Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Most of the current vaccines are delivered through intramuscular or subcutaneous injection. What happens between the injection, the early reaction, and the induction of protective mechanisms is explained in this chapter. Vaccine responses depend on their interaction with the immune system and understanding the main features of this interaction may help designing vaccines and defining optimal vaccination strategies. Five steps are involved: (1) initial events at the site of injection and the draining lymph nodes (dLNs); (2) recognition of antigenic specificities at B- and T-cell level; (3) cell proliferation, maturation, and differentiation; (4) effector stage with production of antibodies and effector T cells; and (5) building up of immunological memory that allows later responses at the time of exposure to the specific pathogen. We will briefly review each of these steps and consider the importance of the vaccine types and vaccine formulations in the outcome of induced responses.
More emphasis will be given to vaccine-induced antibody responses. Indeed most of the current vaccines essentially work through effects of antibodies. Antibodies can protect by a number of effector mechanisms. They can bind to the enzymatic active sites of microbial toxins and prevent their action and diffusion. They can neutralize viral replication through preventing virus entry into their target cells. They can activate the complement cascade and promote opsonization and phagocytosis of bacteria by macrophages and neutrophils. These effects are essential to rapidly limit the microbial load and to help clearing extracellular pathogens from the body. However, critical factors influence vaccine-induced antibody responses.
When one injects a classical subunit vaccine (eg, influenza or tetanus toxoid) intramuscularly, the first reaction is local pain, followed by varying levels of swelling and redness. This reaction reflects an inflammation at the injection site, characterized by increased vascular permeability and local recruitment of inflammatory cells from circulating blood.
The Lymph that may contain antigens and antigen-transporting cells arrives from the injection site through lymphatic channels. These channels open on the outer part of the dLN, in the subcapsular (or marginal) sinus. Antigens and antigen-containing cells are distributed through small conduits within the lymph node to the outer cortex and to the inner medulla. The cortex is filled with lymphocytes and the outer cortex contains aggregates of cells called follicles (B-cell zones). T cells are densely located around the cortical follicles and also extend to the medulla ( Fig. 2.1 ).
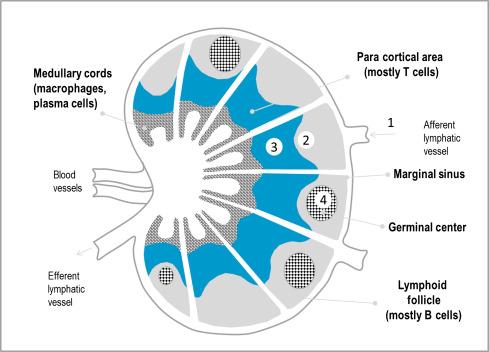
Antibody responses to protein vaccines depend on their recognition by B-cell receptors and interactions between B- and T cells within lymph nodes. The immune system can recognize 10 7 –10 9 different antigenic moieties: B- and T cells carry a highly diverse set of antigen receptors that are generated in naïve cells through gene rearrangement. Soluble antigens, such as those present in a classical influenza vaccine, which are drained from the site of injection to the marginal sinus of the local lymph nodes are translocated by specific subcapsular macrophages into the B-cell zone. If the vaccine forms a depot at the site of injection, for example, tetanus toxoid adsorbed to an aluminum salt, antigens are also captured by attracted monocytes/dendritic cells (DCs) which then migrate to the T–B cell zone border of the dLNs. There, antigen transported by activated DCs recruit and activate antigen-specific CD4 T helper cells that provide appropriate cofactors for the stimulation of antigen-specific B cells. This leads to the first step of the antibody response, called “extrafollicular” ( Fig. 2.2 ). It is associated with B-cell proliferation and differentiation into plasma cells but the resulting antibodies are of low affinity and the response is short-lived. It should be noted that replicating live vaccines which are usually injected subcutaneously, are more widely distributed than subunit vaccines. They can induce responses in multiple lymphoid sites largely dependant on the viral vaccine dynamics and tropism.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here