Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Helminthic infections comprise a great variety of worms that parasitize virtually every organ in the human body. Although helminthic infections occur throughout the world, they are more common in the subtropics and tropics. This is usually related to climatic factors, human customs, and occurrence in countries with less well developed systems of sanitation and education. Human infections are usually acquired when someone ingests the parasite, the parasite penetrates the skin, or the parasite is introduced during the bite of a vector. Many worms require intermediate hosts to complete their life cycles, such as fish, snails, crustaceans, and insects. Thus, the travel history of the patient is frequently the key to determining the genus and species of the pathogenic worm. Lesions can be caused by immature adult worms, mature adult worms, larvae, eggs, or a combination. Because most worms are unable to multiply in their host, they have developed complex and elaborate reproductive organs to ensure survival. It is estimated that Ascaris lumbricoides female worms can produce 200,000 eggs per day.
There are three major groups of worms that cause disease in humans: cestodes (tapeworms), trematodes (flukes), and nematodes (roundworms). All tapeworms are parasitic and belong to the phylum Platyhelminthes and class Cestoda. Tapeworms are dorsoventrally flattened, have a head (scolex), are segmented (proglottids), are hermaphroditic, have no body cavity, and have no digestive system. Nutrients are absorbed through the living tegument. Most tapeworms that infect humans are listed in Table 27-1 . Adult tapeworms live in the intestinal lumen where they produce proglottids that pass in the feces. Proglottids may not be recognized by their gross appearance and may be processed in the laboratory for further identification by the pathologist. The most serious infections by tapeworms, however, are those caused by their larvae (metacestodes). There are four major metacestodes that invade tissue and infect humans: cysticercus, sparganum, coenurus, and echinococcus cyst.
| Cestodes | Trematodes | Nematodes | |
|---|---|---|---|
| More common * | Taenia saginata proglottids, T. solium proglottids and cysticerci, Dipylidium caninum proglottids, Spirometra species larvae (spargana), Echinococcus species larvae (hydatid cyst) | Schistosoma species , Paragonimus species | Strongyloides stercoralis, Dirofilaria species , Enterobius vermicularis, Trichuris trichiura, Ascaris lumbricoides, Anisakis simplex |
| Less common * | Diphyllobothrium latum proglottids , Hymenolepis nana and H. diminuta proglottids, Taenia multiceps, and T. serialis larvae (coenuri) | Fasciola species , Clonorchis sinensis, Opisthorchis species , Fasciolopsis buski | Trichinella spiralis, Ancylostoma duodenale, Necator americanus, Wuchereria bancrofti, Brugia species , Dracunculus medinensis, Onchocerca species , Capillaria species , Mansonella species , Loa loa, Toxocara species , Angiostrongylus species , Pseudoterranova decipiens |
| Rare * | Mesocestoides species, Bertiella species , Raillietina species , Inermicapsifer madagascariensis proglottids | Heterophyes heterophyes, Metagonimus yokogawai, Metorchis conjunctus, Dicrocoelium species , Gastrodiscus hominis, Echinostoma species , Nanophyetus salmincola | Ancylostoma braziliense, Baylisascaris procyonis, Gnathostoma species , Halicephalobus deletrix, Oesophagostomum species , Ternidens diminutus, Lagochilascaris minor, Mammomonogamus laryngeus, Dioctophyma renale, Trichostrongylus species , Uncinaria stenocephala |
* More common, less common, and rare do not refer to overall prevalence of infection but to the probability of observing the parasite in a histologic section. The authors acknowledge that dividing the list of parasites into categories is subjective and is not intended to be exhaustive.
All flukes are parasitic and belong in the phylum Platyhelminthes and class Trematoda. Flukes are also dorsoventrally flattened, are frequently leaf-shaped, usually have oral and ventral suckers, and are hermaphroditic. They also have no body cavity, an incomplete digestive tract, and a living tegument that allows absorption of nutrients. Most produce operculated eggs (i.e., all except the schistosomes). The blood flukes (schistosomes) are unique among flukes in that they live in the lumens of blood vessels, the sexes are separate (diecious), and their eggs are nonoperculate. Most trematodes that infect humans are listed in Table 27-1 . Unlike adult tapeworms, most adult flukes invade human tissue where they themselves or deposited eggs cause lesions. Most fluke disease is attributed to the host reaction to egg deposition. This is especially true of the schistosomes because their eggs are laid within the lumens of blood vessels and can be transported by the circulatory system to most organs. Larval trematodes do not usually cause significant disease.
The nematodes (roundworms) are by far the largest group of worms to infect humans. Nematodes belong to the phylum Aschelminthes and the class Nematoda. Nematodes have bodies that are cylindrical, elongate, and bilaterally symmetric. Sexes are usually separate, and males are smaller than females. The body is covered with a tough, resistant, nonliving cuticle for protection. There is a body cavity (pseudocele), a complete digestive tract with mouth and anus, and a body wall with a single layer of smooth muscle cells. Most nematodes that infect humans are listed in Table 27-1 . The nematodes are an enormous group, and they vary greatly in size, morphologic features, and behavior. Nematode infections in humans can be caused by immature adult worms, mature adult worms, larvae, or eggs. Some species of nematodes lay eggs that hatch in human tissue, liberating larvae that migrate through the tissue, whereas others produce free larvae that likewise penetrate tissue. Filarial worms constitute a unique category in that their larvae (microfilariae) either circulate in the bloodstream or migrate through the tissues. Adult nematodes in histopathologic sections are best studied in transverse section.
Many cestode infections are diagnosed by identifying gross tapeworm proglottids or eggs passed in feces, but these methods will not be further emphasized. The most serious cestode infections are diagnosed upon identification of the larval tapeworm in human tissue. Occasionally, embedded and processed proglottids are available for diagnosis. For the following discussion we have selected to emphasize diseases caused by Taenia solium, Spirometra species, and Echinococcus granulosus because they are the most commonly encountered in the United States and show the greatest diversity.
TAENIA SOLIUM
Taenia solium, the pork tapeworm, has a worldwide distribution. Human infections are more common in countries where raw or insufficiently cooked pork containing cysticerci is consumed. Humans are the only known definitive host. Humans can also serve as an intermediate host upon ingestion of T. solium eggs that hatch and eventually develop into metacestodes (cysticerci).
Human infection with adult T. solium is usually asymptomatic but may be associated with minor gastrointestinal symptoms. Tissue infections with the metacestode larvae of T. solium (cysticercosis) may involve many parts of the body but rarely cause serious disease except when there is cardiac or central nervous system (CNS) involvement. Patients may harbor both adult worms and cysticerci, which can arise from autoinfection. Cysticercosis of the CNS (neurocysticercosis) is the most common cause of acquired epilepsy in endemic areas (e.g., Mexico, South and Central America, the Philippines, and Southeast Asia) and possibly the most common cause of epilepsy in the world. Neurocysticercosis affects males and females equally and has a peak occurrence in young adults 25 to 35 years old, although infection probably peaks at an earlier age (5 to 15 years). Cysts generally become symptomatic when they begin to die and elicit an inflammatory host response. Clinical manifestations of neurocysticercosis vary depending on the location of the cysts. In addition to seizures, headache and mass effects due to intracerebral lesions, hydrocephalus, chronic meningitis, and compression of the spinal cord have been associated with cysts in intraventricular, subarachnoid, and spinal cord locations, respectively. Fever is not a common feature of neurocysticercosis.
Taenia solium taeniasis is usually one adult tapeworm passing proglottids in an asymptomatic patient.
Taenia solium cysticercosis is the development of the larval stage (metacestode) that can occur in any organ of the body with serious complications and even death (neurocysticercosis).
Taenia solium taeniasis occurs worldwide wherever raw or undercooked pork is eaten, but it is rarely acquired in the United States; Taenia solium cysticercosis occurs throughout much of the world where impoverished conditions and personal hygiene tend to be poor.
Neurocysticercosis is one of the most common parasitic infections of the brain, causing seizure disorders and afflicting more than 2.5 million people worldwide.
Intestinal infections with adult T. solium are usually asymptomatic.
Although cysticerci can infect any part of the body, CNS involvement (neurocysticercosis) accounts for most of the clinically significant lesions.
Presenting symptoms of neurocysticercosis vary, but seizures, headache, and focal deficits are common.
The prognosis for intestinal infection with adult T. solium (taeniasis) is good.
Treatment with oral medications niclosamide or praziquantel is effective.
The prognosis of neurocysticercosis is variable, and worldwide an estimated 50,000 fatal cases occur per year.
Treatment of neurocysticercosis is controversial but earlier detection has led to a greater likelihood that pharmacologic treatment will be sufficient. This may include antiepileptic drugs, cysticidal agents (i.e., albendazole and praziquantel), and anti-inflammatory medications.
Surgery may be necessary.
Taenia solium adult tapeworms consist of up to 1000 proglottids and may reach a length of 9 m. The scolex has an armed rostellum with a double row of hooklets and four cuplike suckers. Gravid proglottids are nearly twice as long as broad, and the uterus has 7 to 13 lateral branches per side. Eggs have a thick radially striated shell and measure 31 to 43 μm in diameter. The metacestode stage (cysticercus) is a milky white, fluid-filled cyst, usually 1 to 2 cm in diameter, with a single invaginated protoscolex.
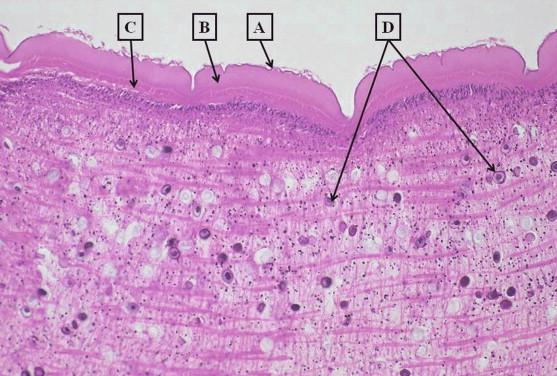
Taenia solium and T. saginata proglottids are usually viable when passed in the feces, and when processed by the laboratory into histologic sections they are readily identifiable by their morphologic features. The proglottids of these two species are similar and the eggs are virtually identical. It is difficult to separate these two species based on the number of uterine branches in histologic sections. Taenia species proglottids can be identified by their microvilli-lined tegument, smooth muscle, and calcareous corpuscles in a loose parenchyma ( Figure 27-1 ). Taenia species eggs in histologic sections are 30 to 35 μm in diameter and have a thick radially striated shell ( Figure 27-2 ). Taenia species gravid proglottids can be distinguished from those of Dipylidium caninum, the dog tapeworm that occasionally infects children, because the eggs of the latter occur in packets ( Figure 27-3 ).

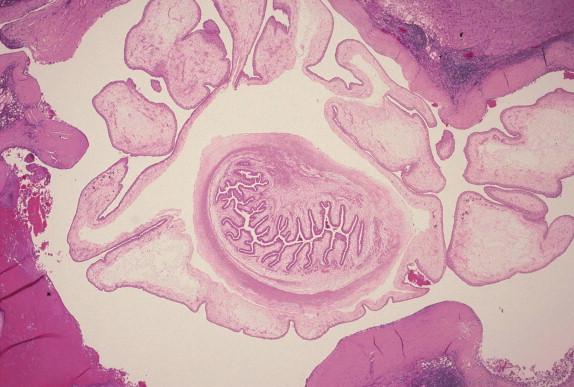
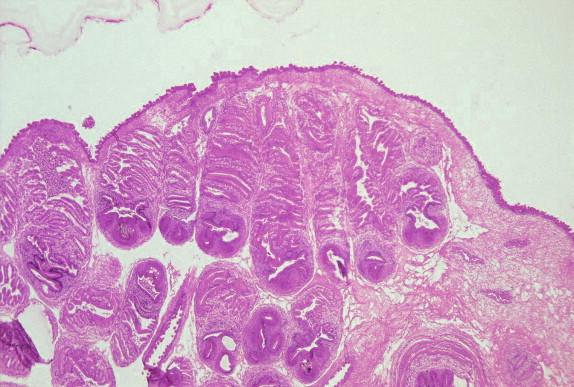
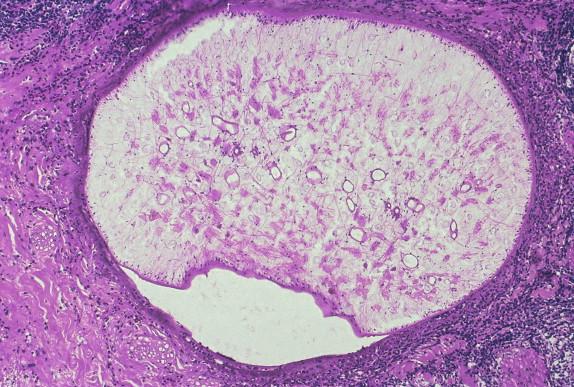
Taenia solium cysticerci are fluid-filled cysts with a single invaginated protoscolex. The tegument and bladder wall are morphologically similar to those of proglottids except thinner. Viable cysticerci sectioned through a plane that demonstrates the invaginated neck region or protoscolex are easily recognizable ( Figure 27-4 ). The diagnosis can be difficult if the histologic section contains only a fragment of the cyst wall and no neck region or protoscolex. Occasionally an aberrant form of cysticercus (cysticercus racemosus) develops in humans with a predilection for the base of the brain and subarachnoid space. Cysticercus racemosus produces no protoscolices, but the bladder wall proliferates extensively forming irregular masses resulting in a pattern resembling a compact cluster of grapes. Viable cysticerci may compress surrounding structures but usually cause minor host response. In contrast, dying or dead cysticerci provoke an intense inflammatory exudate comprised of neutrophils, eosinophils, histiocytes, and fibrin. Eventually, the lesion develops into granulomatous inflammation with formation of epithelioid cells and giant cells. The terminal event is fibrosis and calcification. A presumptive diagnosis of cysticercosis may be rendered upon finding only calcareous bodies (10- to 20- μm diameter laminated rings), providing all other known circumstances are supportive. Coenuri, the metacestode larvae of Taenia multiceps and T. serialis, have similar morphologic features to cysticerci but can be distinguished by the presence of multiple invaginated protoscolices ( Figure 27-5 ).
The most practical approach to the diagnosis of adult T. solium infection is the examination of feces for eggs or proglottids. Samples taken on several successive days may be needed, and concentration techniques may improve sensitivity. Care must be taken to avoid ingestion of eggs because they are infective.
Neurocysticercosis may be suspected based on imaging studies (computed tomography [CT] or magnetic resonance imaging [MRI]). Examination of cerebrospinal fluid (CSF) may reveal lymphocytic or eosinophilic pleocytosis, low glucose, and high protein levels.
Serology is available commercially or through the Centers for Disease Control and Prevention (CDC), which indicates prior exposure to T. solium , but cross- reactivity may occur with other cestode antigens. Negative serology does not exclude the diagnosis in the presence of characteristic CT and MRI results. Immunoblotting with the purified glycoprotein fraction of the cyst fluid may be a more sensitive and specific method.
The differential diagnosis of adult T. solium taeniasis includes other tapeworms particularly T. saginata . DNA probes can reportedly differentiate the two species, if this has not been possible from examination of proglottids or eggs. The differential diagnosis of neurocysticercosis is broad due to the number of different CNS sites that may be involved and the inflammatory response of the host.
Gliomas, cavernous malformations, and echinococcal cysts are differential diagnostic considerations for subarachnoid neurocysticercosis. Carcinomatous meningitis and granulomatous meningitis (sarcoidosis and mycobacterial, fungal, and syphilitic meningitis) are considerations when there is chronic basal arachnoiditis. Choroid plexus cysts, ependymal cysts, and colloid cysts are considerations for intraventricular neurocysticercosis.
The differential diagnosis of other cystic CNS lesions of parasitic, congenital, or traumatic origin may be considerations. Neurocysticercosis should also be considered in patients with brain infarction who are younger than 40 years old, are from endemic areas, and lack a predisposing factor.
Niclosamide and praziquantel are two oral medications that are effective in treating adult T. solium intestinal infections. Some authors suggest using a mild laxative 1 to 2 hours after niclosamide treatment to avoid the possibility of internal autoinfection. Additional considerations apply during pregnancy.
Neurocysticercosis is not a single disease entity, and treatment depends on a variety of clinical factors. Medical treatments include antiepileptic drugs, cysticidal agents (i.e., albendazole and praziquantel), and anti-inflammatory medications. Surgery may be necessary (e.g., for shunt placement), but earlier diagnosis has made it more likely that pharmacologic treatment alone will be sufficient.
Adult Taenia solium attach to the intestinal mucosa by its scolex, which may result in mild local inflammation of the mucosa, but there is minor pathologic change of the intestine.
Viable cysticerci can be obstructive and compress adjacent structures, but they usually cause only a mild host response.
Dying and degenerating cysticerci cause significant histopathologic changes including acute and chronic inflammation with neutrophils, histiocytes, eosinophils and fibrin, granuloma formation, fibrosis, and eventually calcification.
The prognosis for adult T. solium intestinal infections is good, but that for neurocysticercosis is variable depending on the location of lesions, the inflammatory response, and associated complications. A conservative estimate is that worldwide 50,000 deaths occur each year due to neurocysticercosis.
SPIROMETRA SPECIES (SPARGANOSIS)
Sparganosis is caused by at least four species of Spirometra larvae, pseudophyllidean tapeworms. Sparganosis is most common in Southeast Asia but can be acquired in the United States. Dogs and cats, among other animals, serve as definitive hosts, whereas humans serve as second intermediate and paratenic hosts. Humans can become infected with spargana in three ways: (1) drinking water contaminated with infected Cyclops (procercoid larva), (2) consuming a sparganum (plerocercoid larva) in improperly cooked flesh of a second intermediate or paratenic host (amphibian, reptile, bird, mammal), or (3) applying poultices of an infected second intermediate or paratenic host to an open wound.
An extremely rare form of sparganosis, not completely understood but thought by some to be caused by Spirometra (Sparganum) proliferum, occurs when the sparganum begins uncontrolled proliferation by branching and budding. Lesions usually begin as subcutaneous nodules, but the proliferating sparganum can disseminate to any part of the body seeding the tissues with thousands of variously sized spargana.
Up until 1996, 62 cases of sparganosis had been reported in the United States mainly from the Southeast. Spirometra mansonoides is the species most frequently encountered in U.S. Gulf States. Japan and Korea reportedly have the highest prevalence of sparganosis, mainly due to diet-associated infections. Ingestion of contaminated water is the most common source of infection in the Western Hemisphere. Imported cases from Southeast Asia may have been acquired as long as 19 years prior to diagnosis. Most commonly sparganosis presents as a slow-growing subcutaneous mass that may be migratory. Multiple other sites of involvement have been reported, including the breast, lung, abdominal cavity, genitourinary tract, and heart. The most serious infections involve the eyes and CNS. Infections in the CNS can present in a variety of ways depending on the size and location of the lesion, but seizures, headache, and hemiparesis are commonly reported. Vasculitis with stroke has also been reported. Ocular involvement can lead to blindness.
Spirometra mansonoides spargana cause most sparganosis acquired in the United States; humans serve as second intermediate or paratenic hosts, but not as definitive hosts, because spargana are unable to complete their development into adult tapeworms.
Human infections are widely distributed, but China, Japan, and Southeast Asian countries report most cases; although spargana can develop in many organs, subcutaneous tissue and skeletal muscle are the most common sites; spargana developing or migrating to the CNS cause the most serious disease.
Cutaneous sparganosis commonly presents as a subcutaneous or intramuscular nodule that migrates over days to months.
CNS infections commonly present with seizures, headache, and hemiparesis.
Tunnel signs in postcontrast MRI can be seen in cerebral sparganosis.
Punctate calcifications “calcospherules” within the parasite are best seen with CT.
Antiparasitic medications have had limited effect with peripheral sparganosis and no effect in the CNS.
Surgical removal of the nonproliferating sparganum is considered curative.
Human proliferative sparganosis ( S. proliferum ) may be fatal, and surgical removal is usually unsuccessful.
Spargana are white, flat, ribbon-like worms that vary from a few mm up to 50 cm in length. They may vary considerably in width and usually have a vertical groove at the anterior end but lack cuplike suckers and hooklets. Spargana migrate readily and frequently will crawl out of a surgical incision.
Spargana are elongate, flat, solid-bodied larvae that may appear spherical in histopathologic sections. The living tegument is lined with microvilli, allowing for the absorption of nutrients. The parenchyma is a loose stroma containing smooth muscle cells, branching excretory channels, and calcareous corpuscles ( Figure 27-6 ). They have no reproductive organs. Apparently viable spargana can cause an inflammatory response including abscess formation, chronic inflammation, and tissue eosinophilia. As the worm disintegrates, it provokes granuloma formation with palisading epithelioid cells and giant cells. Eventually the worm is completely destroyed and what remains is a tortuous tract with central caseation necrosis.
There may be eosinophilia in blood samples that can be pronounced. Peripheral eosinophilia is common in CNS infections, but curiously cerebrospinal fluid (CSF) eosinophilia is not a reported feature.
Imaging studies, of CNS lesions, especially CT and MRI, can be quite characteristic. In particular there may be a tunnel sign in postcontrast MRIs. Punctate calcifications, “calcospherules,” within the parasite are better seen by CT. Repeat imaging has been recommended to identify changes in the size and location of lesions to indicate that the organism is still alive and that its surgical removal is indicated.
Enzyme-linked immunosorbent assay (ELISA) of serum or CSF for sparganosis-specific antibody is sensitive and specific. Identification of the organism in histopathologic specimens provides definitive diagnosis but may not always be surgically possible. A preoperative diagnosis of cerebral sparganosis could reportedly be established based on clinical data, positive ELISA results, and characteristic imaging findings.
The differential diagnosis of cutaneous sparganosis includes other parasitic diseases that can present as migrating subcutaneous masses, including gnathostomiasis, paragonimiasis, loiasis, and dracunculiasis. A longstanding lesion that becomes calcified may clinically mimic varicose veins. Other inflammatory and neoplastic conditions may enter the differential diagnosis.
Cerebral sparganosis has a differential diagnosis that includes primary and metastatic brain tumors and other inflammatory granulomatous processes.
The prognosis is good for subcutaneous and intramuscular nonproliferative sparganosis if the organism is removed surgically. Ocular and CNS lesions can have significant sequelae including hemiparesis and blindness.
Antiparasitic treatment (praziquantel) has reportedly had limited success in treating peripheral sparganosis and no effect on spargana in the CNS. Surgical excision of the organism in the CNS may therefore give the best response.
Human proliferative sparganosis caused by S. proliferum, a type of sparganum that buds and branches and that may become widely disseminated, may result in death, as attempts at surgical removal are usually unsuccessful. The usual species seen in sparganosis acquired in the United States, Spirometra mansonoides, is nonproliferating.
Spargana are very long, and one particular section may be viable and provoke minimal histopathologic changes, whereas a disintegrating portion will cause major tissue damage; spargana may cause abscess formation, granuloma formation, and caseation necrosis; spargana usually incite a tissue eosinophilia.
ECHINOCOCCUS SPECIES, LARVA (HYDATIDOSIS)
Echinococcosis more accurately refers to infections caused by adult tapeworms in the definitive host, which humans are not. Hydatidosis and hydatid disease are more appropriate terms and refer to infection by the Echinococcus larva (metacestode). At least four species of Echinococcus larvae cause disease in humans. Echinococcus multilocularis causes alveolar hydatid disease, is focally distributed throughout the world, and is the second most common echinococcal larval tapeworm infecting humans. Echinococcus vogeli causes polycystic hydatid disease and prevails in Central and South America. Echinococcus oligarthus also causes polycystic hydatid disease and occurs in Central and South America. Echinococcus granulosus causes cystic hydatid disease and is the most common cause of hydatid disease. Therefore, the following discussion is limited to E. granulosus infections.
Echinococcus granulosus has a worldwide distribution but is a more serious problem in sheep- and cattle-raising regions. Dogs are the most common definitive hosts, but many other animals are also infected including wolves, foxes, and cats. The adult tapeworm is minute, consisting of a piriform scolex with armed rostellum and four suckers followed usually by only three proglottids. Echinococcus granulosus eggs are morphologically indistinguishable from most Taenia species eggs. A variety of animals serve as intermediate hosts, including sheep, cattle, pigs, and horses. Humans are usually an accidental dead-end host. Intermediate hosts acquire their infections by ingesting infective eggs that eventually develop into larval hydatid cysts. Hydatid cysts can develop anywhere in the human body, but the liver is the most common site. The definitive host becomes infected by feeding on the viscera of animals contaminated with hydatid cysts. Hydatid cysts in human liver grow slowly, about 1 mm in diameter per month.
The initial stage of infection following oral ingestion of E. granulosus eggs is asymptomatic, and the infection may remain so for years or even for life. The development of morbidity is related to several factors including the number, size, site and stage of cyst development, host reaction, and pressure effects of cysts on adjacent tissues. The average diameter of asymptomatic cysts is reportedly about 4 cm, whereas symptomatic cysts average about 10 cm in diameter. Hydatid cysts affect both genders equally over a wide age range. Most hospitalized patients are 21 to 40 years old, and morbidity may peak in 6- to 20-year-old individuals. A single cyst in one organ is present in 40% to 80% of patients with primary cystic echinococcosis. The liver is most frequently involved, followed by the lung, kidney, and spleen, although any organ may be involved including the heart and the CNS. Clinical presentations vary and include abdominal pain, hepatomegaly, cholestasis, biliary cirrhosis, portal hypertension and ascites for liver cysts, and cough, dyspnea, hemoptysis, and pleuritis for lung cysts. In both organs, erosion of cysts into the biliary or bronchial trees can cause obstruction and postobstructive bacterial infections. Cysts can also become infected and form bacterial abscesses. Ruptured cysts may cause severe allergic reactions including anaphylaxis, and they may also lead to the seeding of daughter cysts to other organs, increasing morbidity and mortality.
Echinococcosis is the development of the hydatid cyst from any of the four species of Echinococcus in humans. It usually takes years for cysts to become large enough to cause symptoms.
Prevalence is greatest in sheep- and cattle-raising countries, especially where dogs herd sheep; humans acquire infection by ingesting eggs and are usually dead-end hosts; infections are usually acquired in childhood with a higher incidence among males.
The initial stage of infection following oral ingestion of E. granulosus eggs is asymptomatic, and the infection may remain so for years or even for life.
The development of morbidity is related to several factors including the number, size, site, and stage of cyst development, host reaction, and pressure effects of cysts on adjacent tissues.
The liver is most frequently involved followed by lung, kidney, and spleen, although any organ may be involved including the heart and CNS.
Clinical presentations can be quite varied.
Cyst rupture may cause severe allergic reactions including anaphylaxis and may lead to seeding of daughter cysts to other organs.
Surgery can be successful especially for low numbers of cysts with limited organ involvement not involving vital locations.
Puncture-aspiration-injection-reaspiration (PAIR) is a less invasive technique involving injection of parasiticidal fluids into a cyst, but this method has limitations.
Drug treatment with albendazole or mebendazole is indicated for inoperable cysts and has provided improvement in a majority of patients, but cure in a minority.
The size and location of cysts can also influence the likelihood of success with drug treatment (e.g., bone cysts).
Serial imaging may be used to monitor therapy.
The primary unilocular hydatid cyst of E. granulosus removed from the liver usually ranges from 1 to 7 cm, although occasionally they may be much larger. The cyst is white, spherical, and filled with fluid. Opening the cyst reveals a translucent membrane with numerous brood capsules attached and a surrounding outer thick host-formed fibrous capsule. Primary cysts usually contain multiple daughter cysts that are morphologically identical to the primary cyst.
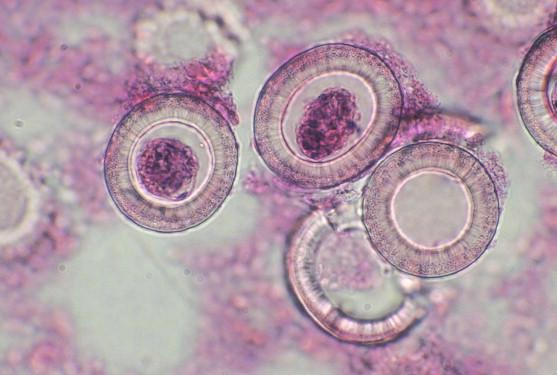
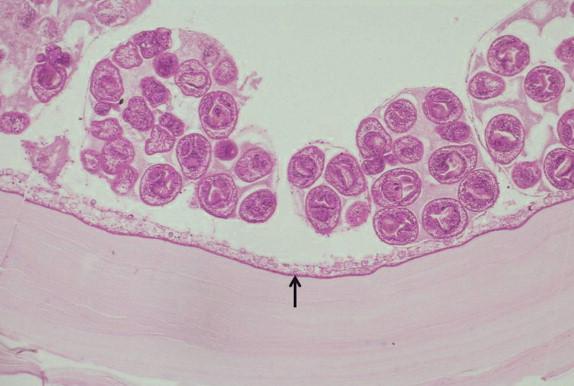
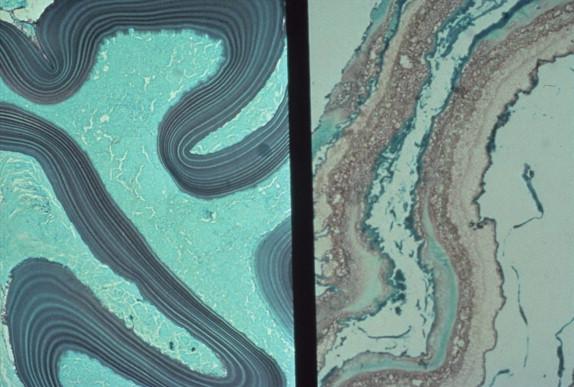
The hydatid cyst wall is composed of two layers: an outer laminated membrane and an inner germinal membrane ( Figure 27-7 ). The laminated membrane is approximately 1-mm thick, and its layering is made more pronounced by use of the Gomori methenamine-silver (GMS) stain ( Figure 27-28 , presented later in the chapter). The germinal membrane is 20 to 25 μm thick and contains nuclei and calcareous corpuscles. In fertile cysts, brood capsules and individual protoscolices arise from the germinal membrane (see Figure 27-7 ). A fertile cyst may contain thousands of brood capsules, and each brood capsule may house a dozen or more protoscolices. Daughter cysts usually form within the primary cyst from the germinal layer, brood capsules, or protoscolices. Brood capsules, protoscolices, hooklets, fragments of germinal membrane, and daughter cysts may be found floating in the cyst fluid. Daughter cysts are morphologically identical to the parent cyst and may have escaped from a damaged parent cyst, developing into exogenous daughter cysts. Some cysts are sterile in that they form no protoscolices, brood capsules, or daughter cysts.
Hydatid cysts grow slowly, taking several years to develop, a time when the patient is usually asymptomatic. During this period the cyst provokes an inflammatory reaction that eventually results in the cyst being surrounded by a thick fibrous capsule. Viable, nonruptured, primary cysts cause damage resulting from compression of adjacent tissues. Dead or ruptured cysts pose serious problems and complications. Fragments of necrotic laminated membrane can cause an acute inflammatory reaction with tissue eosinophilia, granuloma formation with giant cells, and broad areas of necrosis. Dying protoscolices eventually calcify. Sometimes only the birefringent, acid-fast hooklets are preserved in areas of necrosis. Secondary bacterial infection and suppuration may accompany disintegration of cysts.
Radiologic findings (ultrasound, CT, and MRI) can suggest the diagnosis of hydatid cyst. ELISA and Western blot serology (available through the CDC in the United States) can confirm the diagnosis. The sensitivity of serology for liver cysts is higher than that for lung cysts, but a proportion of patients with hydatid cysts in either site do not produce detectable specific serum antibodies. As imaging studies are more sensitive than serology, characteristic imaging studies can still suggest the diagnosis of hydatid cyst even in the presence of negative serology.
Abscesses, neoplasms, and other conditions may enter the differential diagnosis of hydatid cysts of the liver. A variety of other conditions may be differential diagnostic considerations in other sites.
There are several therapeutic approaches for the treatment of cystic hydatid disease. Surgery can be successful, especially when there are low numbers of cysts and there is limited organ involvement not relating to vital locations. Puncture-aspiration-injection-reaspiration (PAIR) is a less invasive technique involving injection of parasiticidal fluids into a cyst, but this approach has limitations, including being contraindicated in lung, heart, and CNS cysts, and in liver cysts communicating with the biliary tree due to the risk of chemical cholangitis. A new technique for which there are few published data is percutaneous thermal ablation. Drug treatment with albendazole or mebendazole is indicated for inoperable cysts, and it has provided improvement in a majority of patients but cure in a minority. Albendazole is better absorbed from the gastrointestinal tract and is the favored medication. The size and location of cysts can also influence the likelihood of success with drug treatment. For example, bone cysts reportedly respond less well than cysts at other sites. Serial imaging may be used to monitor therapy. Surgery can be curative, as can drug therapy in a minority of cases (10% to 30%). Drug therapy has a beneficial effect on cysts in most cases (50% to 70%), but 20% to 30% of patients do not show evidence of improvement. Relapses can also occur after drug therapy, which can usually be retreated.
Morphologic features of hydatid cysts are laminated membrane, germinal membrane, and brood capsules containing protoscolices.
Viable, intact, growing cysts usually cause minimal host response except for fibrous capsule formation.
Dead or degenerating cysts provoke acute and chronic inflammation, eosinophilia, granuloma formation, and eventually calcification.
Less common cestodes include Diphyllobothrium latum , Hymenolepis nana, and H. diminuta proglottids: Taenia multiceps and T. serialis larvae (coenuri). Rare cestodes include proglottids of the following genera: Mesocestoides, Bertiella, Raillietina, and Inermicapsifer .
TREMATODE INFECTIONS
As stated earlier, trematode infections in humans can be divided into two groups: schistosomes (blood flukes) and all the others.
SCHISTOSOMIASIS
Schistosomiasis is probably the most important helminthic infection of humans. It is estimated that more than 200 million people in 77 countries are infected. Although not acquired in the United States, the large immigrant populations from endemic areas migrating to the United States make the histopathologic diagnosis of schistosomiasis an occasional encounter for the U.S. pathologist. Human infection has been reported for 10 different species; however, the majority of infections are caused by three species: Schistosoma mansoni, S. haematobium, and S. japonicum . Schistosomes, regardless of the species, have complex life cycles that include a species-specific freshwater snail as an intermediate host. The geographic distribution is therefore directly related to the availability of the proper intermediate host snail. Humans acquire the infection when they come into contact with fresh water that is contaminated with cercariae. Cercariae penetrate human skin, undergo metamorphosis, migrate, and eventually develop into adult worms that live in the lumens of vessels. Adult male and female worms mate, and females start to lay nonoperculate eggs that can travel by the circulatory system to virtually any organ in the body. The diagnosis of schistosomiasis is usually made by identifying eggs in feces (S. mansoni and S. japonicum) or urine (S. haematobium), as the adult worms inhabit the portal venous system and urinary bladder venous plexus, respectively. Schistosome eggs are probably the most common helminth eggs encountered by the pathologist in biopsy or autopsy specimens. The host response to eggs is the most important histopathologic change. Rarely are adult flukes observed in tissue sections.
Schistosomiasis may present as a dermatitis (schistosome dermatitis or cercarial dermatitis) associated with skin penetration by cercariae, acute schistosomiasis (Katayama fever), or chronic schistosomiasis. Schistosome dermatitis is caused by skin penetration by cercariae, and it initially presents with a prickling sensation followed by a macular rash several hours later. In previously sensitized individuals it may develop into a pruritic maculopapular rash lasting several days.
Acute schistosomiasis (Katayama fever) occurs in previously uninfected individuals 2 to 8 weeks after infection with S. japonicum and S. mansoni in particular. There is an acute onset of fever, chills, headache, myalgia, abdominal pain, diarrhea, and occasionally bloody stools. A majority of patients also develop respiratory symptoms and interstitial infiltrates in chest radiographs. Hepatosplenomegaly and lymphadenopathy are common, and eosinophilia is usually present. Eggs may not, however, be detected in feces until later in the course of disease. The illness usually resolves in a few weeks, but the course may be complicated by lesions at the sites of ectopic egg deposition such as the CNS. Heavy infection may result in death.
In chronic schistosomiasis with light or moderate infections, symptoms may be mild or absent, but there is often eosinophilia. Moderate to heavy infections can lead to morbidity associated with anemia and malnutrition, particularly in children and pregnant women. Patients with heavy S. mansoni infection can present with fatigue and abdominal pain with intermittent diarrhea or dysentery. Intestinal strictures and large inflammatory masses may mimic neoplasms. Some patients present with hepatomegaly, and after years of infection about 5% to 10% develop periportal fibrosis (Symmers’ “pipestem” fibrosis). Portal hypertension may develop, leading to esophageal varices. Coexisting liver disease such as alcoholic cirrhosis and chronic hepatitis B and C may lead to jaundice and ascites. Patients with hepatitis B and S. mansoni infections have a higher risk for the development of hepatoma than patients with hepatitis B infection alone.
Eggs may cause pulmonary lesions by traveling through portosystemic collateral vessels, bypassing the liver. These can cause granulomatous pulmonary arteritis that can progress to cor pulmonale. The CNS is rarely involved by S. mansoni (usually spinal cord or cauda equina) and even less commonly by S. haematobium , but it may be involved in up to 5% of S. japonicum infections.
Adult S. mansoni are flukes in which the sexes are separate and the female worm is usually found in the gynecophoral canal of the male.
Adult S. mansoni live in the veins of the portal system where the female worm deposits 100 to 300 eggs per day.
Humans acquire S. mansoni infection when cercariae penetrate the skin.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here