Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Early diagnosis of abnormalities in the lower extremities is important for normal musculoskeletal and neurologic development.
Developmental dysplasia of the hip starts early in the embryonic period and continues after birth. It includes a range of abnormalities including acetabular dysplasia with deficient development of the acetabulum, subluxation with displacement but some maintained contact between the femoral head and acetabulum, and complete dislocation with no contact between the two surfaces.
Congenital talipes equinovarus, also known as clubfoot, is a congenital dysplasia in the structures distal to the knee. The talus is shortened with greater acute angulation than normal. The navicular is also medially and plantarly deviated.
The calcaneovalgus foot is a soft-tissue positional contracture; it is usually a flexible deformity in which the foot is hyperdorsiflexed at the ankle and there is a mild subtalar eversion.
Congenital vertical talus or rocker-bottom foot is a rigid dorsal dislocation of the talonavicular joint with a fixed hindfoot equinus. A less severe manifestation is the oblique talus, where the navicular can be reduced in certain foot positions.
Congenital hyperextension of the knee describes a spectrum of disease, from hyperextension to subluxation to true dislocation of the knee.
Fibular hemimelia is a congenital deficiency of the fibula. Tibial hemimelia is a spectrum of disease with varying degrees of deficiency of the tibia and associated bones in the knee and the foot. Some patients may show tibial bowing in various planes. Some infants may show a spectrum of femoral shortening and deformity.
Developmental dysplasia of the hip (DDH) covers a spectrum of abnormal development of the hip that starts during embryology and continues after birth. It ranges from dysplasia, or deficient development of the acetabulum, through subluxation, with displacement but some maintained contact between the femoral head and acetabulum, to complete dislocation, with no contact between the two surfaces. , The incidence of DDH is about 1 per 1000.
There are a few known risk factors associated with DDH. These include being female, a family history of DDH, breech positioning, first-born children, and oligohydramnios. However, the etiology of DDH is certainly multifactorial. Ligamentous laxity, which can be hereditary, increases the risk of DDH. This has been confirmed in several animal models, in which changes to the hip capsule and ligamentum teres leads to DDH whereas removing the bony acetabulum does not. Additionally, newborns, especially females, respond to maternal relaxin hormone during delivery, and this may explain the higher rates of DDH in female children.
There is also a higher rate of DDH in infants born in a breech position. This is particularly true for those in a frank breech position. This may be because the hamstrings pull across the flexed hips and straight knees and act as a dislocating force. The increase in DDH in first-born children or pregnancies affected by oligohydramnios further supports the effect intrauterine positioning, in this case uterine crowding, has on DDH. Other postural orthopedic conditions such as torticollis and metatarsus adductus add to the evidence that positioning has an effect on hip development. Postnatal positioning can also lead to DDH. Positioning that keeps the hips in full extension, such as seen in cultures that use cradleboards, increases the rate of DDH.
If DDH is not treated, the hip will continue to develop improperly. The posterosuperior rim of the acetabulum loses its sharp curve over the femoral head and flattens out. This allows the femoral head to slide in and out. Over time, further changes occur, which can in fact block reduction. Pulvinar, a fatty tissue in the acetabulum, can develop and thicken. The ligamentum teres will elongate but also thicken. Both of these take up room within the acetabulum itself. The transverse acetabulum ligament, at the base of the acetabulum, can also thicken and impair spontaneous reduction. The inferior hip capsule changes shape to that of an hourglass. This reduces the opening through which the femoral head can fit. The iliopsoas, pulling across the capsule, is partially responsible for this. If treatment is started at an appropriate time, many of these changes are reversible and the contact between the femoral head and acetabulum allow for proper development of both.
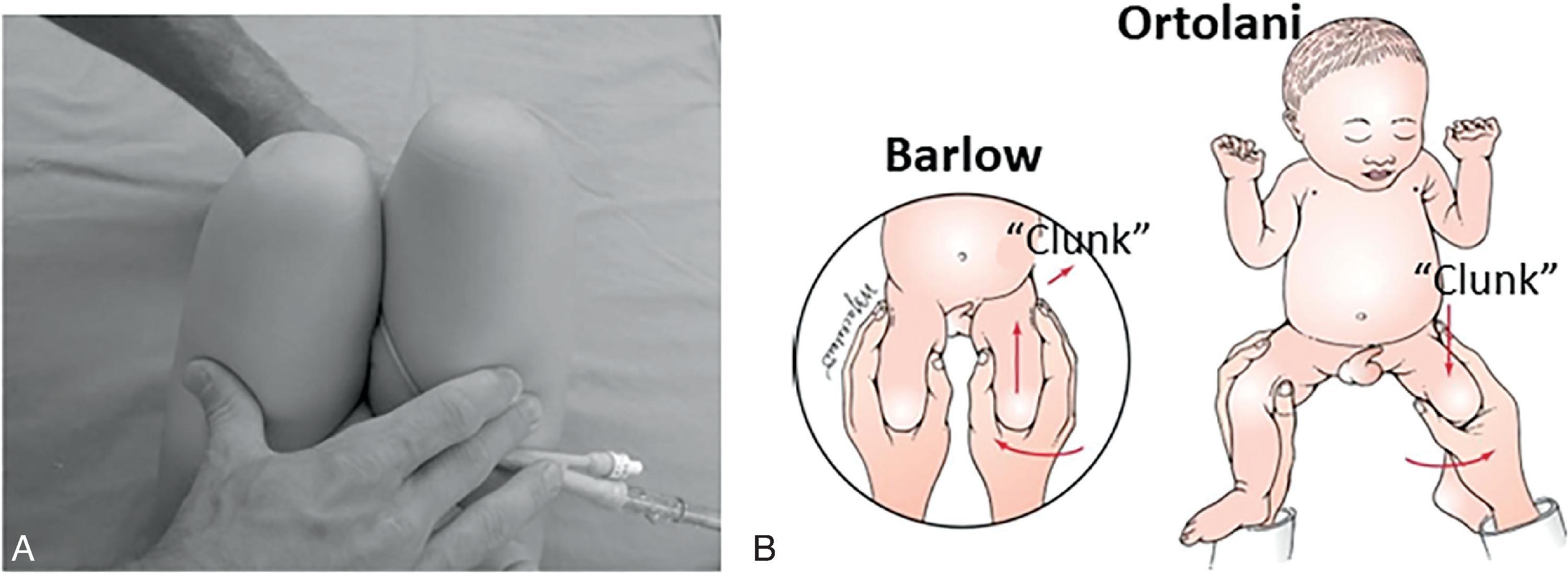
The first step in evaluation is a hip exam. A normal hip will have wide abduction symmetric with the contralateral sign. Limited range of motion (ROM) is concerning for DDH. The Barlow and Ortolani tests are best done one hip at a time and in a patient who is calm and relaxed ( Fig. 73.1 ). The examiner flexes the knees and hips and during the Barlow maneuver attempts to subluxate or dislocate the hip in a posterior direction with the hip slightly adducted. If positive, the examiner will feel the hip slide out of the acetabulum. The hip may reduce spontaneously with decreased force on the hip. During an Ortolani maneuver, the hip is abducted with pressure on the greater trochanter to try to reduce the femoral head. The examiner may feel a clunk on a positive test. These are often the earliest findings on exam.
Over time, as the hip progresses along this spectrum and becomes subluxated or dislocated without the ability to reduce it, other signs start to appear. The dislocated femoral head, located proximal to the other side, causes shortening of the thigh. This can cause asymmetric skin folds, a positive Galeazzi sign, or a positive Klisic test. In the Galeazzi sign, both hips and knees are flexed to 90 degrees with the feet flat on the exam table; the affected knee will appear shorter. For the Klisic test, the examiner places one finger on the greater trochanter and another on the anterior superior iliac sign and creates an imaginary line connecting these points. A test is negative if that line, continuing on, hits at or below the umbilicus. One that continues above the umbilicus is positive. The Klisic test is especially useful with bilateral DDH, as compared with a normal comparative side in which it is not required.
As a child with unilateral DDH begins to walk, their gait may include toe walking because one leg is shorter. They may also have a Trendelenburg gait, in which they lean over the unaffected side while walking. Again, it can be more difficult to evaluate a child with bilateral DDH, because both legs are shortened. However, there may be increased lumbar lordosis and a waddling gait.
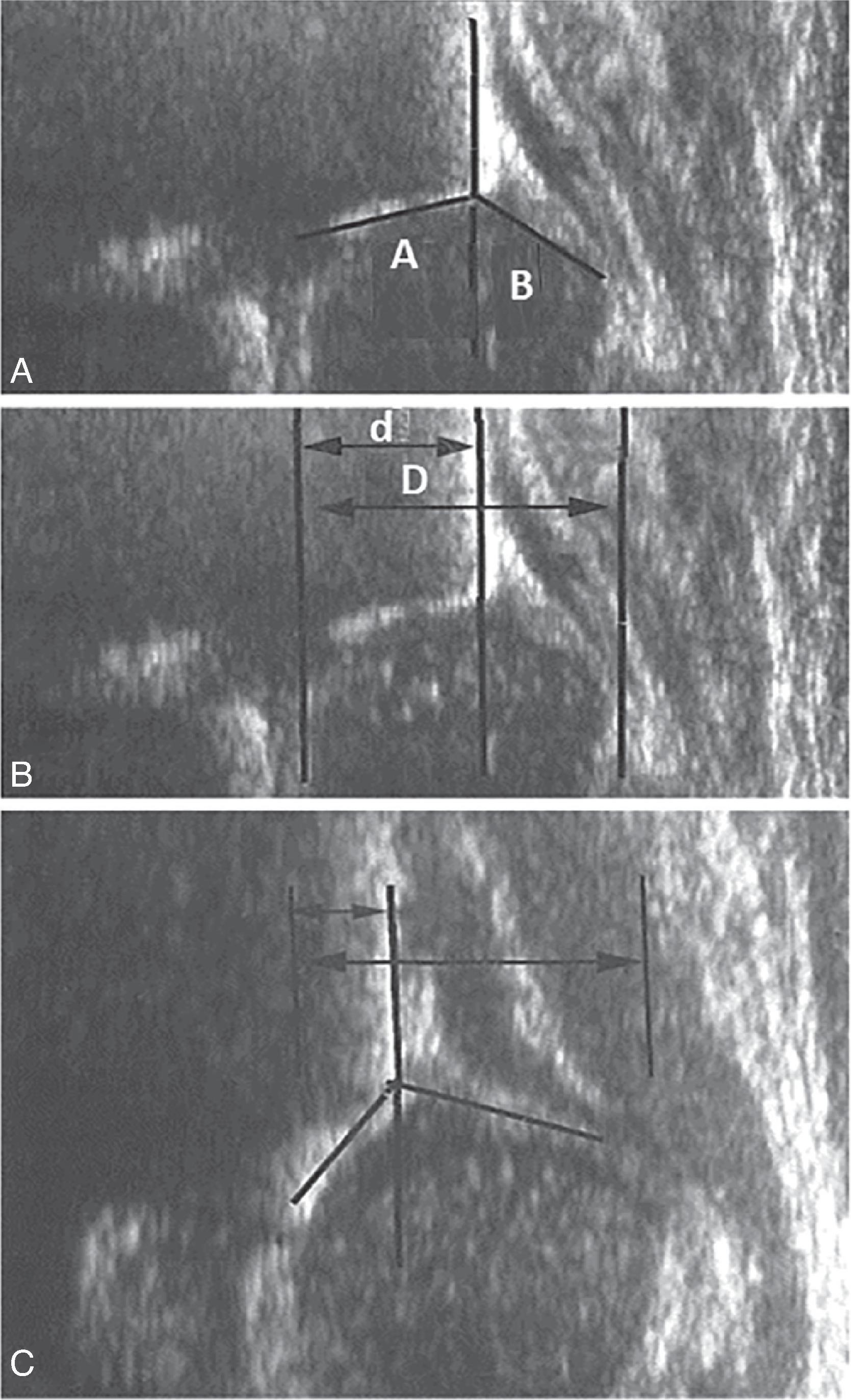
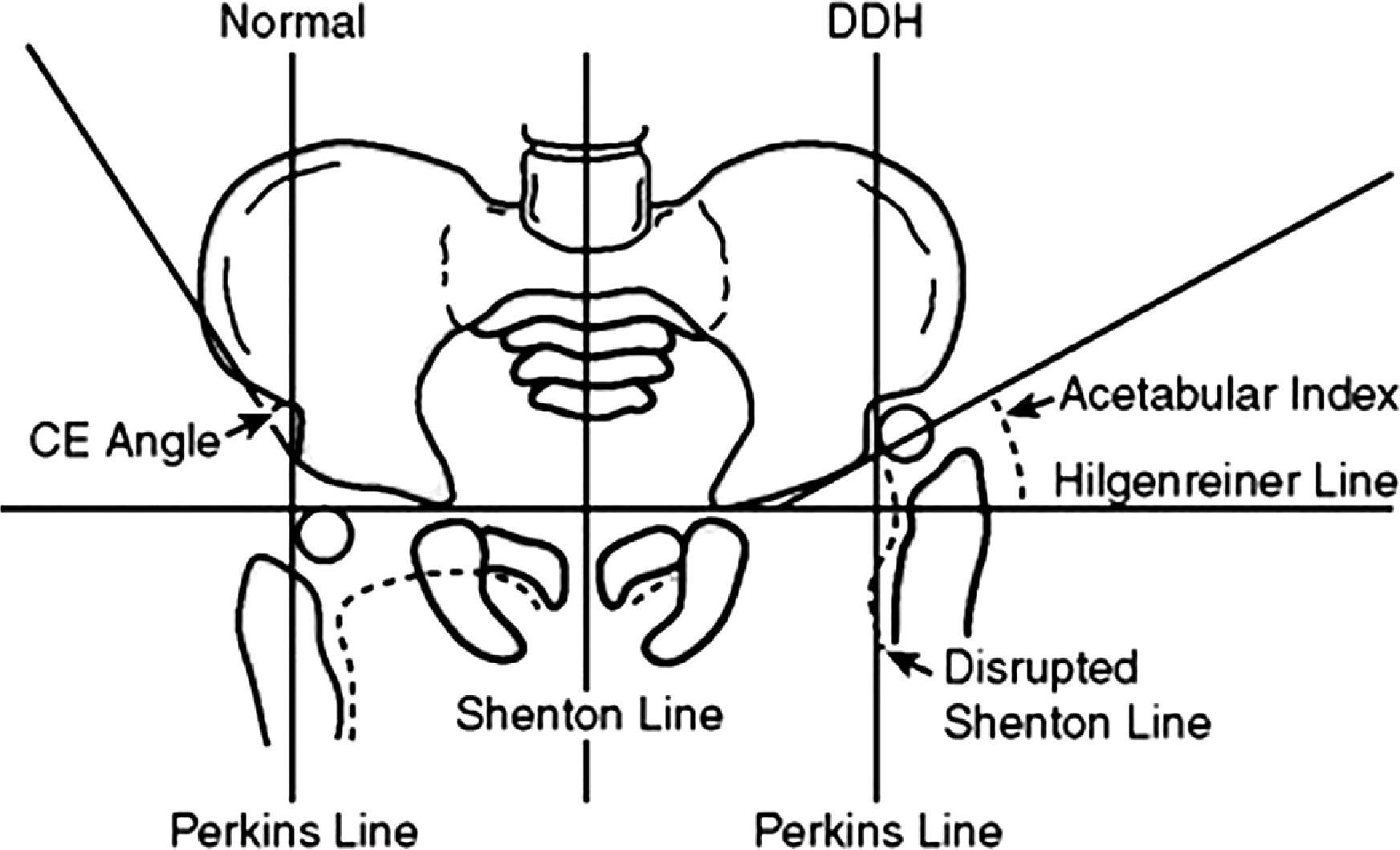
Further evaluation is done with imaging. At birth through 4 to 7 months of age, the femoral head is cartilaginous. Therefore ultrasound is used initially, although this should not be done prior to 6 weeks of age because it can increase the rate of false positives. The alpha angle, the angle between a line down the ilium and a line down the bony acetabulum, should be higher than 60 degrees, although 50 to 60 degrees can be considered borderline in infants less than 3 months. The percentage of the femoral head covered by the bony acetabulum is also measured and should be greater than 50% ( Fig. 73.2 ). A dynamic ultrasound uses the Barlow and Ortolani maneuvers to evaluate the degree of subluxation during stress. Once the femoral head starts to ossify, radiographs can be used to evaluate for DDH ( Fig. 73.3 ). Fig. 73.4 shows the appearance of a hip with DDH and useful lines and angles measured on an anteroposterior (AP) pelvis. A break in Shenton lines suggests proximal migration of the femur. The acetabular index decreases over time and should be less than 20 degrees by age 2.

In a child less than 6 months of age diagnosed with DDH, treatment with a Pavlik harness is initiated ( Fig. 73.5 ). , In the harness, the hips are flexed beyond 90 degrees, sometimes up to 120 degrees, and with the hips abducted, although not in forced abduction. The child is maintained in the harness until reduction is ensured and usually at least 6 weeks. They are monitored in clinic for any issues pertaining to the harness and with ultrasound to ensure improvement of the hips. It is vital to make sure the child continues to kick their legs, because excessive hip flexion can cause a femoral nerve palsy and loss of that motion. If that occurs, the harness should be removed until quad muscle function returns. Abduction ensures good contact between the developing acetabulum and femoral head, but forced abduction can cause avascular necrosis (AVN) of the femoral head. Pavlik harness treatment is highly successful, with success rates over 90%, albeit somewhat lower in hips that are irreducible. If the harness does not show reduction of the femoral head, other, more rigid abduction braces can be used and have reported variable degrees of success based on the reducibility of the hip.

In an infant who presents after 6 months of age or who fails treatment with a Pavlik harness, closed reduction in the operating room is indicated. This includes an arthrogram, where dye is injected into the hip, which allows for better fluoroscopic evaluation of the femoral head and the reduction. The practitioner will also evaluate how easily the hip reduces, if at all, and the range of abduction in which the hip maintains a stable reduction. If that window is too narrow, an adductor tenotomy can be performed to widen that range. If the reduction is adequate, the patient is placed in a spica cast. They are usually taken back once or twice for repeat evaluations in the operating room and cast exchanges.
If the hip is irreducible or is not adequate, an open reduction will be performed. This can be done through two approaches, an anterolateral or a medial approach, both with their pros and cons. In patients who present after 18 to 24 months, most surgeons will primarily do an open reduction. This approach can be combined with a pelvic or femoral osteotomy. A pelvic osteotomy will increase coverage of the femoral head and can reorient or decrease the size of the acetabulum depending on the type of osteotomy performed. A femoral osteotomy usually includes shortening of the femur, which decreases the force needed to reduce the hip. It can also derotate the femur if required. These procedures are also followed with a period of spica casting and possibly followed with abduction bracing afterward.
Most studies support excellent outcomes of DDH treatment even into adulthood. This is true even for hips that show radiographic abnormalities or signs of early degeneration. However, the biggest and potentially most devastating risk during any of these treatments, including the use of a Pavlik harness, is AVN, which causes a growth disturbance of the proximal femoral physis. This is most often caused by excessive abduction in either the brace or cast. Increasing abduction has been shown to decrease blood flow into the femoral head, even in a normal population. Forceful reductions can also increase tension between the femoral head and acetabulum, reducing blood flow and thus also creating AVN. Mild AVN leads to minimal changes in the femoral head and is often well tolerated without long-term sequelae in children. However, more severe forms of AVN significantly alter the shape of the hip joint, potentially leading to alterations in gait and early arthritis. , Therefore, it is vital to be vigilant about positioning of infants in harnesses and casts and to include a femoral shortening osteotomy if the reduction required significant force.
Congenital talipes equinovarus, better known as clubfoot, is a congenital dysplasia of all the structures distal to the knee. This leads to a situation of an abnormal foot in an abnormal position. The goals of treatment are to place the foot in a functional position, although the underlying differences in the musculoskeletal structures are still present. However, outcomes can still be exemplary and allow the patient to lead a normal, fully active lifestyle.
Although there have been several genes that increase the likelihood of clubfoot, there is no one specific gene that definitively causes it. Other proposed etiologies include a neuromyogenic imbalance, an arrest in embryologic development, and a fibrotic response causing contraction of the foot. Studies have both supported and refuted these hypotheses. Additionally, there does seem to be a hereditary pattern to clubfoot, albeit not following a specific hereditary pattern. This suggests that clubfoot is multifactorial but does lead to abnormal development during embryologic development.
The pathoanatomy demonstrates significant abnormality of the talus, which becomes shortened and has more of an acute angulation than normal. Additionally, the entire bone itself is medially and plantarly deviated. , Although the calcaneus and navicular are less abnormal, there are articular changes related to their relationships with the talus. The navicular in particular, which is also medially and plantarly deviated, can create false articulations with the medial malleolus and often leaves the talar head undercovered. Furthermore, there are often contractions of joint capsules, ligaments, and tendons. Because this is a dysplasia starting at the knee, the gastrocsoleus is often smaller than a contralateral, unaffected side. Lastly, reports of absent dorsalis pedis and posterior tibialis artery have been reported in idiopathic clubfeet.
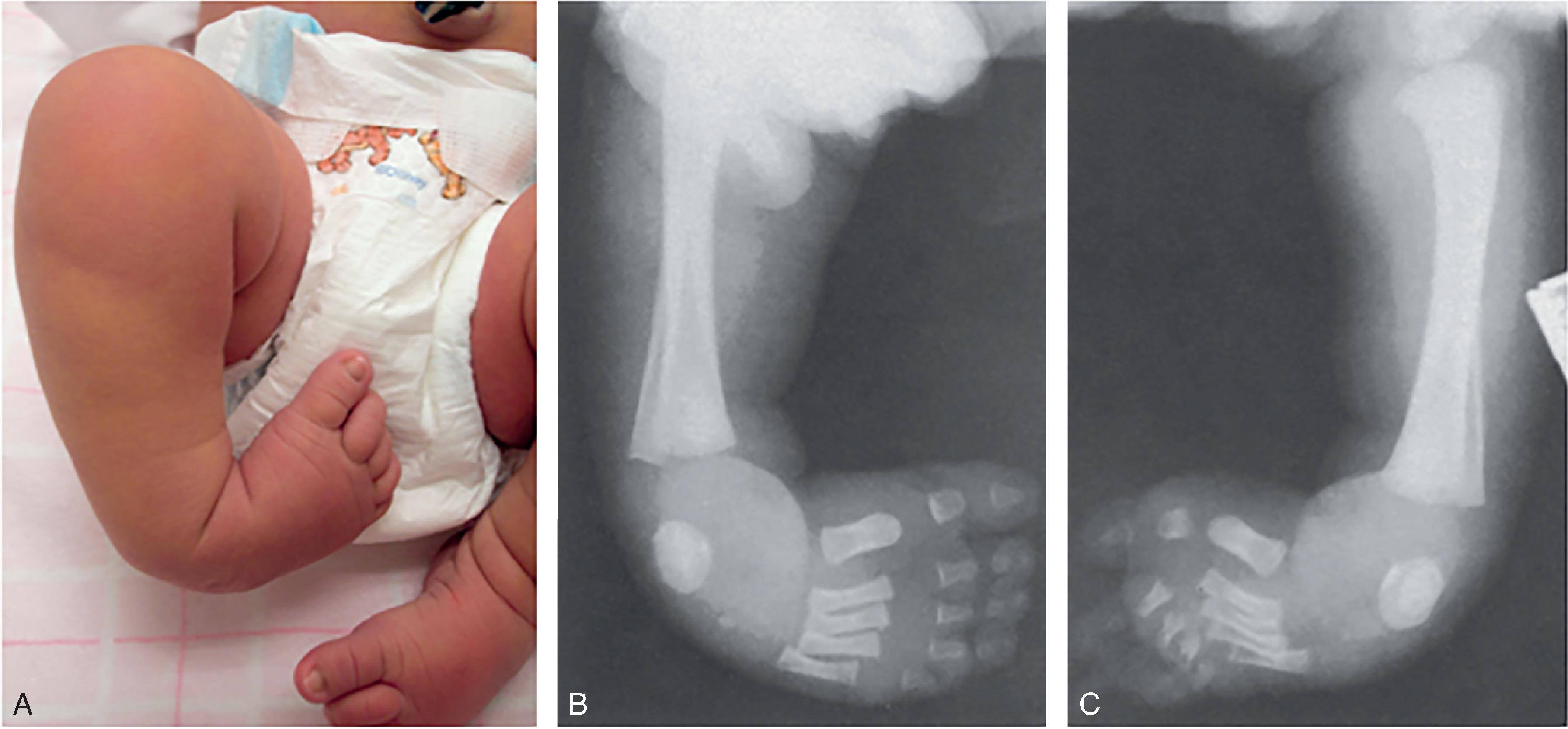
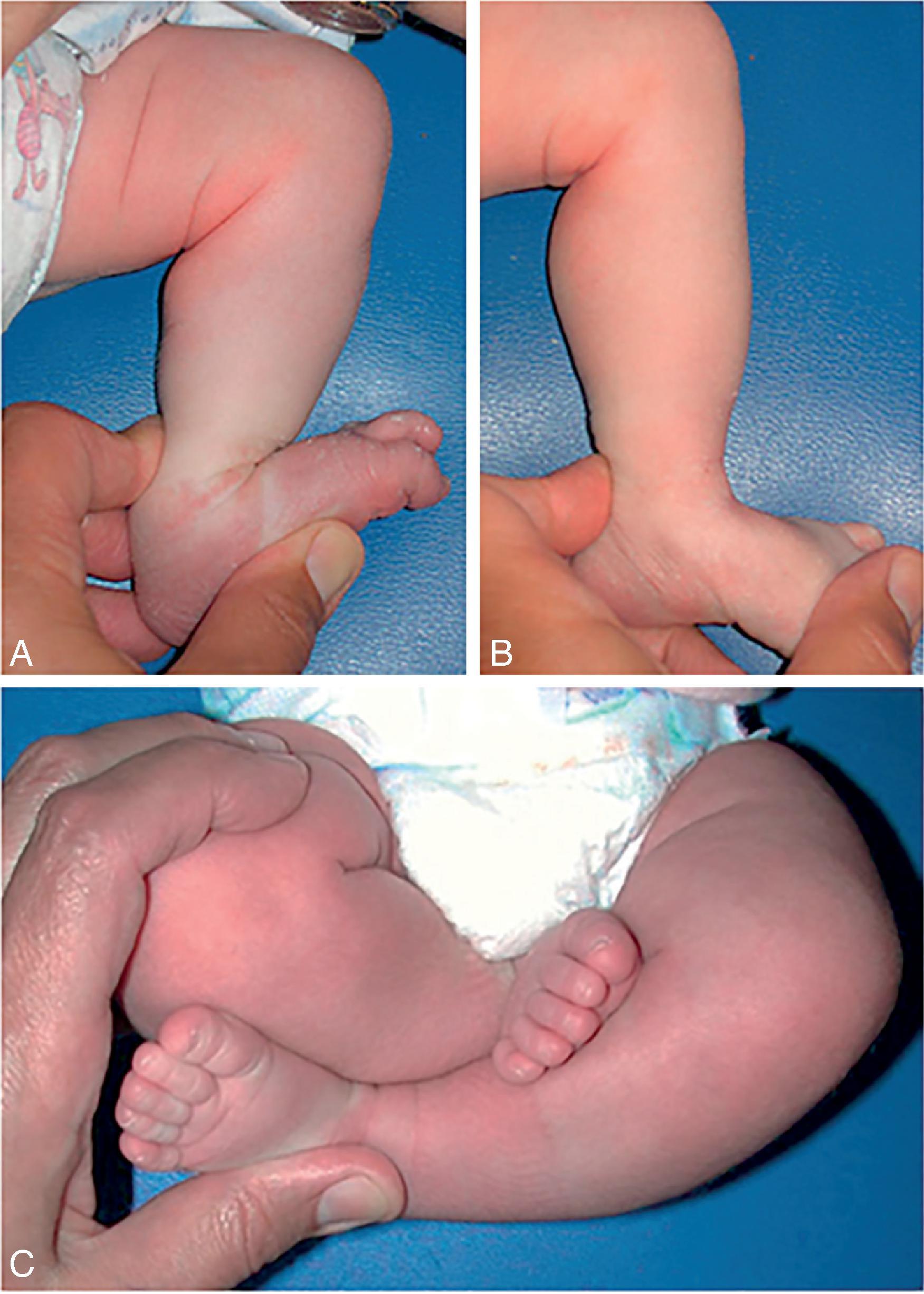
The typical clubfoot is often easily diagnosed at birth and can sometimes be seen on prenatal ultrasound scans. , The foot is equinus and inverted compared with the tibia with hindfoot varus ( Fig. 73.6 ). There is also cavus and adduction of the forefoot. Even at this young age, the unilateral clubfoot is often already smaller than the contralateral side, and this is important to point out to parents. The smaller size becomes more apparent over time, but noting this early on will avoid any concerns that treatment caused a stunting of growth. Postural clubfoot can sometimes masquerade as clubfoot, but its flexibility and ability to correct to neutral, especially without any fixed equinus, helps differentiate it.
Clubfoot can be idiopathic or associated with a variety of conditions, and therefore a thorough evaluation is required. A drop-toe sign, where the toes are held in plantarflexion even with plantar stimulation, may indicate an underlying neurologic condition. Certain conditions such as arthrogryposis, myelodysplasia, diastrophic dysplasia, and fetal alcohol syndrome are known to have resistant clubfoot. There are multiple classification systems available for use, and they can help predict response to treatment and outcomes over the next several years.
The current initial treatment of clubfoot is nonoperative and follows the Ponseti method, developed by Ignacio Ponseti in the 1940s, although it was not universally adopted until several decades later. Other treatments including physical therapy with stretching and taping have been used; however, the easier applicability of the Ponseti method has led to its being the dominant strategy for clubfoot management. The treatment includes weekly casts that gradually address the underlying deformities. The cavus is addressed first; the varus and adductus are addressed next and at the same time. To prevent recurrence, the foot is brought into abduction of 60 to 70 degrees, which can often be alarming to parents and other family members. Adequate explanation of the goals and expectations of casting can help allay concerns. The equinus is addressed last and is usually not fully corrected with casting alone. Therefore, a percutaneous tendoachilles tenotomy is required and can often be done in the clinic, although some practitioners prefer to do this in the operating room. The final cast is left in place for several weeks and then the patient is transitioned to a foot abduction brace to hold the foot in its new, corrected position. Patients initially wear this full time and then transition to nighttime wear for several years.
For patients who present with an underlying syndrome associated with resistant clubfoot, are of an older age, or have a recurrence, Ponseti casting can still be attempted. The foot can often achieve the same result or at least lessen the required surgical intervention. These procedures may include repeat Achilles tenotomy or lengthening, posterior capsular release or a more extensive posteromedial release, and osteotomies.
In children older than 2 or 3 years, the appearance of a dynamic supination, such that the foot inverts only during the swing phase of gait or while they are dorsiflexing the ankle, may appear. This increases weight bearing on the lateral border of the foot, and over time it can lead to hindfoot varus. This is not a true recurrence and not related to compliance during brace wear but is related to the underlying pathology of the clubfoot itself, with imbalance between the relatively stronger tibialis anterior compared with the weaker peroneal tendons and tibialis posterior. In these cases, a transfer of the tibialis anterior from the first metatarsal to the lateral cuneiform is indicated.
The Ponseti method has a 95% success rate of initial correction of the clubfoot. However, there is at least a partial recurrence in one of every 3 such feet over the next couple of years, most frequently due to poor compliance with brace wear or delayed presentation. Still, long-term outcomes are excellent, with one long-term study showing 85% of patients with normal or good outcomes. Strength was comparable with that of the contralateral normal side, whereas motion was decreased.
Increased surgery, especially intraarticular surgery, does seem to worsen outcomes. The capsulotomies stiffen the joints with further loss of motion. Additionally, overcorrection into significant hindfoot valgus is reported, especially with a full posteromedial release. Although poor brace compliance increases the need for these procedures, a more severe clubfoot at birth may also prognosticate increased need for surgery. Worse outcomes, therefore, are difficult to fully differentiate between these two groups and there is most likely overlap. There is no study comparing initial operative versus nonoperative treatment, and only further long-term studies will help delineate outcome patterns for patients with clubfeet.
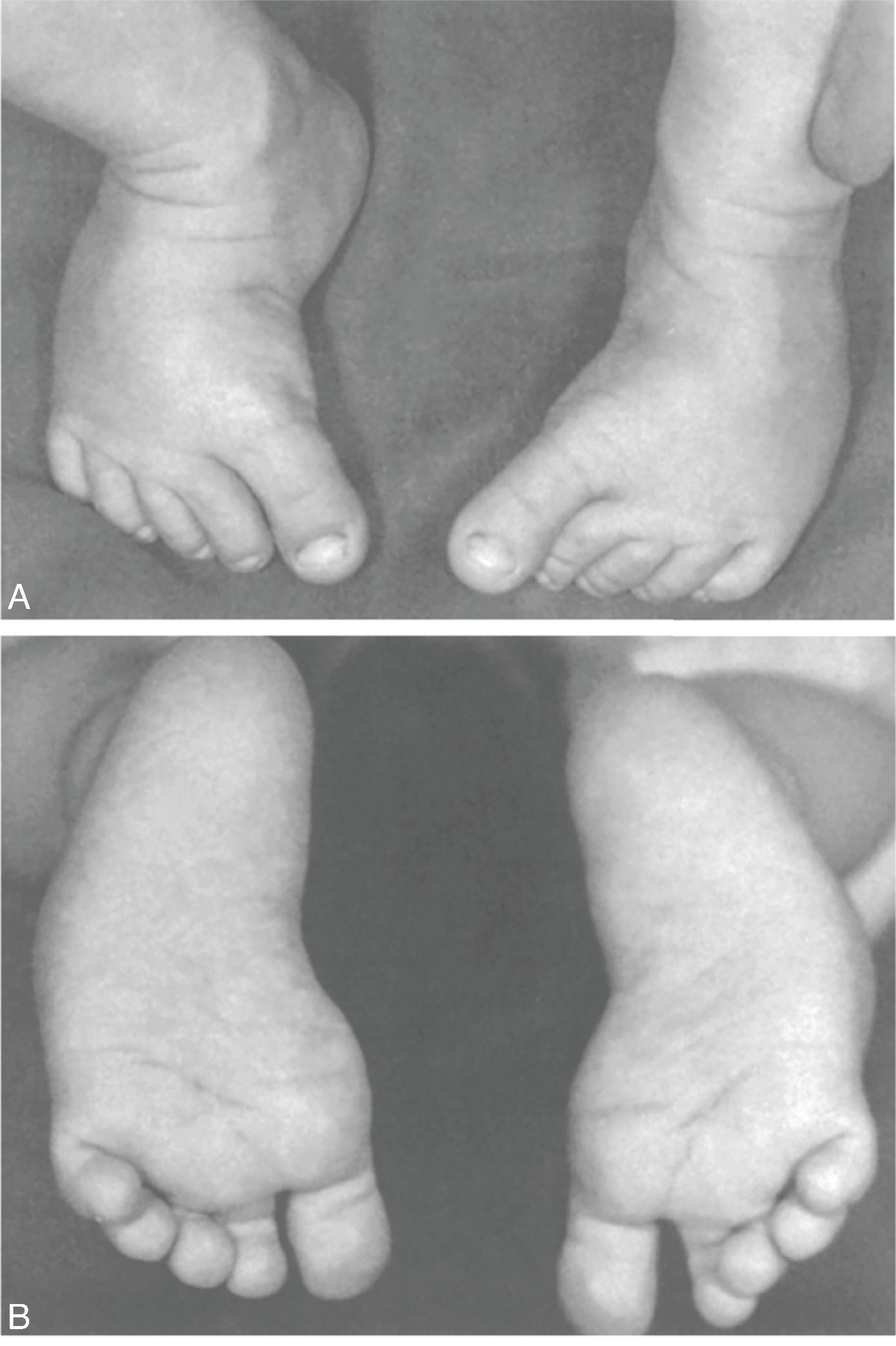
Calcaneovalgus foot is seen in newborns and is a soft-tissue contracture problem ( Fig. 73.7 ). Positional calcaneovalgus is a flexible foot deformity in which the foot is hyperdorsiflexed at the ankle and there is mild subtalar eversion; this is caused by intrauterine positioning. It is more common in girls, first-born children, and children of young mothers.
In evaluating a patient with calcaneovalgus, it will be noted that the hindfoot externally rotates and dorsiflexes. This can cause the dorsum of the foot to come into contact with the anterior tibia. Additionally, there may be associated posteromedial bowing of the tibia, which may exacerbate the appearance of the foot dorsiflexion. However, posteromedial bowing of the tibia can be isolated and is sometimes misdiagnosed as calcaneolvagus foot. To distinguish between these, the apex should be determined; in calcaneovalgus, the apex is at the ankle joint, whereas in posteromedial bowing, the apex is in the tibia. The flexibility of the deformity should also be evaluated; it most often is correctable to an almost neutral position.
Radiographs are usually not indicated unless to evaluate for other diagnoses such as posteromedial bowing of the tibia or vertical talus.
The literature is mixed about the association between DDH and calcaneovalgus, but the association does appear higher in patients who have a contralateral metatarsus adductus ( Fig. 73.8 ).
Most feet with calcaneovalgus are self-resolving, but gentle stretching of the foot into plantar flexion and inversion can be helpful. Expected improvement should occur in 3 to 6 months. Patients who also have posteromedial bowing should be counseled on the potential for a limb-length discrepancy, which may require treatment.
Congenital hyperextension of the knee is often described as the knee being “backward” and describes a spectrum of disease from hyperextension to subluxation to true dislocation of the knee( Fig. 73.9 ).

Abnormal intrauterine positioning with lack of movement from the fetus is the cause of congenital hyperextension and knee dislocation. Although congenital hyperextension is often idiopathic, syndromes associated with laxity and/or decreased fetal movement, such as Larsen, Beals, or Ehler-Danlos syndrome and arthrogryposis, are associated with congenital knee dislocation. These often have an associated hip dislocation and anterior cruciate ligament (ACL) deficiency. Idiopathic, isolated congenital knee dislocation can also occur with no associated underlying syndrome. It is thought that this abnormal positioning and decreased motion then leads to quad muscle atrophy and fibrosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here