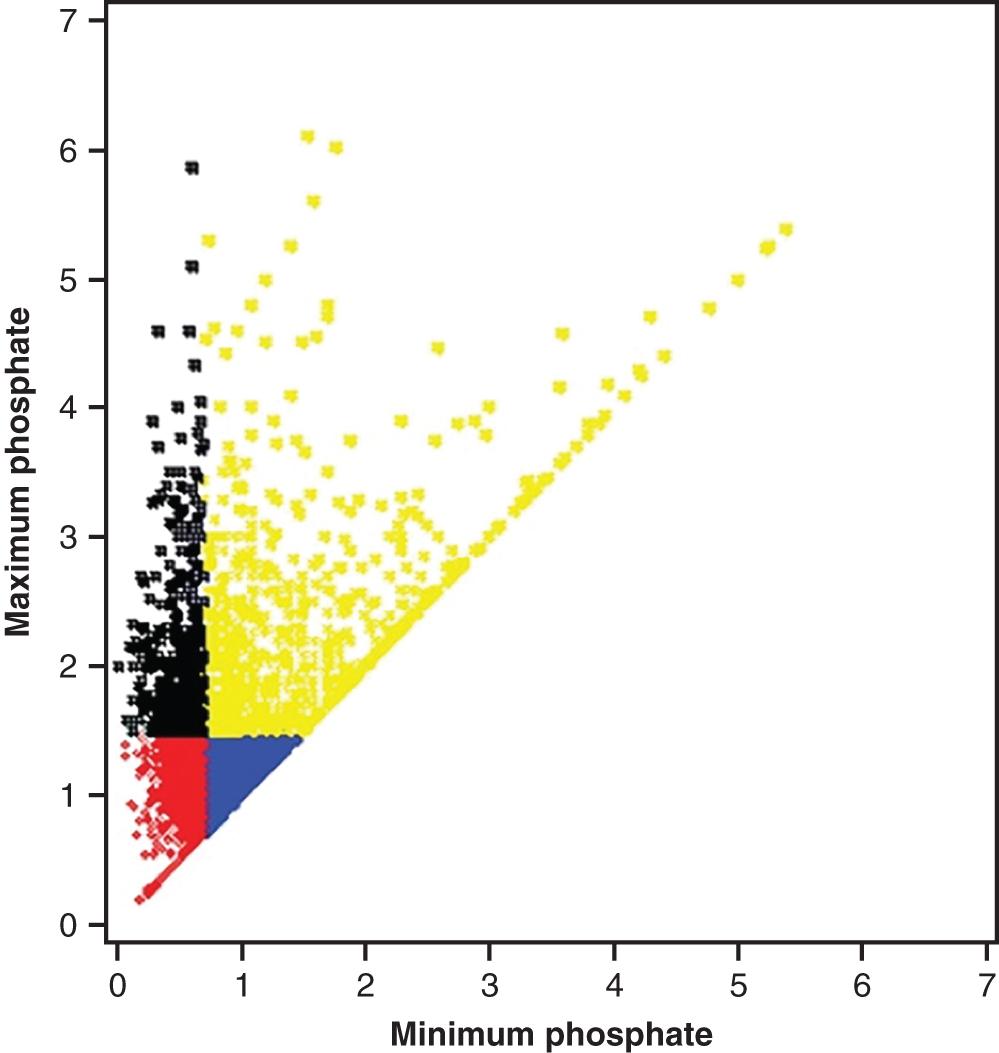
Disturbances in the phosphate balance are common in critically ill patients, but are not always easy to relate to specific symptoms. Dysphosphatemia, however, may cause a significant increase in multiorgan failure. In a Swedish critical care cohort, more than half of the patients showed at least one serum phosphate concentration value outside the normal range ( Fig. 17.1 ). Serum phosphate levels should be measured repeatedly and at least once daily in the intensive care unit (ICU). Hypophosphatemia is multifactorial and independently associated with increased mortality, whereas hyperphosphatemia most often is secondary to renal failure. This chapter presents the etiologies, classifications of severity, clinical manifestations, and treatments of hypophosphatemia and hyperphosphatemia.
Most phosphorus in the human body is complexed with oxygen as phosphate, which is a major intracellular anion. Approximately 85% of the total phosphorus amount (600 g = 20 mol) is contained in bone, where it is a constituent of crystalline hydroxyapatite. The rest (15%) is found in soft tissues, mostly intracellularly as a component of organic compounds, such as nucleic acids, cell membrane phospholipids, adenosine triphosphate, red blood cell 2,3-diphosphoglycerate, and phosphoproteins.
The normal serum phosphate concentration in adults ranges from 0.81 to 1.45 mmol/L (2.5–4.5 mg/dL). Phosphate concentration is 30% higher in children and 50% higher in infants, possibly because of an important role in growth. There is a circadian variation that is dependent on dietary intake in healthy subjects.
Serum laboratory analyses measure the free inorganic phosphate ions H 2 PO 4 − and HPO 4 2− —their ratio is pH dependent; at 7.4, the ratio is 1:4. Serum phosphate levels do not reflect total body phosphorus content. There is no common method in use to measure total body phosphorus stores. Only 55 % of the phosphate in serum is free, whereas 35% is complexed with sodium, calcium, and magnesium and 10% is bound to albumin.
The serum phosphate level may be low, although the total body phosphorus amount is normal, because of a shift into intracellular compartments or a negative intake/excretion balance. On the contrary, a total body phosphorus depletion can prevail in parallel to normal or high serum phosphate levels. Prolonged starvation and acidemia in ketoacidosis are clinical examples of situations that may deplete total body phosphorus amount.
Phosphate homeostasis relies on a complex interplay between the gastrointestinal, renal, parathyroid, and skeletal axis.
Under low serum calcium levels but also low phosphate levels, parathyroid hormone (PTH) is secreted and acts on the kidneys by enhancing hydroxylation of vitamin D to its active form, 1,25-dihydroxy vitamin D 3 , which in turn augments both phosphate and calcium intestinal absorption.
Phosphate is freely filtered in the glomeruli, and up to ∼90% is reabsorbed in the proximal tubules. PTH acts by reducing this tubular absorption.
A PTH release will result in a net drop in serum phosphate level. However, during steady state, the kidneys regulate phosphate homeostasis by matching urinary excretion with intake.
Tubular malfunction—for instance, because of rare genetic disorders—can lead to heavy phosphate urinary waste. The kidneys have a large capacity to excrete phosphate and thereby have a protective function against an ongoing phosphate load from nutritional intake and from metabolism.
Phosphatonins are regulatory peptides produced by osteoblasts and osteocytes in bone and secreted into the systemic circulation, where they decrease the renal tubular phosphate reabsorption, and thus increase the urinary phosphate excretion. Phosphatonins also participate in regulation of bone mineralisation. During baseline homeostasis about 200 mg of phosphate move in and out of the skeleton daily. Fibroblast growth factor-23 (FGF-23) is considered to be the key phosphatonin.
Hypophosphatemia can be classified as moderate 0.4–0.81 mmol/L (1.25–2.5 mg/dL) or severe <0.4 mmol/L (<1.25 mg/dL).
The symptoms of hypophosphatemia are primarily a consequence of a declining 2,3-diphosphoglycerate level in erythrocytes, which increases the affinity of hemoglobin for oxygen and thereby reducing oxygen release in peripheral tissues. This in turn leads to decreased adenosine triphosphate levels in cells, slowing down all energy-dependent intracellular functions.
Critically ill patients with diabetic ketoacidosis and sepsis have a high incidence of hypophosphatemia. In particular, patients who have had cardiac surgery and major hepatic procedures tend to develop hypophosphatemia within the first week. Certain therapies instituted in the ICU, like establishing an aggressive diuresis, renal replacement therapy, and erythropoietin therapy, increase the risk of hypophosphatemia. Modern dialysis fluids contain phosphate, counteracting too high clearance. Frequently, patients present with initial hyperphosphatemia secondary to an acute kidney injury, which rapidly may turn into hypophosphatemia after renal replacement therapy has been initiated.
The phosphate homeostasis is dependent on an ongoing intestinal supply, and states with failing intestinal absorption or even losses, such as malnutrition, vomiting, diarrhea, and nasogastric suctioning, will cause hypophosphatemia ( Box 17.1 ).
Malnutrition
Nasogastric suctioning
Diarrhea
Vomiting
Vitamin D deficiency
Diuretics
Volume expansion
Osmotic diuresis
Primary or secondary parahyperthyroidism
Renal tubular dysfunction
Fanconi syndrome
Refeeding syndrome
Ketoacidosis
Insulin effect
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here