Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Single-stranded RNA (ssRNA) virus (picornavirus)
Transmission route: fecal-oral
Incubation: 2 to 6 weeks
Self-limited
Not associated with chronic carrier state, chronic hepatitis, or hepatocellular carcinoma (HCC)
Partially circular double-stranded DNA virus (hepadnavirus)
Transmission route: perinatal, sexual, and parenteral
Incubation: 6 to 8 weeks
Chronic infection (10%): persistent serum hepatitis B surface antigen (HBsAg) more than 6 months after diagnosis
Associated with chronic hepatitis, fulminant hepatitis, cirrhosis, and HCC
Anti-HBsAg confers long-term immunity
ssRNA virus (flavivirus-like)
Transmission route: parenteral
Incubation: 6 to 12 weeks
Highest rate of chronic hepatitis (60% to 80%) and persistent infection
Associated with cirrhosis and HCC
Anti-hepatitis C virus (HCV) does not confer immunity
Serum transaminases: fluctuating
Defective RNA virus requiring HBsAg (envelope protein) for infectivity
Transmission route: parenteral
Associated with more severe course of HBV infection, cirrhosis, and HCC
ssRNA virus
Water-borne infection
Incubation: 6 weeks
Virion shed in stools
Usually self-limited
High mortality rate among pregnant women
Nonpathogenic
Noncontributory
Injury is predominantly hepatocellular in the acini (zone 3)
General features
Predominantly lymphocytic infiltrate, usually conspicuous in zone 3
Swollen hepatocytes with rarefied and granular cytoplasm
Apoptotic hepatocytes showing pyknotic nuclear remnants, shrunken and dense cytoplasm
Liver cell dropout with replacement by small groups of lymphocytes and macrophages
Specific features
Hepatitis A virus (HAV): perivenular cholestasis; hepatitis with periportal inflammation (interface hepatitis) and dense portal infiltrate, including abundant plasma cells
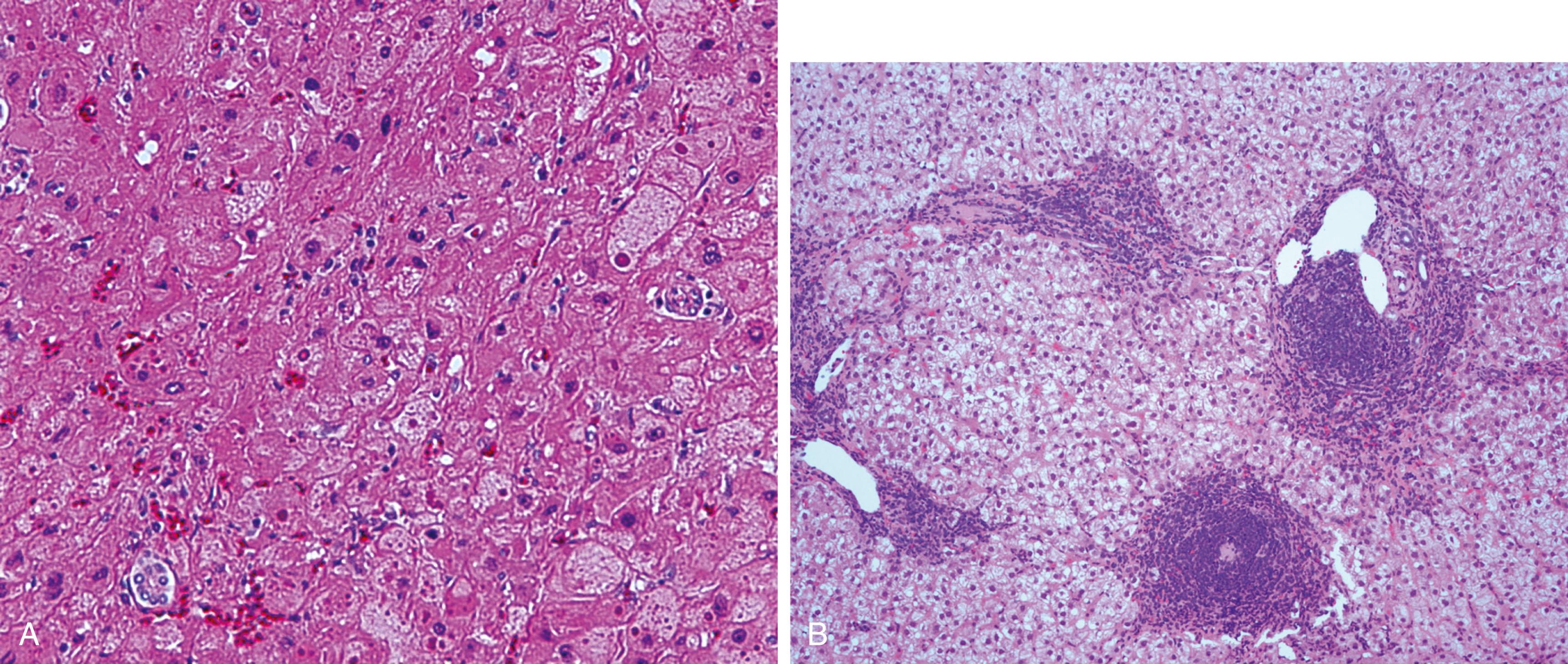
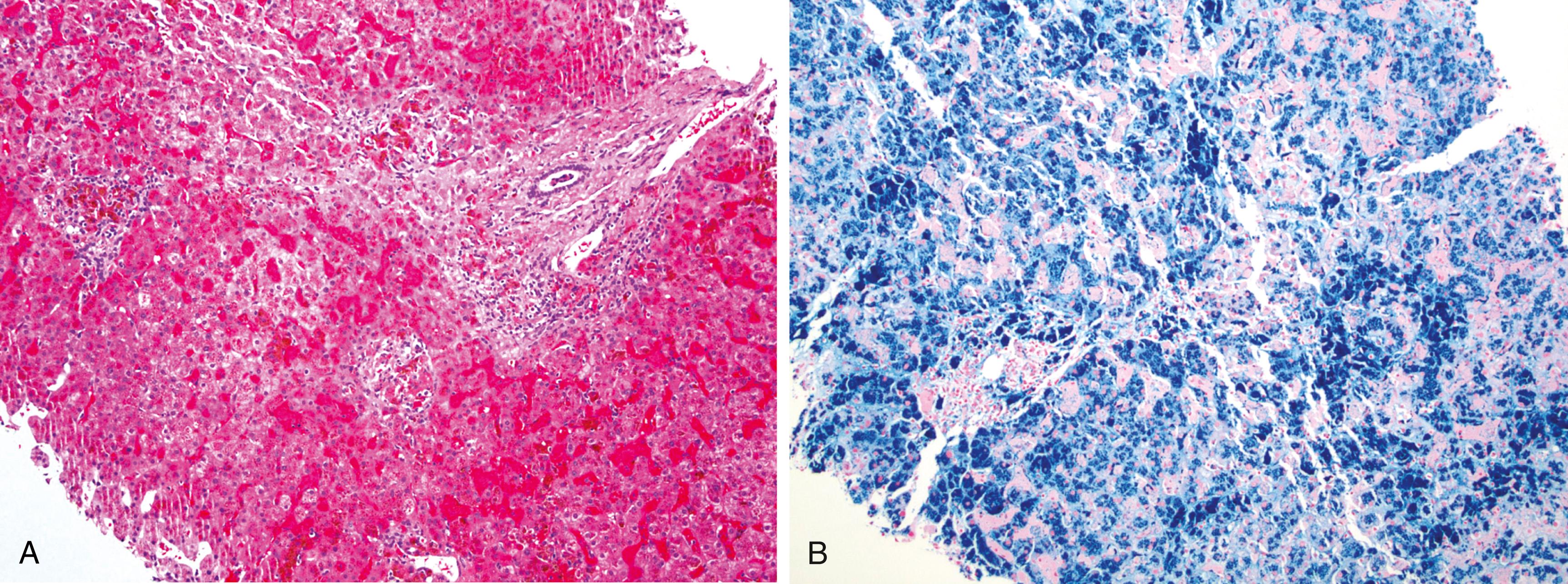
HBV: ground-glass hepatocytes (indicating abundant HBsAg in the hepatocytes—evidence of viral infection) ( Figure 7.1A )
Persistent liver injury with positive viral serology and/or nucleic acid test, and abnormally high serum aminotransferase of greater than 6 months’ duration
Injury is accentuated in the portal and periportal regions
General features
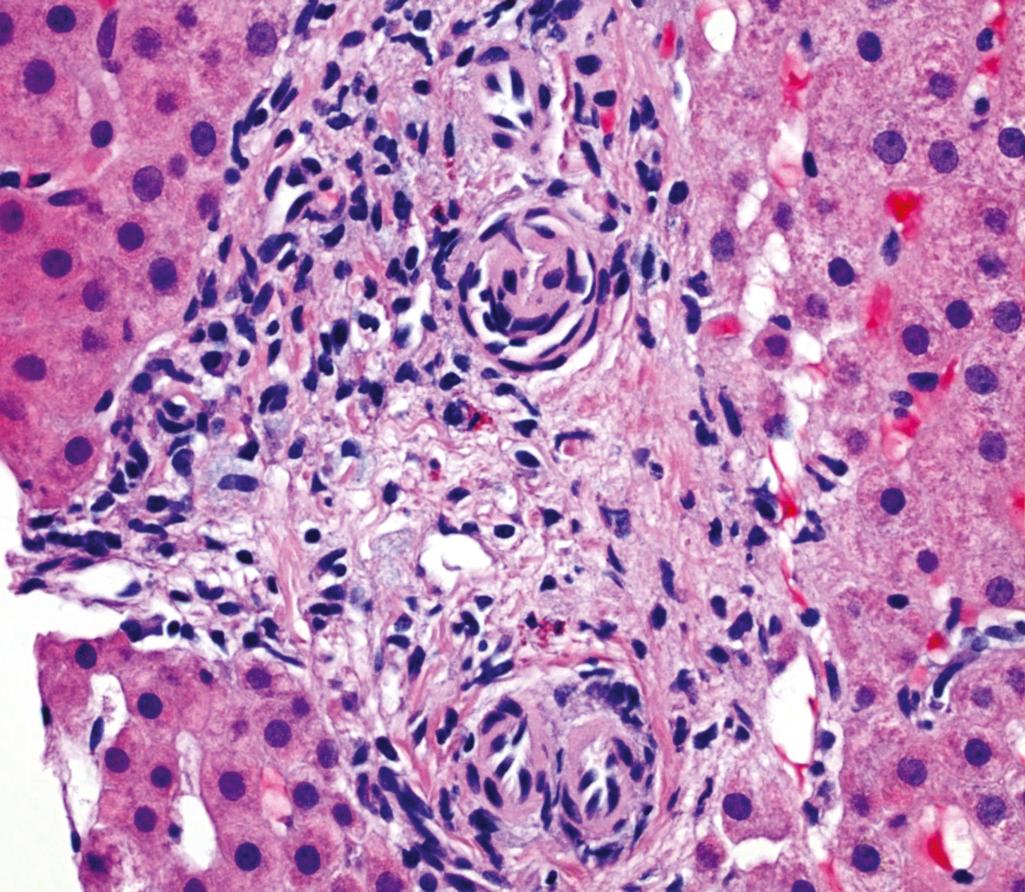
Portal inflammatory infiltrate predominantly composed of lymphocytes with or without interface hepatitis of varying severity (see Figure 7.1B )
Spotty or confluent necrosis with or without bridging necrosis
Portal fibrous expansion, periportal fibrosis, bridging fibrosis to cirrhosis (stages 1 to 4)
Specific features
HBV: ground-glass hepatocytes
HCV: lymphoid aggregates or follicles with or without germinal centers, focal mild macrovesicular steatosis, damaged interlobular bile ducts
Immunohistochemistry for hepatitis B core antigen (HBcAg), HBsAg, and hepatitis B e antigen (HBeAg)
Electron microscopy: HBsAg in hepatocyte cytoplasm (22-nm spheres and rods)
Serologic markers and virologic assays of viral infection are virtually essential to establish or exclude the diagnosis
Clinical history is important
Fatty change is typical but not always present
Many ballooned hepatocytes and Mallory-Denk bodies are usually seen
Megamitochondria may be seen
Lobular inflammatory foci (usually rich in neutrophils)
Perivenular and pericellular fibrosis (chicken-wire pattern)
Significant steatosis is present, predominantly macrovesicular
Zone 3 injury with lobular inflammatory foci pattern in adults
Zone 1 injury with portal inflammatory dominant pattern in children
Ballooned hepatocytes and Mallory-Denk bodies are typical findings
Megamitochondria may be seen
Perivenular and pericellular fibrosis (chicken-wire pattern) in adults
Fibrosis initiates in portal tracts in children
Serologic markers important (positive antinuclear antibody [ANA], anti–smooth muscle antibody [ASMA], or liver-kidney microsomal antibody [LKM])
Coexistent autoimmune diseases are common
Prominent plasma cells in the portal and periportal region or deep within the parenchyma
Marked interface hepatitis and parenchymal activity
Bridging necrosis is common and may form hepatitis rosettes
Seen more often after transplantation
Marked sinusoidal lymphoplasmacytic inflammatory infiltrate characteristically in single-file arrangement
Marked hepatocellular regeneration
EBV encoded RNA in situ hybridization may be helpful
Bile ductular reaction
Florid duct lesion with granuloma
Damage and loss of interlobular bile duct
Positive antimitochondrial antibody (AMA)
Cholestatic picture
Bile ductular reaction
Periductal fibrosis and loss of interlobular bile duct
Association with ulcerative colitis is common
Characteristic beading on endoscopic retrograde cholangiopancreatography (ERCP)
Clinical history is important (time course of drug use)
Negative serologic markers of viral infection
Serologic markers (viral and autoimmune), virologic assays, as well as the pattern of hepatic enzyme elevations are most important in distinguishing the many causes of hepatitis.
High mortality rate
Patients often have fever and right upper quadrant tenderness
Surgical drainage is often required
Bacterial abscesses are caused by portal spread of extrahepatic infection with Staphylococcus aureus, Salmonella typhi, and Treponema pallidum (syphilis)
Parasitic abscesses are caused by Entamoeba histolytica, Echinococcus species, malaria, Leishmania species, Ascaris lumbricoides , and liver flukes (e.g., Clonorchis sinensis, Fasciola hepatica , and Opisthorchis viverrini )
Bacteremic spread through arterial or portal system: multiple, soft, grossly necrotic lesions
Bacteremic spread by direct extension or trauma: solitary, large, soft, grossly necrotic lesions
Single or multiple soft well-circumscribed lesions (gummas) that eventually scar, resulting in hepar lobatum, which grossly resembles cirrhosis
Well-circumscribed lesion containing thick, dark material
Space-occupying cystic lesion with internal daughter cysts
Granular cyst contents (hydatid sand) composed of scolices and hooklets
Numerous foul-smelling cavities
Hepatomegaly (secondary Kupffer cell hyperplasia)
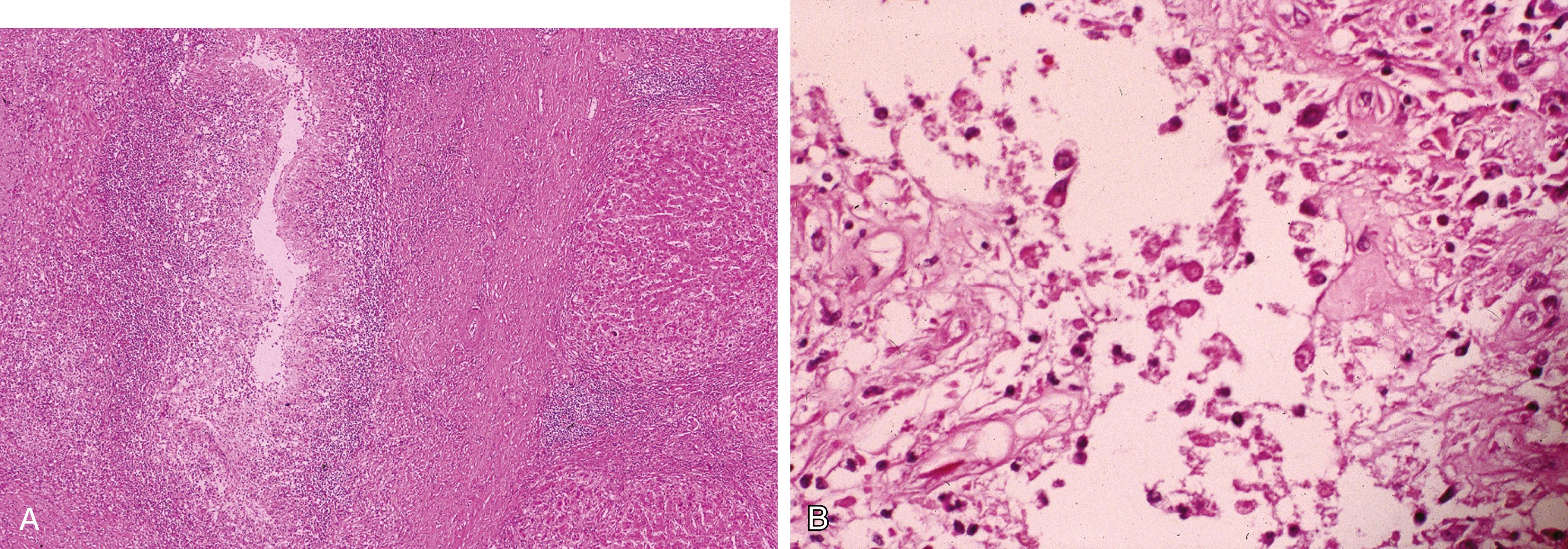
Marked neutrophilic infiltrate with hepatocyte destruction ( Figure 7.2A )
Congenital: neonatal hepatitis
Tertiary: gummas (granulomatous abscesses), which heal as dense scars
Necrotic debris with trophozoites at the periphery (see Figure 7.2B )
Outer laminated nonnuclear layer, inner nucleated germinal layer with attached capsules containing numerous scolices that are released into the cyst cavity and give rise to daughter cysts
Secondary cholangitis results from obstruction of intrahepatic bile ducts
Necrotic debris with granulomatous and eosinophilic response to degenerated parasites
Biliary epithelial hyperplasia, cholangitis, and periductal fibrosis
Kupffer cell hyperplasia and phagocytosis of ruptured erythrocytes
Kupffer cell hyperplasia and phagocytosis of organisms (Donovan bodies)
Gram stain: helps highlight bacteria
Warthin-Starry, Dieterle stain, or T. pallidum immunohistochemistry: syphilis
Giemsa stain to identify amastigotes: leishmaniasis
Direct examination for Echinococcus species scolices and liver flukes
Culture or nucleic acid tests may help identify organism
See earlier discussion for specific infection characteristics
Amebic abscesses are more likely to spread into the thoracic cavity.
Echinococcal cysts should be removed intact, due to risk of severe allergic reactions with disruption .
Clinical history important (e.g., ingesting an agent known to cause liver disease)
An appropriate time interval between exposure and onset of disease
A histologic lesion known to be associated with the suspect drug
Resolution of the lesion after withdrawal
Can be acute or chronic
Correlation with laboratory testing (e.g., acetaminophen level) may be helpful
Drug-specific clinical presentations and literature references are available from LiverTox ( http://livertox.nlm.nih.gov/ )
Different agents may result in different liver injury patterns, such as the following:
Zone 3 hepatocellular necrosis: acetaminophen
Mimicking acute viral hepatitis: antituberculous drugs, anesthetics, herbal medicine, nonsteroidal antiinflammatory drugs
Cholestasis with duct damage and duct loss: amoxicillin and clavulanic acid (Augmentin)
Vanishing bile duct: chlorpromazine, amoxicillin and flucloxacillin, haloperidol, temozolomide
Microvesicular steatosis: valproic acid, tetracycline, nucleoside analogues, salicylate (Reye syndrome)
Hypertrophic hepatic stellate cells and perivenular and pericellular fibrosis: hypervitaminosis A
Sinusoidal obstruction syndrome/veno-occlusive disease: pyrrolizidine alkaloids or chemotherapeutic agents associated with bone marrow transplantation
Steatohepatitis-like: amiodarone, tamoxifen, methotrexate
Hepatitis with features of autoimmune hepatitis: anti-TNFα immunomodulators, immune checkpoint inhibitors
Drug toxicity should always enter the differential diagnosis when abundant eosinophils or epithelioid granulomas are present or when hepatitis and cholestasis are both present
Noncontributory
Noncontributory
Positive serologic markers or viral nucleic acid tests
Immunohistochemistry may help to detect viral antigens (e.g., HBV, cytomegalovirus [CMV], herpes simplex virus [HSV], EBV)
Positive ANA, ASMA, and anti-LKM
Prominent plasma cells
Responds to corticosteroids
Imaging studies may help
Positive AMA
Florid duct lesion
Careful correlation of past and present history is essential, including use of herbal remedies and over-the-counter medications .
Rule out other liver diseases .
Nonspecific symptoms including malaise, anorexia, weight loss, and tender hepatomegaly with mild elevation of serum bilirubin and alkaline phosphatase
About 20% to 25% of heavy drinkers develop alcoholic steatohepatitis
Early: large, soft, greasy, yellow liver
Late: shrunken, mottled, red-brown liver with bile staining
End-stage: cirrhosis
Steatosis
Zone 3 injury pattern
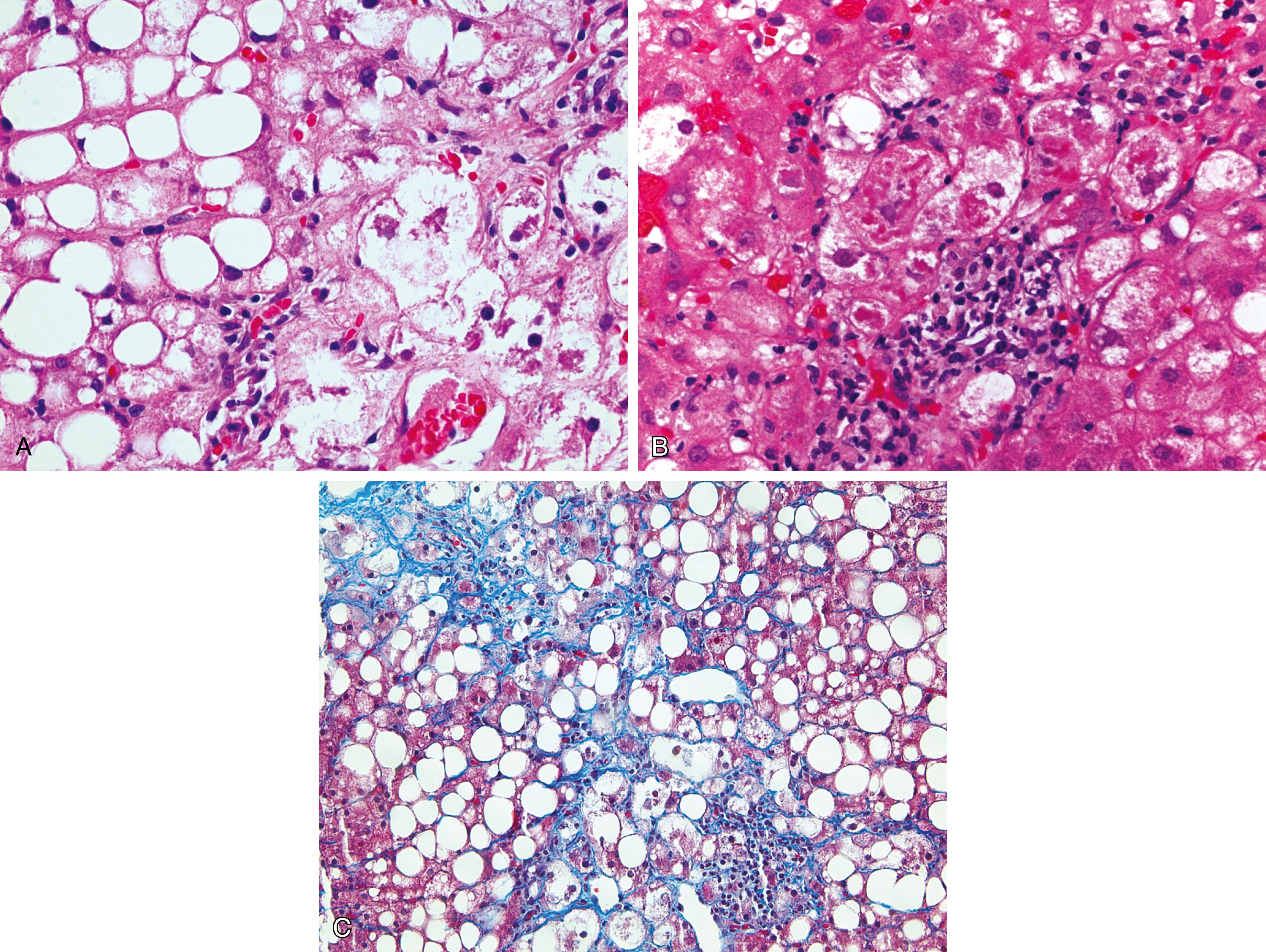
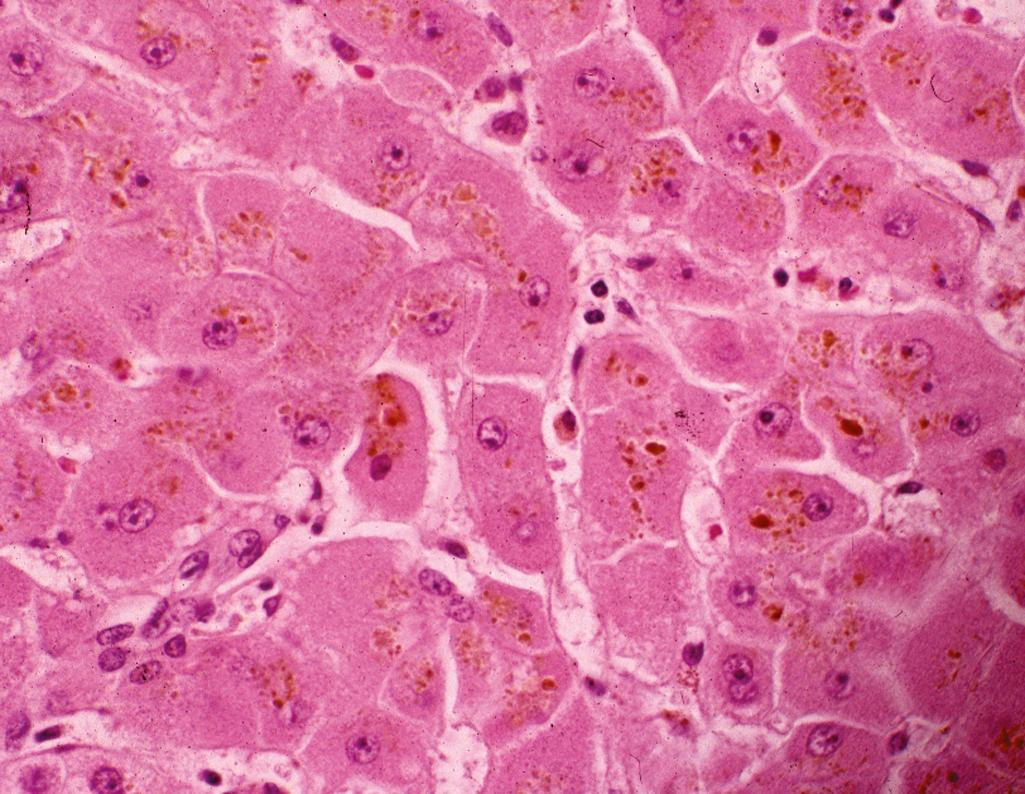
Ballooning degeneration ( Figure 7.3A )
Lobular inflammatory infiltrates, especially rich in neutrophils
Mallory-Denk bodies and megamitochondria (see Figure 7.3B )
Perivenular and pericellular fibrosis (see Figure 7.3C )
Bile ductular reaction
Sclerosing hyaline necrosis
Noncontributory
Noncontributory
Clinical history is essential
Positive serologic and/or virologic markers of viral infection
Hepatocellular injury and initiation of fibrosis are more marked in the periportal areas, as opposed to alcoholic steatohepatitis (perivenular and pericellular fibrosis and hepatocellular injury predominantly in zone 3 region)
Mallory-Denk bodies are more common in steatohepatitis
Typically occurs in third trimester of pregnancy
Steatosis is microvesicular
Steatosis is essential
Neutrophilic aggregates (satellitosis) are not common
Glycogenated nuclei are more common
Sclerosing hyaline necrosis or veno-occlusive lesion are not present
Major pathologic effects of alcohol are caused by interference with lipid metabolism, mitochondrial damage, and cytoskeletal injury .
Genetically determined susceptibility is thought to account for the fact that only 20% to 25% of heavy drinkers develop alcoholic steatohepatitis, whereas individuals with minimal to no alcohol intake may develop histologically identical nonalcoholic steatohepatitis .
A manifestation of the metabolic (insulin resistance) syndrome
Risk factors: central obesity, hyperglycemia, type II diabetes, arterial hypertension, and hypertriglyceridemia
Nonalcoholic steatohepatitis (NASH) is the progressive lesion of nonalcoholic fatty liver disease (NAFLD), which may progress to cirrhosis and liver failure
Histologically, NASH is almost identical to alcoholic steatohepatitis but occurs in individuals who do not have significant alcohol history
Early: large, soft, greasy, yellow liver
Late: shrunken, mottled, red-brown liver with bile staining
End-stage: cirrhosis
Nonspecific steatosis in NAFLD
Predominantly macrovesicular fatty change
Typically starts in a zone 3 centrilobular pattern
In adults, begins as a zone 3 injury pattern consisting predominantly of macrovesicular steatosis, ballooned hepatocytes, and lobular inflammation
In children, begins as a zone 1 injury pattern with steatosis and inflammation accentuated in periportal regions, and initiation of fibrosis in portal tracts
Pigmented macrophages and acidophile bodies can be seen
Cytoplasmic Mallory-Denk bodies (fibrillary eosinophilic material composed of intermediate cytokeratin filaments associated with ubiquitin)
Zone 3 perivenular and pericellular fibrosis (chicken-wire pattern), which progresses to central-portal bridging
Cirrhosis (end-stage disease)
A NAFLD activity scoring (NAS) system designed and validated by the NASH Clinical Research Network including assessment of steatosis, lobular inflammation, hepatocellular ballooning, and a separate staging scheme for fibrosis can be used after establishing the diagnosis of NASH for the evaluation of disease activity and stage before and after mitigation of NASH
Immunohistochemical stains for ubiquitin and p62 have been developed to identify Mallory-Denk bodies.
Rearrangement of the intermediate filament cytoskeleton in ballooned hepatocytes can be demonstrated by the loss of cytoplasmic keratin 8/18 immunostaining and may be evaluated as a marker for the more objective detection of hepatocellular ballooning in NASH.
Noncontributory
Clinical history is essential
Positive serologic/virologic markers of viral infection
Inflammation is more accentuated in the portal and periportal areas
Fibrosis initiates in portal regions
Mallory-Denk bodies are more common in steatohepatitis
Typically occurs in third trimester of pregnancy
Steatosis is microvesicular
Mallory-Denk bodies may be present and would most likely be seen in periportal as opposed to pericentral areas.
Mallory-Denk bodies may be present and would most likely be seen in periportal as opposed to pericentral areas
Marked copper overload
Occurs almost exclusively in India
Mallory-Denk bodies are often present
Steatosis conspicuously absent
Marked copper overload
Presence of Mallory-Denk bodies associated with lobular inflammatory infiltrates and steatosis (predominantly macrovesicular) in a zone 3 injury pattern suggests alcoholic or nonalcoholic steatohepatitis .
Mallory-Denk bodies may be present in other pathologic processes, including chronic cholestatic disease, Wilson disease, Indian childhood cirrhosis, and even HCCs (about 10%) .
Onset typically occurs during third trimester of pregnancy
Bleeding, nausea and vomiting, jaundice, and occasionally coma
Usually resolves after delivery
Greasy, small, pale-yellow liver
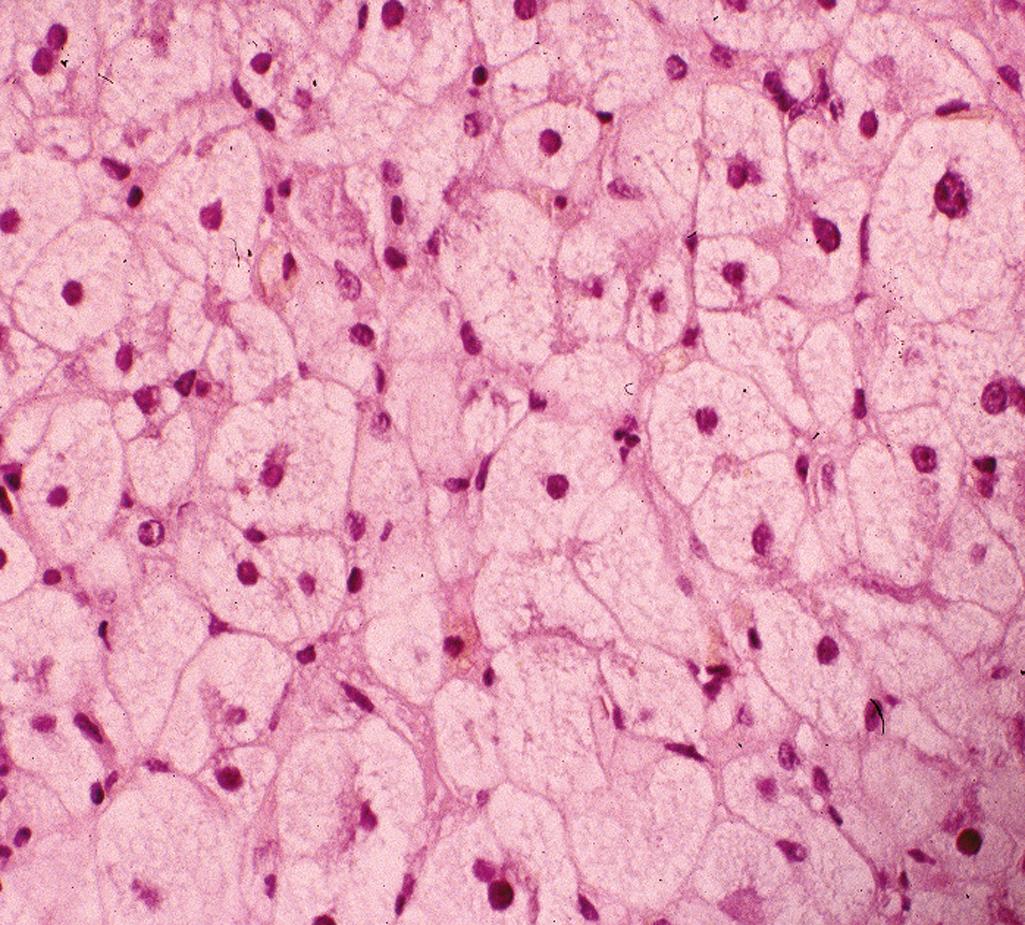
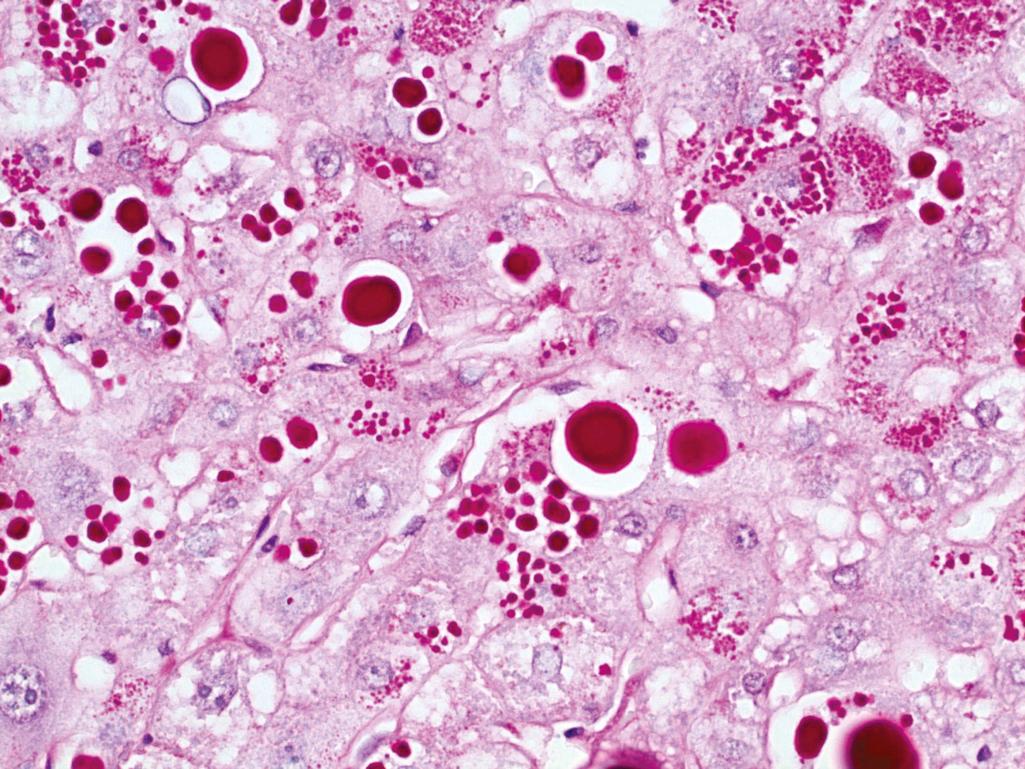
Microvesicular steatosis ( Figure 7.4 )
Canalicular and intrahepatocytic cholestasis may occur
Portal tract inflammation may be prominent
Oil red O (on frozen-section slide) demonstrates microvesicular fat droplets.
Noncontributory
Clinical history is essential
May show similar histologic features (e.g., tetracycline, valproic acid, nucleoside analogues), which are all associated with microvesicular fatty change
Clinical history is required for definitive distinction
Also shows microvesicular steatosis
History of aspirin use
Associated with encephalopathy
Typically shows macrovesicular steatosis
Shows lobular hepatitis and portal lymphoid aggregates
Mallory-Denk bodies are typically prominent and often associated with a neutrophilic infiltrate
Onset during pregnancy, usually third trimester
Pathogenesis: defective intramitochondrial fatty acid oxidation
Abnormal accumulation of iron in liver, pancreas, myocardium, and other organs
Hereditary: homozygous recessive, loss of function in the HFE gene
Acquired: multiple transfusions, Bantu hemosiderosis (alcoholic beverages brewed in iron drums in sub-Saharan Africa)
Most often presents in men older than 40 years
Liver is the most severely affected organ
Classic triad: cirrhosis, skin pigmentation, and diabetes mellitus (not as common now owing to early diagnosis and treatment)
Patients may also have abdominal pain, cardiac dysfunction, and atypical arthritis
Laboratory studies show increased serum iron and ferritin
Increased risk for developing HCC
Enlarged liver with dark-brown pigmentation
Ultimately leads to cirrhosis with persistent dark-brown pigmentation
Early: hemosiderin granules in cytoplasm of periportal hepatocytes
Middle:
Progressive iron deposition in lobules and eventually bile duct epithelium and Kupffer cells, resulting in hepatocyte necrosis, portal inflammation, and portal and bridging fibrosis ( Figure 7.5A )
Lobular inflammation typically absent
Late: fibrous septa develop over years with progression to cirrhosis with intense hemosiderin pigmentation
Prussian blue stain for iron highlights increased iron deposition (see Figure 7.5B )
Hepatic iron index (HII): biochemical quantitation of hepatic iron in fresh tissue or paraffin block calculated as micromoles of iron per gram dry weight divided by patient’s age
Homozygotes: HII greater than 2 (may be greater than 40)
Heterozygotes: less than 2
Normal individuals: less than 1
Nucleic acid testing for germline loss-of-function variants in the HFE gene, most commonly C282Y and/or H63D
Patients typically have a cause for secondary iron overload (e.g., multiple transfusions, porphyria cutanea tarda, or chronic dietary iron overload as in Bantu siderosis).
Common to have iron overload in cirrhosis due to nonbiliary etiology (e.g., HCV, alcohol, NASH)
Iron is directly hepatotoxic; no inflammatory mediators released .
Women are less commonly affected and present later as a result of physiologic blood loss during menstruation and pregnancy .
Treatment is reduction of iron overload by phlebotomy .
Abnormal accumulation of copper in liver, brain, eyes, and other organs
Variable age of onset
Autosomal recessive, mutations in the ATP7B gene encoding a copper transporter
Laboratory findings include decreased serum ceruloplasmin, increased hepatic copper, increased urinary excretion of copper
Serum copper levels not helpful
Most commonly presents with acute or chronic liver disease
Neuropsychiatric symptoms are also frequent at presentation secondary to involvement of basal ganglia
Kayser-Fleischer rings are diagnostic (green-brown deposits of copper in Descemet membrane in limbus of cornea)
Liver eventually becomes cirrhotic
Excessive copper granules in hepatocytes can only be seen with special stain ( Figure 7.6 )
Mild to moderate fatty change
Focal hepatocyte necrosis
Glycogen vacuoles in hepatocyte nuclei
Mallory-Denk bodies in periportal hepatocytes
Acute and chronic hepatitis
Cirrhosis following chronic hepatitis
Rarely, massive liver necrosis
Rhodanine stain for copper positive
Orcein stain for copper-associated protein positive
Quantitation of hepatic copper in fresh tissue or paraffin block (more than 250 μg copper/1 g dry liver), typically with mass spectrometry
Sequencing of ATP7B gene
Serologic/virologic markers are positive
No accumulation of copper
Lesser degree of copper accumulation
Normally free copper is absorbed in the stomach and duodenum, weakly bound to albumin, transferred to hepatocytes, and incorporated into α 2 -globulin to form ceruloplasmin, which is re-secreted into plasma; senescent ceruloplasmin is taken up by hepatocytes, degraded by lysosomes, and copper excreted into bile .
Wilson disease gene is ATP7B on chromosome 13 and encodes a transmembrane copper-transporting adenosine triphosphatase (ATPase) located on canalicular membrane of hepatocytes .
Treatment is copper chelation with D-penicillamine .
Variable age of onset
Autosomal recessive disease caused by mutations of the SERPINA1 gene on chromosome 14
Absent or decreased α 1 -antitrypsin activity results in unchecked activity of neutrophilic elastase leading to pulmonary emphysema (destruction of elastic fibers supporting alveolar spaces)
The most common variant protein (E366K) associated with liver disease is abnormally folded, resulting in impaired transport to the Golgi and accumulation in the endoplasmic reticulum of hepatocytes
In some patients, there is liver disease without pulmonary emphysema owing to functional mutant forms that inhibit neutrophil elastase but that are not appropriately degraded in hepatocytes
Clinical hepatic presentations range from:
Neonatal hepatitis with cholestatic jaundice
Young adults with recurrent attacks of hepatitis that either resolve or lead to chronic hepatitis and cirrhosis
Middle-aged to older adults with cirrhosis after a clinically silent course
Increased risk for HCC, especially in homozygous patients
Successful liver transplantation is curative
Augmentation therapy with intravenous α 1 -antitrypsin delays the natural course of lung disease, but does not impact liver disease
Noncontributory
Round to oval, variably sized eosinophilic globules most concentrated in periportal hepatocytes
Otherwise variable histologic features
Neonatal hepatitis with or without cholestasis
Chronic hepatitic picture
Cirrhosis
Eosinophilic globules are positive for periodic acid–Schiff (PAS) and resistant to diastase digestion ( Figure 7.7 )
Immunohistochemistry for α 1 -antitrypsin highlights eosinophilic globules
Serum α 1 -antitrypsin quantitation (<85 mg/dL is highly predictive)
Serum protein electrophoresis with reduction in alpha-1 band (not specific)
Identification of common variant proteins by mass spectrometry, or genetic variants by allele-specific PCR or sequencing of SERPINA1
Identification of mutant proteins by isoelectric focusing
About 75 variants identified and named alphabetically according to migration on isoelectric gel
Normal genotype is PiMM
PiZZ is the most clinically significant genotype and shows the highest association with carcinoma
Patients with PiMZ genotype have 50% normal α 1 -antitrypsin and 50% mutant form
Other mutant alleles include S (reduced levels of α 1 -antitrypsin but no clinical disease unless inherited in combination with another mutation) and null (no detectable protein)
Other types of chronic hepatitis include viral, drug, and autoimmune hepatitis, but they do not demonstrate the PAS-positive and diastase-resistant globules that are characteristic of α 1 -antitrypsin deficiency
α 1 -Antitrypsin deficiency is one of the few liver diseases that can still be diagnosed in an end-stage liver explant because of the PAS-positive and diastase-resistant globules that remain in the hepatocyte cytoplasm.
This is a multifactorial disease in which there are heterogeneous genetic mutations, resulting in highly variable clinical presentations even among members of individual families .
Young and middle-aged women (female-to-male ratio of 7:3)
Often associated with extrahepatic autoimmune disorders such as rheumatoid arthritis, thyroiditis, Sjögren syndrome
Hyperglobulinemia
Characterized by serum autoantibodies, classically ANA, ASMA, soluble liver antigen (SLA), and anti-LKM1
Negative viral serologic/virologic markers
Responsive to immunosuppressive therapy
Noncontributory
Significant portal and periportal inflammatory infiltrate with lymphocytes and plasma cells (prominent plasma cells are the hallmark) ( Figure 7.8 )
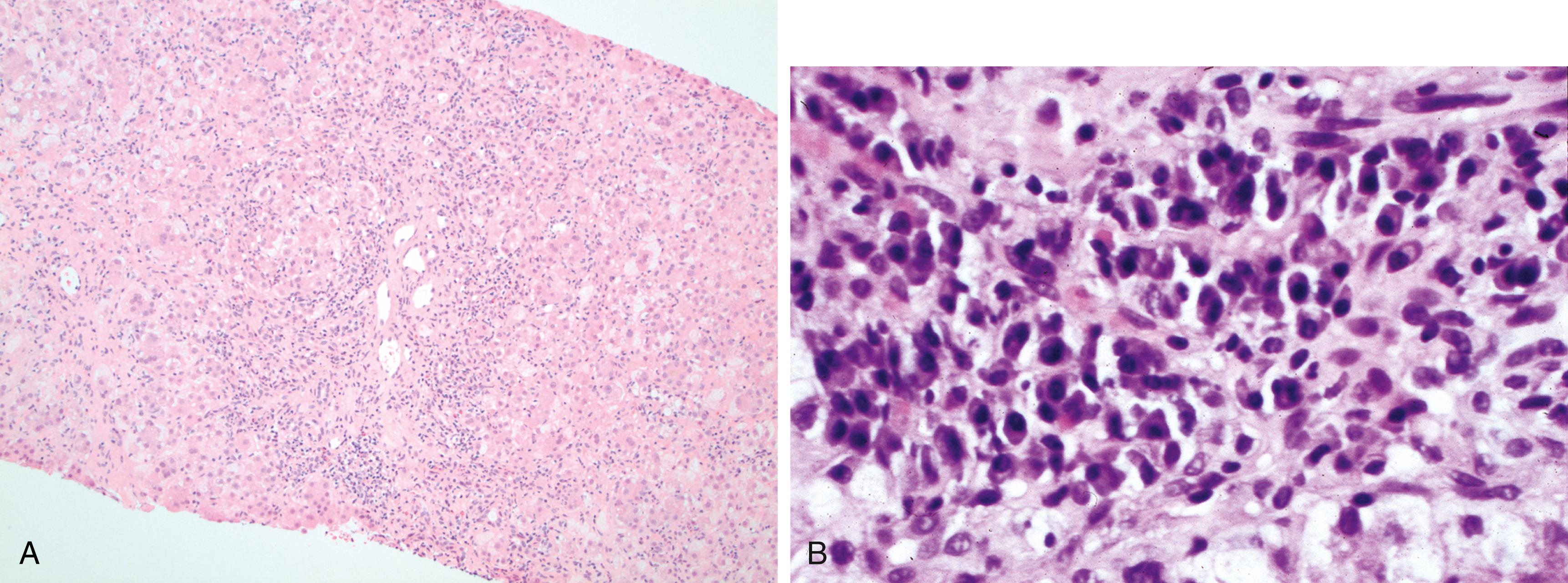
Marked lobular inflammatory infiltrate with prominent plasma cells deep in the parenchyma
Increased lobular acidophil/apoptotic bodies
Prominent interface hepatitis
Bridging/confluent necrosis is common
Severe hepatocellular injury with hepatitic rosette formation and syncytial giant hepatocytes
Noncontributory
Noncontributory
Clinical correlation and medication history including over-the-counter drugs is important in the differential diagnosis of this disease.
Positive virologic and serologic markers
Plasma cells less prominent
Milder lobular hepatitis and interface hepatitis (especially in HCV)
Most frequent in young women and associated with hyperglobulinemia and various serologic markers of autoimmune disease
Rosette formation, although not specific, is highly suggestive of autoimmune hepatitis
This is one of the few forms of chronic hepatitis that responds well to immunosuppressive therapy
Most commonly occurs in middle-aged women
Serum AMA positive in more than 90% of cases
Insidious onset, with pruritus being the most common presenting symptom and jaundice developing later
Elevated serum alkaline phosphatase, with hyperbilirubinemia developing later
Chronic and progressive, with cirrhosis developing only after many years
Early: unremarkable
Late: finely granular capsule; bile-stained parenchyma
Ultimately liver becomes cirrhotic (biliary type cirrhosis)
Variability in stages of lesions (i.e., coexistence of different stages in single specimen)
Stage I (florid duct lesion) : focal destruction of small and medium-sized bile ducts by granulomatous inflammation; bile duct epithelium irregular and hyperplastic; dense portal tract infiltrate of lymphocytes, macrophages, plasma cells, and eosinophils ( Figure 7.9 )
Stage II (ductular reaction) : disappearance of small bile ducts; scarring of medium-sized bile ducts; proliferation of bile ductules in portal tracts; inflammation and interface hepatitis of adjacent periportal hepatic parenchyma
Stage III (scarring) : small and medium-sized ducts scarce; little inflammation in fibrous septa or parenchyma; lymphoid aggregates with or without PASD-positive material representing residual basement membrane material in areas where ducts have been lost
Stage IV (cirrhosis) : cirrhosis, often with a jigsaw pattern
Noncontributory
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here