Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Fetal hydrops is defined as the accumulation of fluid in two fetal compartments (abdominal ascites, pleural effusion, pericardial effusion, skin or scalp oedema). It may also be associated with polyhydramnios and placental oedema.
Immune hydrops is the result of alloimmunisation to red blood cell antigens.
Rhesus (Rh) immunoglobulin has decreased the relative frequency of RhD disease.
Kell alloimmunisation is associated with the least predictable and most severe degree of fetal anaemia.
Doppler measurement of fetal middle cerebral artery peak velocity has transformed the diagnosis and treatment of fetal anaemia and greatly reduced the use of invasive procedures.
Intravascular fetal blood transfusions in cases of severe anaemia and hydrops have dramatically improved the outcome of these pregnancies.
The history of haemolytic disease of the fetus and newborn (HDFN) is an example of how modern medicine can both treat and prevent a disease process with significant perinatal morbidity and mortality. In the 1950s 15% of all alloimmunised gestations ended in stillbirth. Work by Bevis and Walker in Rh-sensitised pregnancies correlated amniotic fluid levels of bilirubin with the incidence of postnatal kernicterus and the severity of anaemia in affected infants. William Liley in New Zealand furthered this work and created the Liley curve, a chart that was able to predict the severity of fetal haemolytic disease and aid in determining the appropriate time for labour induction in affected gestations. Liley’s work decreased the perinatal mortality rate in Rh-sensitised gestations at the National Women’s Hospital in Auckland from 22% in 1958 to 8.7% in 1962.
To improve outcomes for the most severely affected fetuses, Liley further developed the concept of intraperitoneal fetal transfusion. In patients with suspected severe haemolytic disease who were not likely to survive, compatible red blood cells (RBCs) were injected intraperitoneally in the early third trimester. The initial procedures were done by first injecting radiopaque dye into the amniotic cavity of affected pregnancies. X-ray still images were then used to localise the fetal abdomen using the radiopaque dye that had been swallowed by the fetus. Finally, proper placement of the needle in the peritoneal cavity was confirmed by injection of additional radiopaque dye. The first transfusion with fetal survival was reported by Liley and his colleagues in 1962, and by 1965, Liley reported on a further 16 transfused fetuses with a 38% survival rate.
Today, serial intrauterine transfusions (IUTs) to treat severe HDFN in association with maternal RBC alloimmunisation result in neonatal survival in well over 90% of cases. Advancements in ultrasound and IUT technique have certainly played a role in this improvement, but the prevention of Rhesus alloimmunisation by the introduction of Rhesus immunoglobulin (RhIG) has also decreased the disease burden of RhD disease in particular.
The adoption of antenatal and postpartum RhIG has resulted in a marked reduction in the incidence of disease secondary to alloimmunisation by the Rh(D) antigen. Cases of RhD alloimmunisation still occur, however, either secondary to the failure to administer RhIG or secondary to inadequate dosing of RhIG in the presence of an undetected large fetomaternal haemorrhage. Even with the perfect implementation of RhIG, alloimmunisation resulting from incompatibility to the other Rhesus antigens and the non-Rhesus antigens will continue. For example, in east Asia, there is a lower proportion of Rh(D)-negative individuals, leading to a higher relative frequency of non–Rh(D)-related HDFN.
By 30 days of gestation, fetal RBCs express antigens, half of which are paternally derived and may be foreign to the maternal immune system. The transfer of RBCs across the fetal–maternal interface that occurs with spontaneous fetomaternal haemorrhage has been demonstrated to occur in almost all gestations with increasing frequency and volume as the pregnancy progresses. Although fetomaternal haemorrhage before or during birth is thought to be the primary factor in causing maternal alloimmunisation, a complete list of potential precipitating events is listed in Table 40.1 . The exposure of the maternal immune system to the foreign paternal antigen on the fetal RBCs is the impetus for the initiation of the HDFN process.
| Unprovoked | Provoked |
|---|---|
| Idiopathic-spontaneous | Termination of pregnancy |
| Delivery | Amniocentesis |
| Spontaneous abortion | Chorionic villus sampling |
| Ectopic pregnancy | Cordocentesis |
| Abruption | External cephalic version |
| Antepartum haemorrhage | Fetal intervention: fetoscopy, shunt, drainage |
| Trauma | |
| Manual removal of placenta |
The maternal response to RBC foreign antigens is well documented. Cells of the innate immune system identify and destroy foreign cells and present the antigens to the humoural immune system, where specialised cells, specifically B lymphocytes, can recognise the antigen in future encounters and respond rapidly with the production of IgG antibodies. The initial development of immunoglobulin (Ig) G antibodies is a slow process, and it can take anywhere from 5 to 15 weeks for a human antiglobulin titre to be detected after a sensitising event. With few exceptions, the maternal response to the paternal antigen is not sufficient to have a significant effect on the fetus in the sensitising pregnancy. Exposure in a subsequent gestation when the precipitating antigen is present will trigger the rapid production of IgG antibodies. These IgG antibodies freely cross the placenta and bind to fetal RBCs with the offending antigen. These sensitised cells are then sequestered by the fetal spleen and destroyed by macrophages, resulting in fetal anaemia.
The maternal response to paternal antigens on fetal RBCs that have crossed the fetomaternal barrier is variable. Studies in Rh(D)-negative men have demonstrated that some individuals can be sensitised by an intravenous (IV) injection of as little as 0.1 mL of Rh(D)-positive blood, but 30% of individuals are still not sensitised after serial IV injections of 10 mL and 5 mL of Rh(D)-positive blood over a 6-month period. Volume is not the only factor responsible for initiating a maternal response to the paternal antigen on fetal RBCs. The maximum rate of sensitisation after exposure to a full unit of Rh(D)-positive blood is only 80%. Other factors thought to play a role are the frequency of the exposure, a protective effect of ABO incompatibility between the fetus and the mother and the status of the maternal immune system because immunodeficiency may prevent alloimmunisation.
The severity of the fetal anaemia is primarily dependent on the concentration of maternal antibody crossing the placenta into the fetal compartment, but other factors also play a significant role. The following factors are all known to affect the development and severity of HDFN: (i) the subclass and glycosylation of the maternal antibody; (ii) the structure, site density, maturational development and tissue distribution of the fetal blood group antigens; (iii) the efficiency of transplacental IgG transport; (iv) the functional maturity of the fetal spleen; (v) polymorphisms affecting the Fc receptor function and (vi) the presence of human leukocyte (HLA)–related inhibitory antibodies. As an example, maternal antibodies cannot cause fetal anaemia if they cannot cross the placenta or if they are directed against an antigen that is poorly expressed or not expressed on the fetal RBCs. All IgG antibodies are freely transported across the placenta by pinocytosis; however, the IgG1 subclass is more efficiently transported and can more easily result in haemolysis of fetal RBCs. In contrast, IgM antibodies, such as antibodies to the Lewis, I, and P blood groups, do not cross the placenta and therefore do not result in HDFN. Similarly, antibodies to the Cromer blood group bind to placental proteins, preventing their access to the fetal compartment and protecting against the development of HDFN. Antibodies to the Lutheran, Vel and Cartwright blood groups are also unlikely to cause HDFN because these antigens are poorly developed on the RBCs during fetal life. Finally, fetal sex may play a role in the severity of HDFN. Ulm and colleagues demonstrated that Rh(D)-positive male fetuses have a 13-fold increased risk for developing hydrops and an odds ratio (OR) for perinatal mortality of 3.4 compared with Rh(D)-positive female fetuses.
As described earlier, the fetus is not an innocent bystander in the development of fetal anaemia. Extravascular haemolysis of antibody-bound fetal RBCs occurs via phagocytosis by reticuloendothelial macrophages in the spleen and liver. In severe forms of HDFN, intravascular haemolysis by direct lysis of antibody bound fetal RBCs also occurs. Severe anaemia resulting in fetal hydrops occurs when the fetal haemoglobin is greater than 7 g/dL below the mean for the estimated gestational age. This is usually consistent with a fetal haematocrit less than 15% and a fetal haemoglobin less than 5g/dL. Hydrops is associated with end-stage disease and an increased likelihood of a poor fetal outcome. Erythropoiesis is usually elevated in a fetus with the exception of cases of Kell alloimmunisation. The Kell antibody destroys RBC progenitor cells in the fetus and results in an earlier onset and more severe anaemia than that found with other alloantibodies. Hydrops is defined as fluid collections detected by ultrasound in two or more of the following fetal compartments: (i) skin oedema, (ii) ascites, (iii) pericardial effusion and (iv) pleural effusion. Placentomegaly and polyhydramnios are also often included in the diagnostic criteria. Ascites is usually the first finding, followed later by the development of pleural effusions and finally scalp and skin oedema. The exact mechanism for the development of fetal hydrops is not understood. Lower serum albumin levels secondary to the decreased production of proteins by the haematopoietically focused liver has been hypothesised to lead to decreased colloid osmotic pressure, third spacing of fetal fluid and finally the development of hydrops. This theory, however, is not supported by animal models in which the fetal plasma proteins have been replaced by saline or in human fetuses with congenital hypoalbuminaemia, neither of which develop hydrops despite low serum colloid osmotic pressure. Proposed theories to explain the pathophysiology of developing hydrops are (i) iron overload from haemolysed RBCs leading to increased free radical formation and the development of endothelial cell dysfunction, (ii) tissue hypoxia from anaemia leading to increased capillary permeability and (iii) elevated central venous pressures leading to the functional blockage of draining lymphatics. The last theory is supported by the fact that intraperitoneal transfusions (IPTs) are not as effective in hydropic fetuses. The development of hydrops is also gestational age dependent. Hydrops in association with HDFN at less than 22 weeks’ gestation is rare despite the presence of severe anaemia. Yinon and colleagues in their series found that 71% of fetuses with haemoglobin less than 5 g/dL did not demonstrate any evidence of hydrops before their first transfusion. The hyperbilirubinaemia resulting from the destruction of fetal RBCs does not pose the same danger to the fetus as the neonate because the placenta transports the bilirubin to the maternal side. Of specific clinical importance, it is imperative for the physician managing any HDFN case to continue to monitor the infant postnatally for haemolysis because the presence of maternal antibodies in the fetal circulation will continue to cause haemolysis after delivery and still poses a risk for poor neonatal outcomes. This is compounded in a neonate who has received multiple antenatal transfusions because her or his haematopoietic system will be suppressed with minimal reticulocytosis at the time of birth.
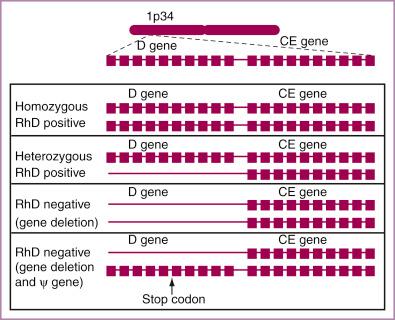
The standard nomenclature for denoting a pregnant women’s blood type is by identifying the ABO type and Rhesus (D) blood type. Other antigens in the Rhesus system also exist, including the C/c, E/e and G antigens. These antigens are all produced by two genes. The RHD gene and the RHCE gene are both located on the short arm of chromosome 1 ( Fig. 40.1 ). A cytosine to thymine change in exon 2 of the RHCE gene leads to expression of the C antigen as opposed to the c antigen, and a single cytosine to guanine change in exon 5 of the RHCE gene results in the expression of the e antigen as opposed to the E antigen. A single amino acid change in the extramembranous portion of the RhD and RhC antigens results in the RhG phenotype.
Often anti-D alloimmunisation is accompanied by a low level of alloimmunisation to anti-C (anti-C titre < anti-D). When an RhD-negative individual is found to have anti-D and anti-C at a similar titre or when the anti-C titre exceeds the anti-D, the RhG phenotype should be suspected.
The prevalence of Rh(D)-negative individuals varies greatly among different populations with a high incidence of Rh(D)-negative individuals in the Basque population (30%–35%) to a relative scarcity of Rh(D)-negative individuals in the Chinese population (0.3%) ( Table 40.2 ). Of all Rh(D)-positive individuals, 40% are homozygous (DD), guaranteeing that any offspring with an alloimmunised partner will be at risk for HDFN; the remainder are heterozygous (D-) and have a 50% chance of having no HDFN risk with an alloimmunised partner.
| Ethnicity | % Rh(D) Negative |
|---|---|
| Basque | 30–35 |
| White: North American and European | 15 |
| African American | 8 |
| African | 4-6 |
| Indian | 5 |
| Native North American and Inuit Eskimo | 1–2 |
| Japanese | 0.3 |
| Thai | 0.3 |
| Chinese | 0.3 |
A majority of Rh(D)-negative individuals result from a gene deletion in both Rh(D) genes (see Fig. 40.1 ), but in some phenotypically Rh(D)-negative individuals, the Rh(D) gene is present but is either not translated or expressed. Alternatively, the RhD antigen can be weakly or only partially expressed.
The Rh(D) pseudogene is common in the African population with 21% of African Americans and 69% of black South Africans expressing it. The Rh(D) pseudogene contains all exons of the normal Rh(D) gene, but there is a stop codon between exons 3 and 4 stopping the translation of the gene into mRNA and preventing any Rh(D) protein from being expressed on the RBC membrane (see Fig. 40.1 ). As a result, the patient is serologically Rh(D) negative.
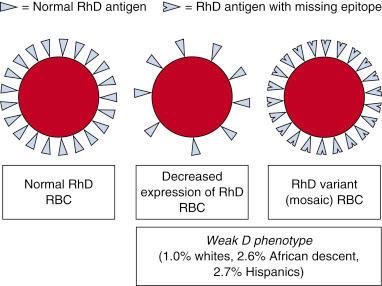
Depending on the reagent used, some patients undergoing RhD typing will reveal a weak D expression. When the patient’s RBCs are tested with an anti-D reagent, they react with no or a 2+ or less reaction; when antihuman globulin is added, there is then a moderate to strong reaction. Previously called Du positive , the term used today for this situation is weak D positive or partial D. The two major explanations for this finding are either a decreased number of intact RhD antigens on the surface of the RBCs or the presence of RhD antigens that are missing epitopes ( Fig. 40.2 ). Weak Rh(D) responses resulting from these two phenotypes are seen in 0.3% of whites and 1.7% of African Americans, and the weak D phenotype was noted in 0.96% of participants in a Canadian study. Although more than 200 mutations have been associated with alterations in the expression of the RhD antigen, the majority of weak D phenotypes are types 1, 2 or 3. When exposed to RhD-positive RBCs, these types do not become alloimmunised to RhD. Other types of Rh variants can, however, form anti-D when exposed to the intact RhD antigen that contains the epitopes they are missing. Alloimmunisation leading to severe HDFN and fetal hydrops has been reported in these individuals.
Some patients may be tested in one laboratory (using a sensitive reagent that detects the weak D phenotype) and told they are RhD positive. Testing in a second laboratory may then report a RhD-negative result. This can occur when the patient is being considered as a blood donor and then is tested again later in a pregnancy. In the United States, a guideline from the American Association of Blood Banks (AABB) does not require that a test for weak D or variant D be performed on Rh(D)-negative pregnant patients. These patients will be considered RhD negative and be candidates for RhIg. Current guidelines from The American College of Obstetricians and Gynecologists (ACOG), however, recommend that patients with a serologic weak D result be considered RhD positive. In an effort to reconcile these guidelines, a working group with representatives from the blood banking and obstetric community was formed to review the literature and make new recommendations. The group recommended that when a discrepant RhD typing was noted or a weak D type was detected, the patient should undergo genotyping. If found to be type 1, 2 or 3, she can be considered RhD positive, and RhIg is not indicated.
The ‘other’ Rh antibodies associated with HDFN are anti-(c) and anti-(E). Although less frequent than anti-Rh(E) antibodies, anti-Rh(c) antibodies have a virulence similar to anti-Rh(D) with IUT required in 1% to 17%, neonatal transfusions needed in 10% to 30% and death in up to 10% of affected cases. A large series of 118 anti-Rh(c) pregnancies also confirmed its virulence with 10% ( n = 12) of the gestations affected with severe HDFN.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here