Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Hand fractures are common injuries and have been reported to account for 10% of upper-extremity fractures. Timely diagnosis and treatment are essential to provide a good outcome. Although many hand fractures can be managed without surgery, recognition of those requiring surgery is essential. Operative treatment is aimed to provide functional stabilization of the fracture followed by appropriately timed rehabilitation. Occasionally, secondary procedures such as capsulotomy or tenolysis may be required to restore motion. The techniques described in this chapter can be used throughout the world.
Hand and finger fractures are exceedingly common, accounting for approximately 10% of all fractures with an incidence of roughly 225 fractures per 100,000 people per year. The task of diagnosing and treating hand fractures falls on multiple different specialties across the spectrum of medicine, from primary care and emergency room physicians, to hand surgeons and therapists. The goal of treatment is to improve or prevent deformity and to restore and optimize motion and function. Nonoperative treatment is often successful, but multiple factors may necessitate surgical intervention. This decision is contingent upon fracture displacement, angulation, inherent stability, chronicity of presentation, and other associated injuries as well as patient occupation and health comorbidities. Regardless of the method of intervention, successful treatment relies on reduction and stabilization of the fracture and initiation of rehabilitation.
The goals of fracture stabilization in the hand are to provide a stable construct to allow for fracture healing while maintaining motion. The unique anatomy of the hand, however, creates differences in treatment compared with common techniques used in long bones. Absolute, rigid stability across fracture fragments is not necessary, and the soft tissue envelope overlying bones in the hand does not allow for stout coverage of thick plates and screws. In addition, irritation of the tendons can occur even with smaller, low-profile plates, especially in the phalanges, and result in adhesions and stiffness. The aim of treatment is to provide functionally stable fixation and to minimize soft tissue disruption. Therefore closed reduction and fixation with Kirschner wires (K-wires) is often utilized in the fingers and commonly used in the hand. Fracture geometry may preclude the use of K-wires, necessitating alternative procedures, such as lag or positional screws, plate and screw constructs, or external fixation.
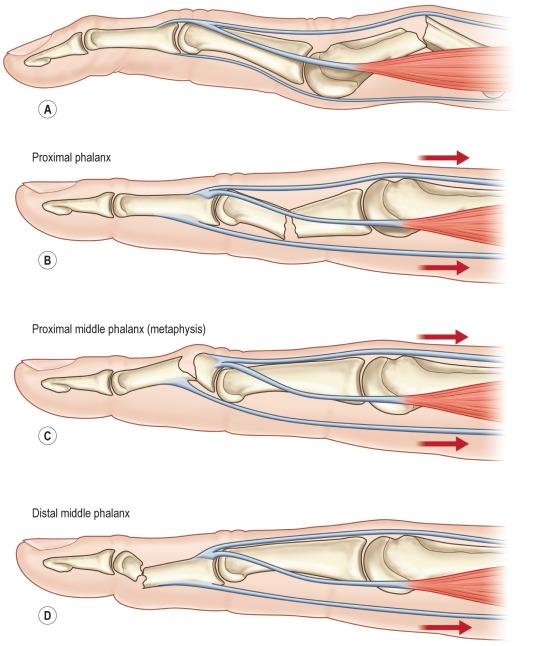
A thorough understanding of the anatomy of the hand is critical to successful treatment of hand fractures. There are distinct differences between treating hand fractures due to the distinctive anatomy and proximity of tendons. In addition to the difficulties of having minimal soft tissue coverage and the need for tendon gliding, multiple other anatomical considerations must be understood to properly treat hand fractures. First, the multiple tendinous insertions throughout the fingers create complex deforming force vectors depending on the location of the fracture. For instance, metacarpal shaft fractures typically have an apex dorsal angulation, whereas proximal phalanx shaft fractures have an apex volar configuration; both of these deformities result from the fracture location in relation to the interosseus muscular insertions. Similarly, fractures in the proximal extent of the middle phalanx often have a flexion deformity (apex dorsal angulation), whereas those fractures located in the distal aspect of the middle phalanx have a tendency to fall into extension (apex volar angulation). Again, this difference in fracture orientation is due to a deforming force, with the pull flexor digitorum superficialis (FDS) being either proximal or distal to the fracture site. These substantial deforming forces must be overcome to attain an acceptable reduction, or at least counteracted with well-molded immobilization devices to prevent later displacement ( Fig. 5.7.1 ).
The initial step in managing a hand fracture is making the diagnosis and understanding the inherent stability, or lack thereof, that each individual fracture possesses. History should include hand dominance, mechanism of injury, and patient vocations and avocations because these are critical to developing the best treatment plan. Observation of the hand in a resting position allows visualization of the digital cascade and any gross malalignment. In addition, edema and ecchymosis can identify areas requiring further evaluation. Asking the patient to flex and extend the digits should result in all fingers pointing to the scaphoid tubercle with full flexion. Any rotation or scissoring is noted. Flexion and pronation of the thumb should allow opposition to the small finger. Gentle palpation of the injured area is performed, noting tenderness. In the event that the patient cannot flex the fingers secondary to pain, use of tenodesis by flexing and extending the wrist will allow finger motion and may demonstrate rotation of the digit.
Once a history and physical have been performed, plain radiographs are obtained to determine exact fracture location and displacement. Multiple views, including posteroanterior (PA), lateral, and oblique, will allow full visualization of the characteristics of a fracture. Evaluation should be focused on the injured digit. Radiographs of the hand can be used as screening and are often adequate for finger metacarpal fractures, but evaluation of conditions in the phalanges requires imaging of the injured finger, as this will focus the beam in the most advantageous position to evaluate the fracture. The thumb requires special consideration because its normal position is out of the plane of the hand. For example, it is much easier to visualize an intraarticular 1st metacarpal base fracture (Bennett or Rolando fracture) on a true anteroposterior (AP) view of the thumb (Roberts view) and a true lateral (Bett's view). Often, appropriate plain radiographs are sufficient for a complete understanding of a fracture's character and stability; no further imaging is routinely required.
The final step in diagnosis is to coalesce all information from the patient's history, physical, and imaging to determine a fracture's need for reduction and subsequent stabilization. For instance, transverse metacarpal fractures with minimal displacement and angulation and no malrotation often are sufficiently stable fractures to treat nonoperatively in a cast/splint due to the stabilizing transverse intermetacarpal ligament. Thus not only is an accurate diagnosis required when evaluating hand fractures but also is an understanding of the deforming forces present on fracture fragments and the resulting risks of displacement if nonoperative treatment is pursued.
Fractures can be classified according to the location, geometry, and displacement to determine the stability. Intraarticular fractures tolerate minimal displacement, whereas fractures in the neck or shaft can tolerate some displacement. Extraarticular fractures can be transverse or oblique, and simple or comminuted. Transverse fractures result in angulation but not often rotation, whereas oblique fractures are more likely to result in shortening and rotation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here