Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Deep burns to the hands are significant injuries that result in scarring, contractures, and functional limitations. These post-burn contractures are common in pediatric and adult patients despite appropriate initial management. The most common contractures include the first and interdigital web spaces, and flexion or extension contractures. Pre-operative management includes a complete hand examination focusing on skin quality, previous skin grafts, web spaces, and joint range of motion. Planning a reconstructive operation should focus on improving both the functional limitation and the esthetic appearance of the hand. The fundamentals of hand burn reconstruction include contracture release with scar excision, followed by local soft tissue rearrangement or skin grafting. The size of the wound after contracture release should not be underestimated, and procedures may be staged if necessary. Post-operative care includes pain control, wound care, splinting, and aggressive hand therapy. Management of complications such as bleeding, nerve injury, and wound care issues is discussed. Finally, recurrent contractures may require reoperation to achieve satisfactory function.
The outreached hand is frequently burned, resulting in significant functional limitations. This is especially common in the developing world, where open cooking flames and manual work are realities of daily life. The principles of acute burn care management are essential to optimize functional outcomes of the hand. These include hand elevation, aggressive and frequent burn wound care, early tangential excision with skin grafting when appropriate, strict adherence to splinting (position of safety or intrinsic-plus), and early motion. Sheet (non-meshed) split-thickness grafting on the hand dorsum may provide coverage with a more esthetic result. Additionally, deep burns of the hand dorsum with small areas of exposed extensor tendons may initially be covered with a variety of dressings to allow the underlying tissue to granulate, and ultimately may require skin grafting. In the subacute period, the use of supervised motion (hand therapy), compressive dressings, and scar management, including massage and silicone sheet compression, becomes important.
Despite appropriate initial management, post-burn contractures of the hand are common in pediatric and adult patients. These post-burn deformities result from the initial burn injury and subsequent soft tissue deficit. Contractures frequently result from deep burns healing by secondary intention or the eventual contracture of split-thickness skin grafts. The most common contractures of the hand include the web spaces, and flexion or extension contractures of the hand and digits. Other sequelae of burn injury include hypertrophic scarring, nail deformities, boutonniere deformities, and digital amputation. On presentation, these patients may have been living with hand burn deformities for several years. These functional limitations may cause significant economic hardship if patients cannot work and/or care for themselves.
A classification of post-burn hand deformities has been previously described by Achauer :
Claw deformity
Complete
Incomplete
Palmar contracture
Web space deformity
Web space deformity
Adduction contracture
Syndactylism
Hypertrophic scar and contracture bands
Amputation deformity
Nail bed deformity
In this chapter, the diagnosis of hand burn contractures and reconstructive operative management will be reviewed.
The mechanism of the initial hand burn injury is important to clarify. Pediatric patients often touch a hot object or submerge the hand in a hot substance, resulting in post-burn flexion contractures. As in all pediatric injuries, the overall safety of the child in the home environment should be assessed.
A complete hand examination is the most important pre-operative testing needed. With deep burns of the hand, the affected areas, depending on whether they are palmar or dorsal, have different issues. The palmar aspect has thicker glabrous skin, subcutaneous tissue, palmar fascia, and fibrous septa. This thick tissue protects the underlying flexor tendons. However, the dorsal skin is thin and pliable, with the extensor mechanism just deep to the subcutaneous tissue. Therefore the dorsal skin is more susceptible to contractures.
A complete hand examination should be performed, including:
A complete neurovascular examination.
Examination of the quality and pliability of the overlying skin on both the palmar and dorsal aspects, with identification of previous skin grafted areas.
Determination and documentation of both passive and active range of motion of each digit.
Assessment of the interdigital web spaces for post-burn syndactyly, which affects the normal 45-degree dorsal slope of the web space.
Examination of the thumb in full range of motion in abduction and opposition, including the first web space to determine the degree of skin pliability.
Examination of the entire upper extremity to determine the need for a more proximal contracture release, which likely should be considered a priority for operative intervention.
Radiographs of the hand and wrist to identify underlying bone and joint deformities; in long-standing burn contractures, some joints may be dislocated or even fused.
Ideally, a patient should be at least 12 months post-burn to allow full scar maturation before operative intervention. At least 2 to 3 months of hand therapy, with a plateau in progress and a continued functionally limiting contracture, is a prerequisite for operative management. Attention should be paid primarily to improving the functional limitation, while the esthetic appearance of the hand is also taken into consideration. The patient and family should be counseled that multiple operations may be required to achieve an improved outcome.
Hand burn reconstruction begins first with scar excision and release of the contracture, followed by local soft tissue rearrangement and/or skin grafting. The size of the wound after contracture release should not be underestimated. Staged procedures may be required when releasing significant contractures of the hand.
Scar excision is performed for web space contractures and post-burn syndactyly of the second through fourth web spaces. Interdigital web space contractures may extend to the middle of the proximal phalanx. Releasing incisions are performed to incorporate planned local flaps or Z-plasties. Flaps are designed to cover areas where skin grafts will not take, including exposed tendons or joints. Dorsally based skin flaps are ideal to reconstruct the web space in larger defects. After scar excision, the pliable tissue is recruited into the defect.
Tendons are exposed with care, keeping the paratenon intact to allow skin grafting over these areas. The underlying nerves and arteries are protected given their significant risk of direct injury during scar excision and from stretching after release.
The skin and underlying scar are excised over the joint. Restricted joint capsules and/or ligaments necessitate concurrent capsulotomies to achieve improved range of motion. Deep dorsal or palmar burns may result in direct injury or scar adhesions to the underlying extensor or flexor tendons. Tenolysis is performed as needed; however, exposed tendons may require flap coverage. Kirschner (K) wires are utilized to maintain finger position after release of severe contractures, given the difficulty with splinting these deformities.
Full-thickness skin grafts are the mainstay for coverage after burn contracture release, given that less secondary contracture occurs post-operatively compared with split-thickness skin grafts.
Full-thickness skin grafts are harvested from the forearm or the groin, and hair-bearing regions are avoided. Donor sites are closed primarily.
Absorbable sutures (such as chromic or plain gut, 4-0 or 5-0 size) are used for suture of skin grafts and closure of donor sites.
Skin grafts are pie-crusted to allow fluid and blood to adequately drain.
A tie-over bolster for compression of the skin graft is placed on the recipient wound bed with a nonadherent dressing over the skin graft.
These patients are followed up on day 5 for takedown of the splint and bolster.
The Z-plasty is an effective technique in hand burn reconstruction for elongating contracted skin ( Fig. 4.8.1 ). A Z-plasty is performed with the interposition of two triangular flaps from immediately adjacent areas with maximum elongation. The central limb is designed parallel and directly over a burn contracture scar. This orientation allows for the transposition of the Z-plasty flaps to result in a gain in length. A standard Z-plasty has angles of 60 degrees with a theoretical gain in length of 75%. A single Z-plasty or multiple Z-plasties are commonly utilized in the web space contractures. Four- and five-flap Z-plasties are also utilized for web space deepening.
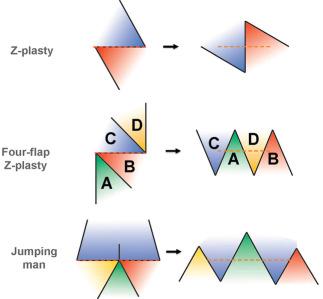
The four-flap Z-plasty is designed with 90-degree angles that are bisected to create 45-degree angle flaps, which are transposed to gain length.
The flaps are marked A, B, C, D. After transposition, the flaps should read C, A, D, B (“Cadbury”).
Absorbable sutures are used for closure (4-0 or 5-0).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here