Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Perform a standardized history and physical examination protocol of the hip.
Perform examinations of the hip with consistent technique.
Incorporate physical examination findings with quality radiographic and three-planar osseous assessment through magnetic resonance imaging (MRI) or computed tomography (CT).
Use guided intraarticular/extraarticular injection tests to aid in diagnosis.
Learn to recognize complex posterior hip pathology.
Hip disease is commonly associated with a loss of active and passive end range of motion (ROM). A loss in ROM can result in an isolated hip pathology or induce a combination of problems with the hip and neighboring joints, especially the spine. The physical examination of the hip is designed to take the hip through a series of dynamic and passive assessments. A thorough knowledge of hip anatomy, biomechanics, clinical presentation, and diagnostics is required to correctly interpret the findings of the hip examination. An increased understanding of hip biomechanics has found that diagnostic tests can be used to determine a number of coexisting hip pathologies.
The goal of the clinical examination of the hip is to assess its five levels: the osseous, capsulolabral, musculotendinous, neurovascular, and kinematic chain. The balance and interrelationship that each system has with the other in a static and dynamic fashion is recognized, as the hip assumes an essential role in most activities. Not only is the hip responsible for distributing weight between the appendicular and axial skeletons, it is also the joint from which motion is initiated and executed. The hip joint is the center of the longest lever arm and shortest lever in the human body, from the femur to the spine segments. During running and jumping, forces upon the hip joint can reach three to five times body weight. Hip pain often stems from a sports-related injury, and some athletes are prone to hip injury and secondary degenerative hip disease.
Historically, 60% of intraarticular disorders were initially misdiagnosed. Improved techniques have reduced misdiagnosis. The physical examination of the hip must be inclusive enough to rule out other potential pain generators as a dominant cause of complaint. An organized physical examination is designed to differentiate between pain generators originating from intraarticular structures of the hip and those originating from extraarticular structures surrounding the hip in addition to the spine, abdominal, neurovascular, and neurologic systems. The hip is recognized as the source of pain when a consistent method of interpreting the history and clinical examination of the hip is followed. The goals of this chapter are (1) to review pertinent information required for a detailed patient history; (2) to describe how a structured, comprehensive clinical examination of the hip is performed; and (3) to further outline and explain the commonly misdiagnosed posterior hip.
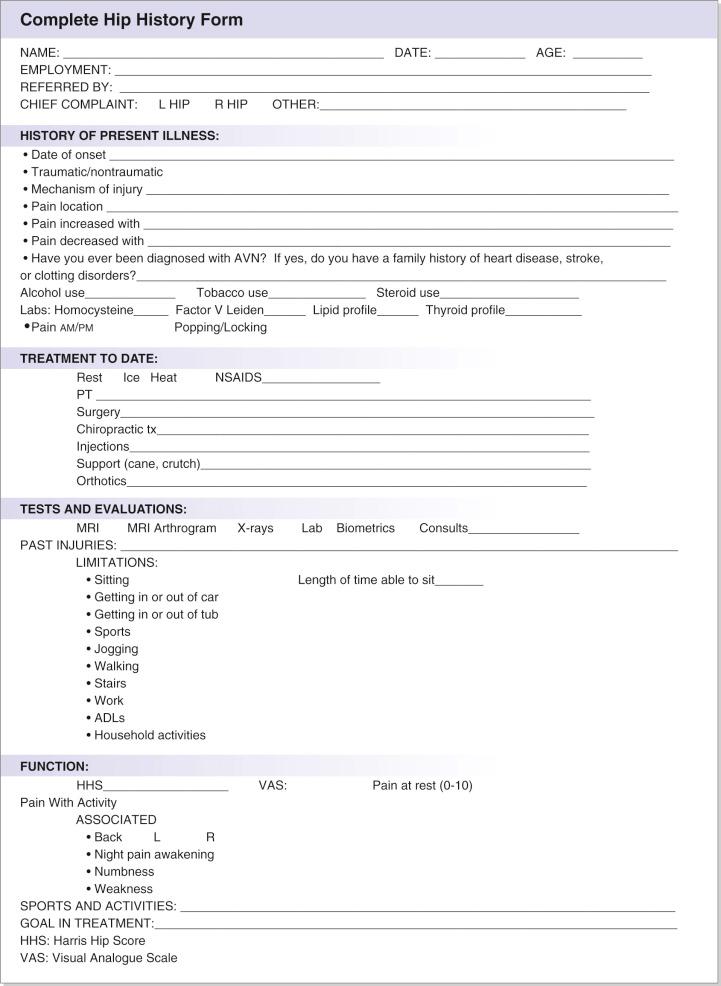
A complete patient history is obtained before physical examination of the hip is performed. The first factors in consideration of treatment are the age of the patient and the presence or absence of trauma. A description of the present condition is documented, including date of onset, mechanism of injury, pain location, and factors that increase or decrease the pain. Previous consultations, surgical interventions, and injuries are documented. Treatments to date, such as rest, physical therapy, ice, heat, nonsteroidal antiinflammatory drugs (NSAIDs), surgery, injections, orthotics, and the use of support aids, must be delineated. Limitations to patient function are detailed; these may involve getting into or out of the bathtub or car, performing activities of daily living, jogging, walking, or climbing stairs. Symptoms related to the back, the neurologic system, or the abdomen and lower extremity complaints must be recognized. Lumbar problems occasionally are confused with problems in the hip as a partial or dominant cause of complaint, particularly in the presentation of posterior hip or buttock pain. Associated complaints—such as pain in the abdomen or back, numbness or weakness in a dermatomal distribution, cough, or sneeze exacerbation—help the clinician identify lumbar issues.
The vascular supply to the femoral head and any possible sources of disruption are screened, including metabolic disorders such as abnormalities in lipids, thyroid, homocysteine, and clotting mechanisms. The social history of the patient is reviewed to identify the presence or use of tobacco, alcohol, steroids, or altitude issues, all of which can affect the blood supply to the femoral head. A history of sports and recreational activities helps document the potential mechanism of injury. Rotation sports—such as golf, tennis, ballet, and martial arts—have been commonly associated with injury to the intraarticular structures, including the labrum, iliofemoral ligament, and ligamentum teres.
The history and physical examination of the hip will direct the differentiation of intraarticular versus extraarticular sources of pain, along with location of the presenting pain and the presence or absence of popping/locking. Extraarticular sources of pain often respond well to nonoperative treatment; intraarticular sources require further workup, which may include radiographs, magnetic resonance imaging (MRI), MRI arthrogram, or diagnostic/therapeutic injection tests. Patient goals and realistic expectations of treatment are discussed. Communication, understanding, empathy, and compassion are important in obtaining an accurate history. Fig. 28.1 provides an example of a complete hip history form.
Several questionnaires that provide quantitative and qualitative descriptions of a patient's functional ability are available. The modified Harris Hip Score (mHHS), the most documented and standardized functional score to date, is a quantitative score based on pain and function. However, problems with a ceiling effect have limited its utility, particularly in younger, more active patient populations. The Multicenter Arthroscopy of the Hip Outcomes Research Network (MAHORN) Group has validated the International Hip Outcome Tool (iHOT-33). Developed through an international multicenter study, the iHOT-33 is a self-administered questionnaire. Its target population is active adult patients with hip pathology. A short form (iHOT-12) was also described for use in routine clinical practice. The Short Form 36 (SF-36) and Short Form 12 (SF-12) are questionnaires used for general health surveys and are sometimes associated with the more hip-specific evaluation tools. Outcome is dependent on the effects of treatment, which should consider the mental and spiritual aspects of the patient. Proven useful in heart and cancer treatment, this assessment is required in complex hip pathology evaluation due to the hip's critical role in all activities of daily life. An additional commonly used questionnaire includes the Hip Disability and Osteoarthritis Outcome Score (HOOS).
A consistent hip examination is performed quickly and efficiently to screen the hip; the back; and abdominal, neurovascular, and neurologic systems. A comprehensive physical examination of the hip is inclusive enough to rule out other joints as a dominant cause of complaint. Interobserver consistency and practice account for some of the most important aspects of the evaluation. Fig. 28.2 shows an example of a physical examination of the hip intake form.
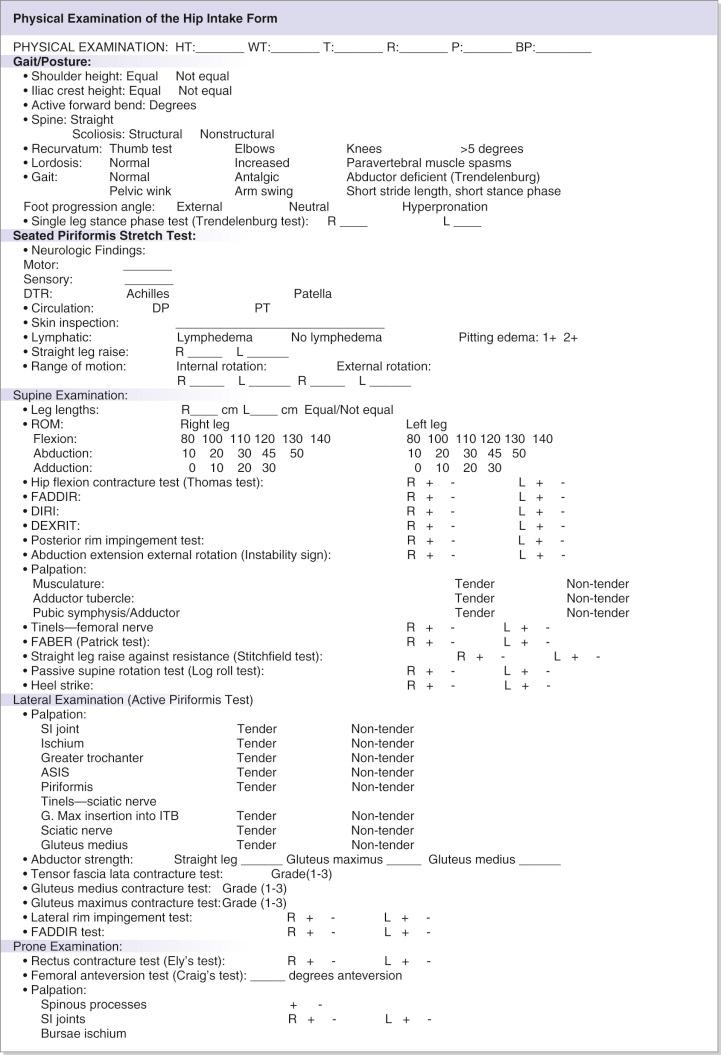
The MAHORN group physical examination consists of common tests for the core multilayer hip evaluation, involving 32 maneuvers. The osteochondral layer is assessed with 16 maneuvers, capsulolabral with 13 maneuvers, musculotendinous with 11, neurovascular with 7, and kinematic chain with 5 maneuvers. The physical examination consists of a variety of tests involving wide ranges of motion and palpation. For international clarification among clinicians, each test is given a descriptive functional title. Standardization enhances physical examination reliability. The most efficient order of examination begins with standing tests followed by seated, supine, and lateral tests, then ending with prone tests.
The general area of pain is noted by having the patient point with one finger. The groin region directs suspicion to an intraarticular problem, whereas lateral-based pain can be associated with both intraarticular and extraarticular pathology. A characteristic presenting pain pattern described by patients with hip pain is the “C sign,” in which the patient holds the hand in the shape of a C and places it above the greater trochanter, with the thumb positioned posterior to the trochanter and fingers extending into the groin. This finding can be misinterpreted as lateral soft tissue pathology, such as trochanteric bursitis or the iliotibial band; however, the patient may often describe deep interior hip pain. Posterior-superior pain necessitates a complete evaluation for differentiating hip and back pain. Often, back issues are noted concomitantly, along with musculotendinous extraarticular hip pathology.
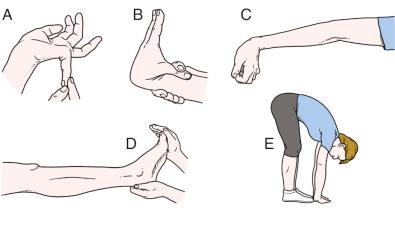
As the patient stands ( Table 28.1 ), general body habitus is assessed and bilateral shoulder and iliac crest heights are evaluated for leg length discrepancies or pelvic obliquity. Placing incremental wooden blocks under the short-side heel will aid in orthotic considerations and leg length discrepancies. Generalized ligamentous laxity is investigated by calculating the Beighton score after assessing the patient's ability to perform a series of hypermobility tests ( Fig. 28.3 ). One point is awarded for each positive test, and a score of greater than 4/9 is indicative of generalized joint hypermobility. Forward bending allows assessment of spinal alignment and differentiation of structural versus nonstructural scoliosis. The degree of flexion at the waist is recorded. Reproduction of pain with lumbar extension and lateral bending may be indicative of a spinal etiology.
| Examination | Assessment/Association |
|---|---|
| Abductor-deficient gait | Abductor strength, proprioception mechanism |
| Antalgic gait | Trauma, fracture, synovial inflammation |
| Pelvic rotational wink | Intraarticular pathology, hip flexion contracture, increased femoral anteversion, anterior capsular laxity |
| Foot progression angle with excessive external rotation | Femoral retroversion, increased acetabular anteversion, torsional abnormalities, effusion, ligamentous injury |
| Foot progression angle with excessive internal rotation | Increased femoral anteversion or acetabular retroversion, torsional abnormalities |
| Short-leg limp | Iliotibial band pathology, true/false leg length discrepancy |
| Single-leg stance phase test | Abductor strength, proprioception mechanism |
| Spinal alignment | Shoulder/iliac crest height, lordosis, scoliosis, leg length |
| Laxity in other joints (Beighton sign test) | Ligamentous laxity in other joints: thumb, elbows, shoulders, or knee |
An understanding of mechanical load transfer in the hip in both static and dynamic situations is essential for assessment and diagnosis of hip pathology. Comprehensive knowledge of normal gait will aid the physician in discriminating between normal and abnormal gait patterns. Abnormal gait patterns can indicate where abnormal transfer of load is applied across the hip joint; this can result in improper force load transfer to the lower back and knee joints. Irregularities in gait are derived most often by compensating for pain perceived in stride. The musculature of the lower limbs produces the forces required for ambulation, and the ligamentous capsule maintains hip stability. This relationship emphasizes the importance of adequate postoperative rehabilitation, especially with connective tissue disorders and improper osseous alignment.
Adequate space, such as a hallway, is needed so that a full gait of six to eight stride lengths can be assessed. Gait abnormalities often help detect hip pathology and kinematic chain disorders. Gait evaluation includes observation of foot progression angle (FPA), pelvic rotation in the coronal and sagittal planes, stance phase, and stride length. FPA will indicate osseous or static rotatory malalignment, which occurs with increased femoral anteversion (in-toeing gait) or decreased femoral anteversion (out-toeing gait) versus a capsular or musculotendinous problem. Differentiation must be made for compensated or noncompensated torsion. The knee and thigh are observed simultaneously to assess rotary parameters. Secondary abnormal hip rotation may be caused by holding the knee in internal or external rotation in an effort to maintain proper patellofemoral joint alignment. This abnormal motion or battle between the hip and the knee for a comfortable position will affect the gait; this is usually seen in cases of severe increased femoral anteversion. The following are abnormal gait patterns associated with hip pathologies: winking gait with excessive pelvic rotations in the axial plane, abductor-deficient gait, antalgic gait with shortened stance phase on the painful side, and short-leg gait with dropping of the shoulder in the direction of short legs.
Long-stride gait steps are a validated measure for ischiofemoral impingement and hamstring avulsions. Patients are asked to take long walking strides to achieve terminal hip extension. Pain experienced in the posterior region during the hip extension phase of the gait can identify ischiofemoral impingement, whereas pain during the hip flexion gait phase can signify hamstring avulsion.
Careful observation of iliac crest rotation and terminal hip extension will assess pelvic rotation. On average, normal gait requires 8 degrees of hip rotation and 7 degrees of pelvic rotation, equaling a total rotation of 15 degrees. Excessive rotation in the axial plane toward the affected hip is demonstrative of producing extension and rotation through the lumbar spine to attain terminal hip extension. Excessive rotation can be associated with laxity or hip flexion contracture, which can be exacerbated by increased lumbar lordosis or a forward-stooping posture. Ischiofemoral impingement can also produce a lumbar pelvic flexion to gain hip extension. Spinal function and mechanics can be affected by gait abnormalities. In cases of excessive femoral anteversion, the patient will try to create greater anterior coverage with a rotated pelvis to achieve terminal hip extension. Anterior capsular injury or laxity can also contribute to the excessive hip rotation in terminal hip extension. Patients with a femoral anteversion greater than 30 degrees or less than −5 degrees with normal body habitus may tolerate the excessive version. Those outside or on margins of this anteversion range have less tolerance owing to body habitus. A small frame cannot tolerate the malalignment. Hip disease from any block of terminal hip extension (decreased femoral version, coxa profunda, ischiofemoral impingement, iliofemoral ligament/psoas contracture) will cause abnormal rotatory gait biomechanics.
Heel strike occurs at 30 degrees of hip flexion, thus generating maximum ground reactive forces to the hip. Neuromuscular abnormalities, trauma, and leg length discrepancies can be indicated by a shortened stance phase. Abductor weakness or disrupted proprioception can be attributed to abductor-deficient gait (Trendelenburg gait or abductor lurch). The abductor-deficient gait is an unbalanced stance phase, which may present in two ways: a pelvic shift away from the body (“dropping out” of the hip on the affected side) or a weight shift over the adducted leg (shift of the upper body “over the top” of the affected hip). Antalgic gait, a self-protecting limp caused by pain, is characterized by a shortened-stance phase on the painful side, limiting the duration of weight bearing. Differentiation of a short-leg gait involves a drop of the shoulder in the direction of the short leg.
The single-leg stance phase test is an assessment of hip joint function that simulates the single-leg stance phase with load on the examined hip. The single-leg stance phase test is performed bilaterally, with the nonaffected side examined first and serving as a baseline reference for the affected side ( Fig. 28.4 ). The single-leg stance phase position is held for 6 seconds. As the patient lifts and holds one foot off the ground, the contralateral hip abductor musculature and the neural loop of proprioception are being evaluated. If the musculature is weak, or if the neural loop of proprioception is disrupted, the pelvis will tilt toward or away from the unsupported side. A positive test is noted if the pelvis drops toward the nonbearing side or shifts more than 2 cm toward the bearing side, which may indicate weak abductor musculature, disrupted neural loop of proprioception on the bearing side, or trunk inclination. This test is also performed in a dynamic fashion.

A thorough vascular, lymphatic, and neurologic examination is performed during the seated hip examination ( Table 28.2 ). Vascular and lymphatic assessment includes the posterior tibial pulse, any swelling of the extremity, and inspection of the skin. Neurologic evaluation consists of motor function, sensibility, and deep tendon reflexes (patellar and Achilles). A straight-leg raise test detects the presence of radicular neurologic symptoms and is performed by passively extending the knee into full extension. Loss of internal rotation is one of the first signs of the possibility of an intraarticular disorder ; therefore, one of the most important assessments is that of internal and external rotation in the seated position. The seated position ensures that the ischium is square to the table, thus providing sufficient stability at 90 degrees of hip flexion and a reproducible platform for accurate rotational measurement, providing that the patient is not allowed to recline or slouch during hip rotation assessment. The hip at 90 degrees flexion places the ligaments in a relaxed, loose-packed position, allowing for an osseous assessment. Hip rotation measured in different positions (seated, prone, and supine) can be compared for an assessment of ligamentous versus osseous abnormality. Gently perform passive internal and external rotation until a firm endpoint or pain is involved and compare bilaterally ( Fig. 28.5 ).
| Examination | Assessment/Association |
|---|---|
| Neurologic | Sensory nerves originating from the L2-S1 levels, DTR of patella (L2-L4 spinal nerves and femoral nerve) and Achilles (L5-S1 sacral nerves) |
| Straight-leg raise | Radicular neurologic symptoms |
| Vascular | Pulses of the dorsalis pedis and posterior tibial artery |
| Lymphatic | Skin inspection for swelling, scarring, or side-to-side asymmetry |
| Internal rotation | Normal between 20 and 35 degrees |
| External rotation | Normal between 30 and 45 degrees |

Musculotendinous, ligamentous, and osseous control of internal and external rotation is complex. Therefore, any differences in seated versus extended positions may raise the question of ligamentous versus osseous abnormality. The seated loose-packed position will test only the osseous and ligamentum teres contribution versus the hip-extended close-packed position testing ligamentous contribution. For proper hip function, sufficient internal rotation is needed. At the midstance phase of normal gait should be at least 10 degrees of internal rotation, but less than 20 degrees is abnormal. Diagnoses such as arthritis, effusion, internal derangement including labral tear, slipped capital femoral epiphysis, femoroacetabular impingement (FAI), and muscular contracture can be related to loss of internal hip rotation. Significant side-to-side differences can be related to femoroacetabular impingement or to rotational constraint from increased or decreased femoral or acetabular anteversion. Increased internal rotation combined with decreased external rotation may indicate increased femoral and/or acetabular anteversion, although hip capsular function will require further radiographic and biometric assessment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here