Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Langerhans cell histiocytosis and related neoplastic histiocytoses (Erdheim–Chester disease, juvenile xanthogranuloma, and Rosai–Dorfman disease) typically arise from clonal proliferation of myeloid precursor cells driven by pathologically activated MAPK signaling, where hemophagocytic lymphohistiocytosis is a heterogeneous syndrome characterized by excessive immune activation. A revised classification proposal organizes histiocytoses according to pathogenic mechanisms and distribution as well as histology ( Table 15.1 ) and ( Table 15.2 ).
Dendritic cell and dermal dendritic cell disorders
|
Macrophage-related disorders
|
Malignant histiocytic disorders
|
| Histiocytosis group | Diseases |
|---|---|
| L |
|
| C | Cutaneous/mucosal non-LCH
|
| R |
|
| M |
|
| H |
|
The prevalence has been estimated to be between 2 and 10 cases per million children under age 15 years annually with a male-to-female ratio between 1.3 and 1.9:1. The peak incidence is between the ages of 1 and 4 years, although it may also arise de novo in older children and adults. Isolated pulmonary Langerhans cell histiocytosis (LCH) occurs primarily in adults who smoke cigarettes (>90% of cases). LCH may arise in identical twins, likely due to shared fetal hematopoietic precursors. LCH is also more common in Hispanics and less common in children with African ancestry ( Tables 15.1 and 15.2 ).
The characteristic histopathology required for a presumptive diagnosis usually shows a granulomatous-like lesion with immature dendritic-appearing cells that have characteristic bean-shaped, folded nuclei and pale cytoplasm among a robust inflammatory infiltrate. Multinucleated giant cells may be present. Definitive diagnosis of LCH requires the immunohistochemical identification of CD207 (langerin), and historically electron microscopy was used to identify Birbeck granules. Langerin and Birbeck granules are features initially thought to be exclusive to epidermal Langerhans cells that have more recently been identified in cells from other myeloid lineages. The percentage of clonal CD1a + CD207 + cells in LCH lesions varies considerably, as does the nature and extent of immune cell infiltration. CD207 + expression may be dim or absent in some lesions, particularly bone marrow, liver, and brain. Antibody testing (VE-1), molecular testing for BRAF V600E, or sensitive sequencing methods to identify alternative Mitogen-activated protein kinase (MAPK) pathway gene mutations also support a diagnosis of LCH. The somatic BRAF V600E mutation has been associated with the increased risk of relapse.
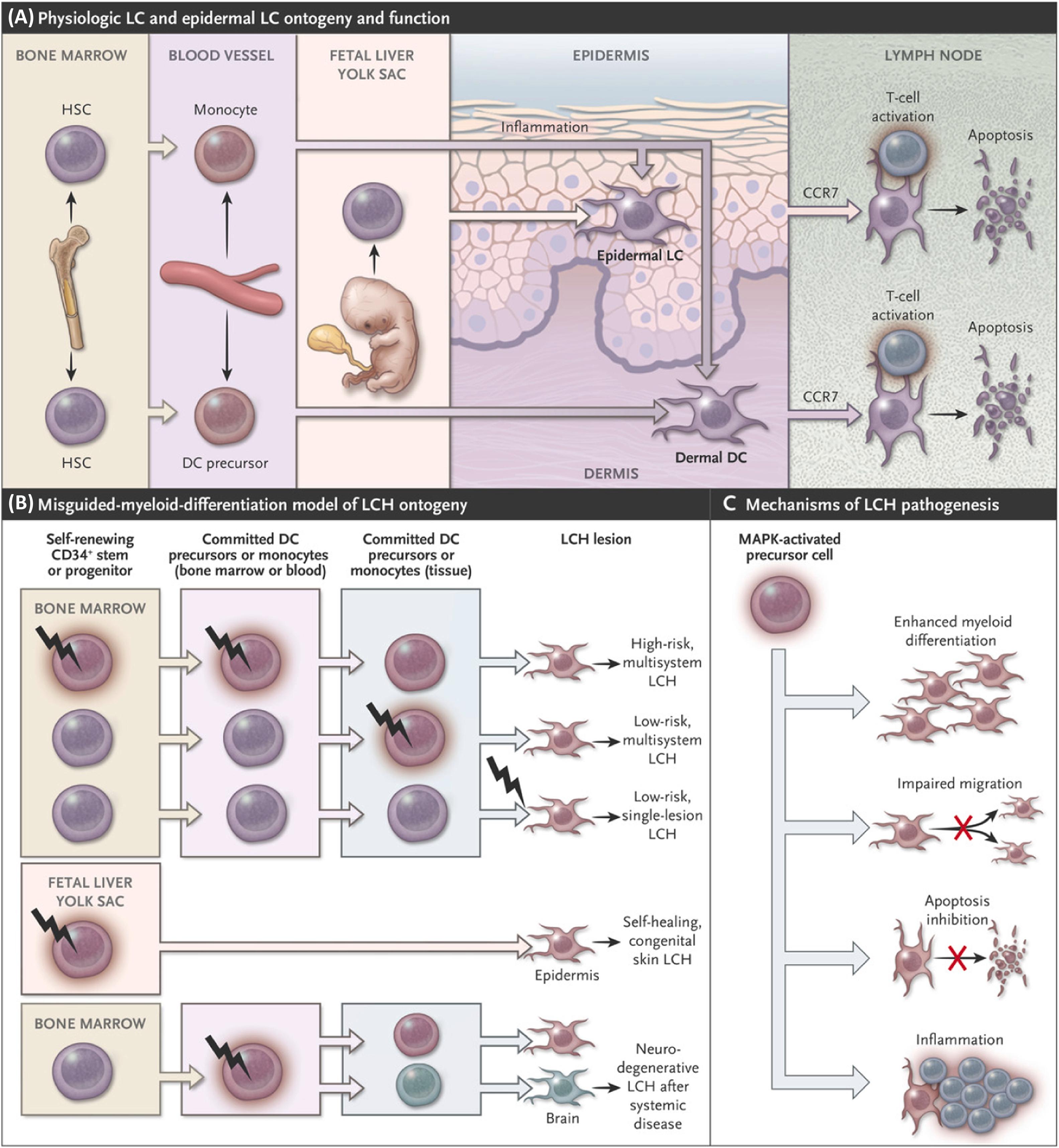
LCH is a clonal neoplasm that arises from an immature dendritic cell or in some cases an earlier hematopoietic precursor cell. The genomic landscape of LCH is quite bland other than activating MAPK pathway gene mutations identified in almost all cases. Multiple reports have now documented the presence of BRAF V600E mutations (50–60% of cases) or less frequently alternative activating mutations in BRAF , MAP2K1 , ARAF , or other MAPK pathway genes. Evidence for hematopoietic progenitors harboring BRAF V600E mutations, usually in the more severe forms of LCH, along with RNA expression patterns characterizing the transcriptome of the pathologic LCH CD207+ cell more closely with that of immature myeloid dendritic cells than with more differentiated epidermal LC. These findings have contributed to LCH being considered an oncogene-driven neoplasm of the myeloid lineage. A model for LCH pathogenesis that may be generalizable to other histiocytic neoplasms driven by activating somatic MAPK pathway gene mutations is illustrated in Fig. 15.1 .
Clinical manifestations depend on the site of lesions, number of involved areas, and the extent to which the organ function is compromised. Early reports of what is now recognized as LCH-described eosinophilic granuloma (bone lesions), Hand–Schüller–Christian disease [bone lesions, diabetes insipidus (DI), and exophthalmos], and Abt–Letterer–Siwe disease (aggressive disseminated disease). Current classification is based on sites of lesions, number of involved sites (single or multisystem; local or multifocal), and organ involvement. Patients with disease in liver, spleen, and bone marrow are categorized as high risk (HR) and patients with lesions anywhere else are considered low risk (LR) based on risk of death on Histiocyte Society trials. Approximately 50% of patients present with single-system disease, and approximately 15% of patients with multisystem disease have HR LCH. LCH-associated neurodegeneration (LCH-ND) is a poorly understood devastating sequela of LCH, characterized by progressive degeneration concentrated in brain stem, basal ganglia, and cerebellum that arises in approximately 5% of patients. Skull lesions in mastoid, orbit, clivus, or temporal bone represent central nervous system (CNS)-risk lesions due to suspected increased risk of developing DI and/or LCH-ND.
Painful bone lesions are common. Radiographically, the lesions are lytic and may have sclerotic edges or bone islands within the lytic area. They occur frequently in the skull as punched-out lytic lesions. Bone involvement of the mandible and maxilla as well as soft-tissue involvement of the gingivae may result in abnormal tooth development or loss of teeth. The involvement of vertebrae can cause vertebral collapse (vertebra plana), and lesions of long bones can result in pathologic fractures. There is often an inability to bear weight and tender, sometimes warm, swelling due to soft-tissue infiltration overlying these bone lesions. Radionuclide bone scan ( 99m Tc-polyphosphate) or Positron emission tomography (PET)/computed tomography (CT) may show localized increased uptake at the site of involvement. The differential diagnoses include osteomyelitis, malignant bone tumors, and bony cysts. Table 15.3 lists the frequency of distribution of the sites of bone lesions.
| Site | Incidence (%) |
|---|---|
| Skull | 49 |
| Innominate bone | 23 |
| Femur | 17 |
| Orbit | 11 |
| Ribs | 8 |
| Humerus | 7 |
| Mandible | 7 |
| Tibia | 7 |
| Vertebra | 7 |
| Clavicle | 5 |
| Scapula | 3 |
| Fibula | 2 |
| Sternum | 1 |
| Radius | 1 |
| Metacarpal | 1 |
Skin lesions may easily be confused with other more common pediatric rashes. In some infants, skin-limited lesions may spontaneously resolve, where in other infants the skin lesions arise as part of multisystem disease.
Cutaneous eruptions include:
diffuse papular scaling lesions, resembling seborrheic eczema (most common);
petechiae and purpura;
granulomatous ulcerative lesions; and
xanthomatous lesions.
Lung involvement may result in pulmonary dysfunction with tachypnea and/or dyspnea, cyanosis, cough, pneumothorax, or pleural effusion. Radiographic infiltrates consisting of diffuse cystic changes, nodular infiltrations, or extensive fibrosis can occur. The radiographic appearance may resemble miliary tuberculosis. In older children and adults, isolated lung LCH may be associated with heavy cigarette and/or marijuana use.
The liver may be enlarged with dysfunction that results in hypoproteinemia (total protein <5.5 g/dL and/or albumin <2.5 g/dL), edema, ascites, and/or hyperbilirubinemia (bilirubin level >1.5 mg/dL, not attributable to hemolysis). Pretreatment liver biopsy more often reveals portal triaditis and less often fibrohistiocytic infiltrates or bile duct proliferation. Sclerosing cholangitis, fibrosis, and progressive liver failure may lead to the need for liver transplantation. Activated clonal BRAF V600E + cells in liver may not express langerin (CD207).
The pathophysiology of hematopoietic dysfunction can be due to hypersplenism as well as direct involvement of the bone marrow by pathologic Langerhans cells. Activated clonal BRAF V600E+ cells in bone marrow may not express langerin (CD207). Hematopoietic system dysfunction may consist of the following: anemia (hemoglobin level <10 g/dL, not due to iron deficiency or superimposed infection), leukopenia (neutrophils <1500/mm 3 ), or thrombocytopenia (<100,000/mm 3 ).
Some patients with bone marrow involvement also develop secondary hemophagocytic lymphohistiocytosis (HLH) with potentially life-threatening pathologic inflammation and demonstrate highly elevated ferritin, soluble IL2Rα, and hemophagocytosis on bone marrow.
Occasionally, massive lymph node enlargement of cervical or other lymph nodes occurs without other evidence of histiocytosis. Physiologic trafficking antigen-presenting CD207 + cells in reactive lymph nodes may easily be confused with LCH.
LCH may present as pituitary mass with associated pituitary dysfunction. Posterior pituitary involvement with central DI is the most frequently identified endocrinopathy. Short stature has been identified in up to 40% of children with systemic LCH. Chronic illness and steroid therapy play an important role in its causation. However, short stature may also be a consequence of anterior pituitary involvement and growth hormone deficiency that may occur in up to about half of the patients with initial anterior pituitary dysfunction. Other endocrine manifestations include hyperprolactinemia and hypogonadism due to hypothalamic infiltration.
Approximately 10% of patients have biopsy-proven gastrointestinal involvement and/or digestive tract symptoms, although this may be an underestimate due to difficulty establishing diagnosis. Diarrhea, malabsorption, and hematochezia are common manifestations.
Four groups of patients can be clinically distinguished:
patients who present with hypothalamic pituitary system involvement;
patients who present with site-specific symptoms of space-occupying lesions;
patients who exhibit neurologic dysfunction characterized by a neurodegenerative picture of reflex abnormalities, ataxia, intellectual impairment, sometimes hydrocephalus, tremor, and dysarthria with variable progression to severe CNS deterioration (LCH-ND); and
patients who present with an overlap of the aforementioned symptoms.
Patients who develop CNS disease are more likely to have multisystem disease and skull lesions. Table 15.4 shows the clinical characteristics of patients with LCH who developed CNS disease compared to those who did not develop CNS disease. It reveals that patients who developed CNS disease are more likely to have multisystem disease with skull and temporal bone lesions, orbital involvement, and pituitary-related endocrinopathies.
| Percentage in LCH with CNS disease ( n =38) | Percentage in LCH without CNS disease ( n =275) | |
|---|---|---|
| Multisystem disease | 72 | 40 |
| Single-system bone disease | 18 | 53 |
| Single-system skin, lymph node | 0 | 7 |
| Primary CNS disease | 10 | 0 |
| Bone | 84 | 79 |
| Skull | 74 | 40 |
| Temporal bone | 34 | 8 |
| Skin | 58 | 25 |
| Diabetes insipidus | 31 | 6 |
| Orbits | 24 | 2 |
| Endocrinopathies | 18 | 3 |
| Lungs | 16 | 6 |
| Gastrointestinal tract | 10 | 5 |
| Liver | 10 | 11 |
| Spleen | 10 | 9 |
Signs and symptoms: disturbances in social behavior, appetite, temperature regulation, and sleep patterns are common.
Posterior pituitary involvement: Diabetes insipidus, polyuria, and polydipsia.
Anterior pituitary involvement: growth failure, precocious or delayed puberty, amenorrhea, and hypothyroidism.
Of these, DI is the most common manifestation. The incidence of this complication ranges from 5% to 35% depending upon the extent and location of disease. Most present within 4 years of diagnosis. DI is due to infiltration by the disease into the hypothalamus with or without the involvement of the posterior pituitary gland. Polydipsia and polyuria may develop at presentation, during active disease (even when there is improvement in other areas), or after therapy is discontinued and there is no other apparent active disease.
Water deprivation test with at least 3 hours of no intake and with serum and urine electrolytes and osmolalities before and after deprivation plus arginine vasopressin levels is a definitive approach to diagnosis. Correction with a dose of desmopressin (DDAVP) further confirms the diagnosis. An early morning fasting urinalysis for specific gravity and simultaneously collected urine and serum osmolality levels are also helpful as a screen.
Gadolinium-enhanced MRI studies with dedicated pituitary sequences show thickening of the hypothalamic pituitary stalk (>2.5 mm) and the absence of a posterior pituitary bright signal in T1-weighted images. These lesions are caused by pathologic infiltrates. New-onset DI is considered to represent active disease and rapid initiation of treatment, usually LCH-directed chemotherapy, is recommended. It is possible that untreated active pituitary LCH may be associated with higher risk of developing LCH-ND.
Replacement therapy with DDAVP is recommended for patients with DI with guidance from an endocrinologist. The rapid institution of effective systemic chemotherapy for disseminated disease may prevent the occurrence of DI and might be responsible for the low frequency of DI, although this has not been definitively proven. A small pituitary or empty sella suggests combined anterior and posterior pituitary insufficiency.
Patients who present with isolated idiopathic DI and morphologic changes in the suprasellar area should be closely observed. Stereotactic biopsy performed because of an enlarged pituitary stalk can distinguish a variety of conditions such as sarcoidosis, granulomatosis, tuberculosis, nonspecific lymphocytic hypophysitis, and LCH. A biopsy is not always possible. Cerebrospinal fluid (CSF) and blood analysis for markers of germ cell tumors can be an important differentiator. Patients without a definitive diagnosis and with DI are often followed with serial contrast MRIs. If the CNS lesion enlarges and no definitive diagnosis has been made, then a biopsy or empiric LCH-directed therapy may be indicated.
These lesions may arise from adjacent bone lesions, brain meninges, or choroid plexus. They usually give rise to signs and symptoms of increased intracranial pressure. They are also site specific and size dependent. Symptoms include headaches, vomiting, papilledema, optic atrophy, seizures, and other focal symptoms. Even diffuse meningitis-like manifestations can occur. These lesions may occur without any other evidence of LCH. Mass lesions may respond well to treatment, leaving minimal or no residual defects.
LCH-ND typically follows systemic disease and may arise years after a patient is presumed to be cured. Symptoms mainly follow the pontine–cerebellar pattern, beginning as a discrete reflex abnormality or gait disturbance, and/or nystagmus. Sometimes patients may also present with hydrocephalus. They can progress to disabling ataxia. Pontine symptoms include dysarthria, dysphagia, and other cranial nerve deficits, ultimately leading to fatal neurodegeneration. On MRI, enhancing lesions involving the pons, basal ganglion, and cerebellar peduncles are observed. MRI of the cerebral hemispheres may show white-matter lesions in the periventricular area. Radiographic evidence of neurodegenerative disease may occur asynchronously from clinical manifestations and can occur years after remission and often in the setting of no other obvious sites of LCH.
Biopsy shows a primarily inflammatory, lymphocyte response associated with gliosis, demyelination, and neuronal cell death. Recently, areas of neurodegeneration were associated with BRAF V600E + microglia-like cells that are clonal with systemic LCH lesion cells. Presumably, these cells propagate inflammation that drives neurodegeneration.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here