Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
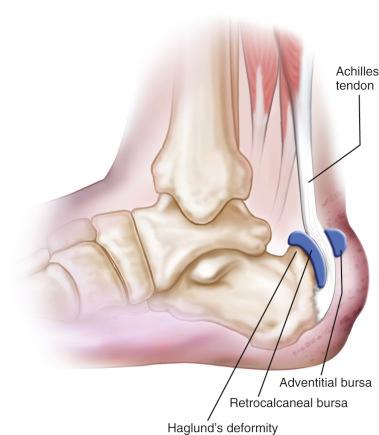
Pain in the posterior, superior portion of the calcaneus may be multifactorial, ranging from retrocalcaneal bursitis, enlargement of the superior bursal prominence of the calcaneus, insertional Achilles tendinosis, to inflammation of an adventitious bursa between the Achilles tendon and the skin ( Fig. 120.1 ). Each of these entities may exist as an isolated condition or may be part of a symptom complex. Careful analysis of the patient's subjective complaints and objective findings are required to arrive at the correct diagnosis. Disorders of the Achilles tendon are covered in Chapter 118 and are not reviewed in detail here.
Retrocalcaneal bursitis may occur as an isolated entity but is more commonly associated with the prominent posterior superior bursal portion of the calcaneus, or Haglund deformity. When Achilles tendinosis occurs concomitantly with this condition, it is generally located in the area of the Achilles tendon just at or above the insertion of the Achilles tendon at the posterior portion of the os calcis. Retrocalcaneal pain syndrome is commonly associated with a high-arched cavus foot and a varus heel. The combination of these factors tends to produce a foot that does not dorsiflex as readily as a normal foot. The heel is prominent and is more susceptible to increased pressure from the tendons and the counter of the shoe.
The history is generally that of slow onset of dull aching pain in the retrocalcaneal area aggravated by activity and certain footwear. Footwear with a narrow heel counter is most commonly associated with this condition. Pain that starts after sitting or when arising from bed in the morning is commonly reported. At times, the patient may have a history of the acute onset of pain, which is sometimes associated with a traumatic incident. When this history is reported, a rupture of the Achilles tendon or disruption of calcific tendinosis must be considered.
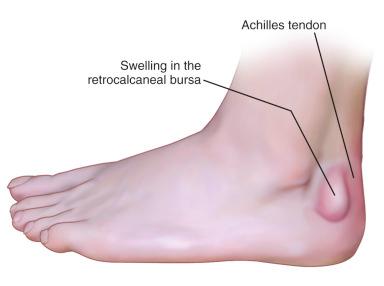
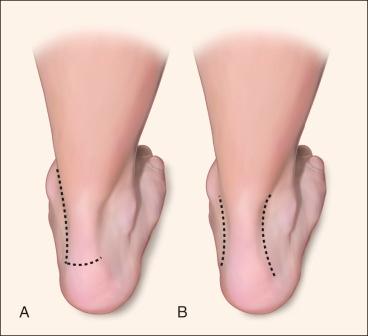
Physical examination reveals swelling in the area of the retrocalcaneal bursa between the Achilles tendon and the calcaneus. A prominence is generally present in the area of the superior portion of the heel. The swelling in the retrocalcaneal bursa will be found just anterior to the Achilles tendon. By palpating medially and laterally at the same time, and with the aid of ballottement, one can sometimes feel fluid within the bursa ( Fig. 120.2 ). With careful and discrete palpation, one can generally differentiate between swelling in the Achilles tendon and swelling in the retrocalcaneal bursa. The swelling of the Achilles tendon associated with retrocalcaneal bursitis is usually at the level of the tendon at or just proximal to the insertion. Dorsiflexion of the foot usually increases the pain in the area. A great deal of swelling and inflammation on examination may indicate involvement of both the retrocalcaneal bursa and the Achilles tendon. Redness and swelling may be present between the Achilles tendon and the skin, usually as a result of an adventitious bursitis produced by pressure of the shoe counter against the Achilles tendon. Periostitis may be present, which is a discrete localized area of tenderness of the os calcis, usually on the lateral side of the posterior portion of the os calcis and produced by pressure of the shoe counter. A “squeeze test,” in which the palms of both hands apply moderate compression to the tuberosity, should be performed to rule out the presence of a stress fracture. If the patient reports pain with this examination, a high suspicion for a stress fracture should be noted.
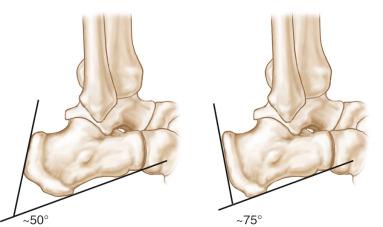
A lateral view of the foot is taken with the patient standing, which allows biomechanical evaluation of the foot and evaluation of the specific points of the os calcis. The points of the os calcis are identified as the posterior margin of the posterior facet, the superior bursal projection, the tuberosity indicating the site of the Achilles tendon insertion, the medial tubercle, and the anterior tubercle. The shape and appearance of the superior bursal prominence are noted. Evaluation of the lateral radiograph may be performed using the method described by Fowler and Philip, which measures the posterior calcaneal angle ( Fig. 120.3 ). Fowler and Philip consider the bursal projection prominent if the angle is greater than 75 degrees. Some authors have concluded that a combination of the Fowler angle and the angle of calcaneal inclination is more effective in correlating the radiographic appearance with symptomatology than the Fowler and Philip angle alone, with the combined angle being greater than 90 degrees in patients with symptomatic Haglund disease.
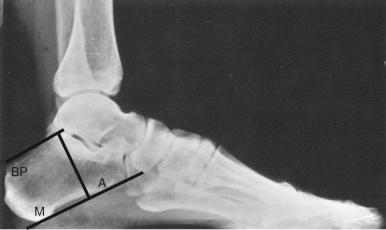
Parallel pitch lines have been used by Heneghan and Pavlov to determine the prominence of the bursal projection ( Fig. 120.4 ). The base line is constructed by placing a line along the medial tuberosity and the anterior tubercle, and a parallel line from the posterior lip of the talar articular facet. The bursal prominence is considered abnormal if it extends above this line.
Magnetic resonance imaging (MRI) has provided clearer insight into the anatomic abnormalities associated with posterior heel pain. The imaging allows visualization of the Achilles tendon and the bursa, as well as demonstrating any bony abnormalities in the posterior superior calcaneus. In patients with a suspected stress fracture of the calcaneus, an MRI scan can be ordered to delineate the diagnosis in an expeditious manner so that the most appropriate treatment may be initiated. In patients refractory to nonoperative treatment, a preoperative MRI will define which anatomic structures need to be addressed ( Fig. 120.5 ). The degree of tendinosis present in the Achilles tendon is easily visualized and distinguished from isolated bursitis.

Nonoperative treatment is successful at alleviating posterior heel pain regardless of cause in most patients. Adventitious bursitis is generally treated conservatively by softening the heel counter with use of a small U-shaped pad to relieve the pressure of the shoe or counter against the inflamed area; in addition, anti-inflammatory medications are used. Surgical intervention performed solely for adventitious bursitis is unusual and carries a risk of wound slough, and thus it should be avoided if possible.
Retrocalcaneal bursitis and Haglund deformity are generally managed by conservative measures consisting of antiinflammatory medication, decreased activity, padding to prevent pressure on the affected area, orthoses or heel lifts, and strengthening and stretching exercises. If the condition does not respond to these modalities, then surgical intervention may be considered. Surgery generally consists of excision of the exostosis and the retrocalcaneal bursa and, at times, the adventitious bursa, if present, along with correction of the Achilles tendon disease with tendon transfer if necessary. Although good results after surgery are reported in most series, in the athlete, this condition may present a serious threat to continued full activity, even after surgical intervention.
Initial goals of the treatment of patients with retrocalcaneal bursitis are to control pain and attempt to allow the patient to return to normal function and activity. Rest, particularly soon after the onset of symptoms, can be helpful. The duration of rest may be prolonged, depending on the increasing duration of symptoms. Cross-training with low-impact exercises, such as an elliptical machine, swimming, or biking, may prevent deconditioning in the athlete. Modified regimens may be suggested for an athlete who is unwilling to cross-train. In patients with exquisite tenderness, immobilization in a controlled ankle motion (CAM) boot or short-leg walking cast may be helpful. Immobilization should be used cautiously in athletes, because patients can have resultant tendon and muscle atrophy, degeneration, and decreased blood supply.
Nonsteroidal drugs that are administered orally or delivered locally in the form of a patch may decrease local inflammation. Cryotherapy and ice can decrease pain, swelling, and inflammation as well. Corticosteroids that are taken orally, injected locally, or applied topically have been used. Injections must be used cautiously because they can lead to a higher incidence of tendon ruptures and tendinopathy. Animal model studies with intratendinous injections have been shown to result in localized tendon necrosis and decreased mechanical strength. If used, the steroid injection must be placed anterior to the tendon, in the area of the retrocalcaneal bursa. The patient is immobilized in a CAM walker for 3 to 4 weeks to minimize the risk of tendon rupture after injection into the retrocalcaneal bursa.
Orthoses may help these patients by providing a heel lift function, correcting hyperpronation, or minimizing leg length discrepancies. Care must be exercised when correcting hindfoot pronation deformities, because overcorrection can result in inflexibility of the hindfoot with decreased shock absorption. Heel cups can decrease the strain on an Achilles tendon and elevate a prominent superior calcaneal tuberosity away from the tendon. High heels, clogs, open-back shoes, gel braces, and horseshoe pads can also provide symptomatic relief for the patient.
If retrocalcaneal bursitis is present with a normal Achilles tendon, conservative therapy is implemented until the patient has been asymptomatic for 4 to 6 weeks. The patient may then return to sports participation starting with limited activity and working up to full activity within 4 to 12 weeks, assuming that they have recovered full strength and mobility without pain. If retrocalcaneal bursitis is associated with degeneration of the Achilles tendon, nonoperative treatment should be used until the patient is asymptomatic; a gradual increase in activity is then allowed over a 6- to 12-week period.
If the patient does not respond to these modalities, then surgical intervention may be considered. Surgery generally consists of excision of the exostosis, the retrocalcaneal bursa, and at times the adventitious bursa, if present, along with correction of the Achilles tendon disease with tendon transfer if necessary. Although most authors report good results after surgery, in the athlete this condition may present a serious threat to continued full activity, even after surgical intervention.
Surgical procedures are usually performed for retrocalcaneal bursitis associated with the superior bony prominence. The retrocalcaneal bursa and the superior bursal prominence are excised. The adventitious bursa is excised if it is prominent. If the adventitious bursa is excised, the surgeon must take care to excise it carefully and meticulously to avoid adversely affecting the blood supply or the skin overlying this area, because a skin slough can result in significant morbidity for the patient.
A medial or lateral incision, or a combination of incisions 1.5 cm anterior to the Achilles tendon, is made as determined by the location and width of the bony prominence ( Fig. 120.6 ). Alternatively, a central posterior Achilles splitting approach can be used. Prone positioning can be used with all of the aforementioned incisions. A medial incision may be carried out with the patient supine and minimizes the risk of damage to the sural nerve, but the superior calcaneal exostosis is typically lateral, which may make excision slightly more difficult. Given the elimination of sural nerve injury and simplified positioning, this is the author's preferred technique in these cases. If the patient has concomitant tendinosis of the Achilles tendon, the central posterior tendon splitting approach is used.
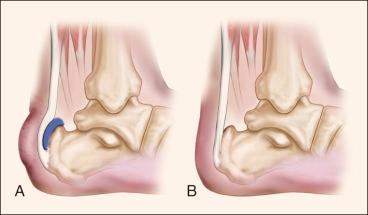
After incision of the central aspect of the posterior skin, the incision is carried directly to the level of the paratenon, and dissection is performed at this level to maintain full-thickness skin flaps to avoid skin loss. Attention should be given to the calcaneal branch of the sural nerve on the lateral side and the medial calcaneal nerve on the medial side. The Achilles tendon is inspected to confirm the presence and degree of tendinosis. Regardless of the surgical approach, the retrocalcaneal bursa is now excised. An exostosectomy is performed, removing the bone from the area of insertion of the Achilles tendon to the superior portion of the posterior facet of the os calcis ( Fig. 120.7 ). Adequate bone is removed, and the edges are smoothed with a rasp. If greater than 50% of the insertion of the Achilles tendon is elevated from the calcaneus, repair with suture anchors is recommended to avoid rupture. In the case of a concomitant tendinosis, a flexor hallucis longus transfer may be required if a significant portion (>50%) of the Achilles tendon is excised as described in Chapter 118 . The split in the Achilles tendon is repaired with an absorbable monofilament number 0 suture. The subcutaneous tissue and skin are closed after the procedure. Compressive dressings and plaster splints are applied to maintain 15 degrees of ankle plantar flexion to maximize perfusion to the posterior skin.
In cases in which the Achilles tendon is not involved, the patient is seen at 2 weeks for stitch removal, the lower extremity is placed into a removable CAM walker with the ankle at neutral position for an additional 4 weeks, and weight bearing is begun. A rehabilitation program for non-weight-bearing strengthening and range of motion (ROM) is begun at this initial visit. Six weeks after surgery, the walking boot is removed and the patient is allowed to weight bear with a ![]() -inch heel lift during this time for 4 to 6 weeks. Therapy is continued and graduated to weight-bearing exercises. Patients are then advanced to regular footwear and continue to follow a strengthening program at home with a Theraband. Athletic activity is restricted for 3 months after surgery.
-inch heel lift during this time for 4 to 6 weeks. Therapy is continued and graduated to weight-bearing exercises. Patients are then advanced to regular footwear and continue to follow a strengthening program at home with a Theraband. Athletic activity is restricted for 3 months after surgery.
If surgery has been performed on the tendon in combination with excision of the retrocalcaneal bursa and exostosectomy, immobilization is continued for 8 weeks, but active (ROM) is begun at 3 weeks. Strengthening and stretching exercises are started at 6 to 9 weeks. Increased activity according to tolerance can be started at 12 weeks, and return to strenuous activity is allowed at 4 to 6 months if local symptoms have resolved.
Ippolito and Ricciardi-Pollini described three patients with invasive retrocalcaneal bursitis who had a large bursa and invasion of the os calcis. Pathologic examination revealed lymphoplasma cellular infiltrates containing proportionately more plasma cells than lymphocytes. Removal of the bursa provided clinical relief, and systemic rheumatic disease did not develop in later years.
Keck and Kelly reported on 13 patients with 20 symptomatic heels that were treated surgically. In 17 heels, the superior bursa was excised, and in three heels a dorsally based closing wedge osteotomy was performed. Good results were reported for 15 of the heels treated. The initial results were good in all but two patients, whose pain recurred as a manifestation of generalized rheumatoid arthritis. An osteotomy was used to reduce the posterior prominence, and results were rated good in two heels—fair in one heel, and poor in two heels. The authors believed that too few osteotomies were performed in this series to evaluate this method. A disadvantage of the osteotomy was that a longer convalescence was required.
A series of 65 patients with Haglund disease was reported by Ruch ; 17 underwent resection of the posterior superior portion of the os calcis, with resection of the posterior superior aspect both medially and laterally and removal of sufficient bone to render the previous palpable prominence entirely absent. The patients were evaluated 6 months to 5 years after undergoing surgery. Fifteen demonstrated good to excellent results with elimination of symptoms. Three of the patients required a second procedure to obtain the desired result.
Schepsis and Leach reported that the majority of athletes, particularly runners, who presented with acute or chronic posterior heel pain were successfully managed nonoperatively using a combination of (1) a decrease in or cessation of the usual weekly mileage, (2) temporary termination of interval training and workouts on hills, (3) a change from a harder bank surface to a softer surface, (4) a 0.25- to 0.50-inch lift inside the shoe or added to the shoe, and (5) a program designed to stretch and strengthen the gastrocnemius-soleus complex. These measures were combined with use of oral anti-inflammatory medications and an occasional injection of corticosteroid into the retrocalcaneal bursa. Postural abnormalities were treated with orthotics. The authors retrospectively studied 45 cases of chronic posterior heel pain that were treated surgically in 37 patients. All but two of these patients were competitive long-distance runners who ran an average of 40 to 120 miles per week prior to the onset of symptoms. Their ages ranged from 19 to 56 years.
The surgical approach used by Schepsis and Leach was a longitudinal incision 1 cm medial to the Achilles tendon that was continued transversely to form a J-shaped incision if necessary. A cast was applied and worn for 2 to 3 weeks, with weight bearing permitted after 1 week. When disease within the tendon required excision and repair, immobilization was continued for 1 to 2 weeks longer. (ROM) exercises were emphasized. A graduated program of swimming and stationary bicycling combined with isometric, isotonic, and isokinetic strengthening of the calf muscles was prescribed. Jogging was permitted after 8 to 12 weeks, but rarely sooner. Full return to a competitive level of sports activity usually required 5 to 6 months.
The patients were divided into three groups—those with Achilles tenosynovitis-tendinitis, those with retrocalcaneal bursitis, and those with a combination of both. In the 14 patients with retrocalcaneal bursitis, seven (50%) had excellent results, three (21%) had good results, and four (29%) had fair results. In the group with a combination of both conditions, five (71%) had excellent results and two (29%) had good results. It was noted that four of the six unsatisfactory results occurred in the group with retrocalcaneal bursitis.
More than half of all reported complications involve the surgical wound. Skin edge necrosis, superficial or deep infection, and seroma or hematoma formation are the most common complications. These complications can be minimized with postoperative splinting in 20 degrees of plantar flexion. Sural neuritis, tendon rupture, or disruption of the repair and deep vein thrombosis have also been reported. Failure to achieve complete relief of symptoms has been reported in up to 29% of patients with retrocalcaneal bursitis. Given the high demands of the athletic population, appropriate counseling regarding the outcomes is critical prior to performing surgery.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here