Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Corticosteroids are increasingly used in the acutely ill newborn population to increase blood pressure and reduce inotrope exposure.
There are clinical and disease states in infants in which glucocorticoids have been studied and found to have potential benefit. Populations who may respond to corticosteroids include ill term and preterm infants with hypotension and infants with pulmonary hypertension, meconium aspiration syndrome, hypoxic-ischemic encephalopathy, sepsis, and congenital diaphragmatic hernia. Cortisol levels have varying clinical utility in these conditions.
Hydrocortisone is the most studied corticosteroid for the treatment of hypotension, and although doses have varied in studies, doses as low as 1 mg/kg/day are effective in stabilizing cardiovascular insufficiency.
Despite the growing literature on the benefits of hydrocortisone for the treatment of hypotension, there remains a lack of data on long-term outcomes. The administration of hydrocortisone in the short term has been associated with hyperglycemia, hypertrophic cardiomyopathy, hypertension, and sepsis.
Glucocorticoid therapy should be tailored for each patient and account for gestational age, condition, and response of the patient while limiting the exposure as much as possible and monitoring for known complications.
Since the last edition of this chapter, studies have continued to observe higher blood pressure and less inotrope need in infants given corticosteroids. However, despite the growing number of studies and the increasing utilization of corticosteroids in newborns, there remains no consensus on a singular pathway for recognition, treatment, and the assessment of best practices and outcomes. This is in comparison to other populations whose societies or colleges have created unified guidelines. The American College of Critical Care Medicine updated their guidelines in 2017 on the hemodynamic support of pediatric and neonatal septic shock. In the same year the Multispecialty Task Force for the Society of Critical Care Medicine and the European Society of Intensive Care Medicine updated their guidelines on critical illness–related corticosteroid insufficiency (CIRCI) in critically ill patients. Since the initial publications of these guidelines, there has been ongoing testing of these guidelines resulting in ongoing changes and improvements. In the newborn population there are no unified standards. The American Academy of Pediatrics (AAP) Committee on Fetus and Newborn (COFN), a leader in proposing standards of care in the United States, recently published its first clinical report in 2022, on the Recognition and Management of Cardiovascular Insufficiency in the Very Low Birth Weight Newborn . However, the section on cardiovascular use of steroids is limited, with no clear trigger or strategy for initiating and administering steroids. The last Cochrane Review on Treatment for Hypotension in Very Low Birth Weight Infants was published in 2011, and corticosteroids were recognized to be as effective as dopamine in treating refractory hypotension but, because long-term safety and benefit data were lacking, they were not recommended for routine use. Corticosteroid treatment in newborn infants for hypotension has been recommended by various experts in general article reviews. In one of these reviews Dr Watterberg proposed one of the most detailed algorithms for use of hydrocortisone for hypotension and included suggested dosing and timing. However, it remains that without a formally established consensus, it is difficult to assess the extent to which these recommendations have been utilized. There have been significant research efforts to better understand the use of corticosteroids in the newborn population; however, large randomized controlled trials (RCTs) designed to evaluate short and long-term effects of hydrocortisone for the treatment of cardiovascular insufficiency are very challenging to conduct and execute. The Neonatal Research Network has attempted to conduct RCTs on the hemodynamic effects of corticosteroids in sick preterm and term infants with hypotension in the past decade but was unable to complete the enrollment of patients. , Reasons for the low enrollment rates included fewer-than-anticipated infants with low blood pressure, difficulties in obtaining consent within the narrow study window, and lack of physician equipoise. In addition, many patients at the time of screening (within 2–12 hours of age or onset of presentation) have already been administered corticosteroids (up to 33% and higher). , The enrollment of preterm infants has also been hampered by high rates of early indomethacin administration. With the difficulty of conducting rigorous studies and given the use of steroids in the acutely ill newborn population, alternative approaches and creativity may be needed to answer the question of best clinical practices, long-term safety, and potential benefits.
There is a need to construct a clear and consensus-driven guideline directing a more standardized approach to the use of corticosteroids in the newborn infant. This should include: (1) triggers to aid recognition of infants who may be amenable to corticosteroids, including clinical presentation, disease states, and laboratory values; (2) a pathway for the administration of corticosteroids, including type, timing, dosing, and duration; and (3) a standardized assessment of performance of the pathway to evaluate safety and overall outcomes.
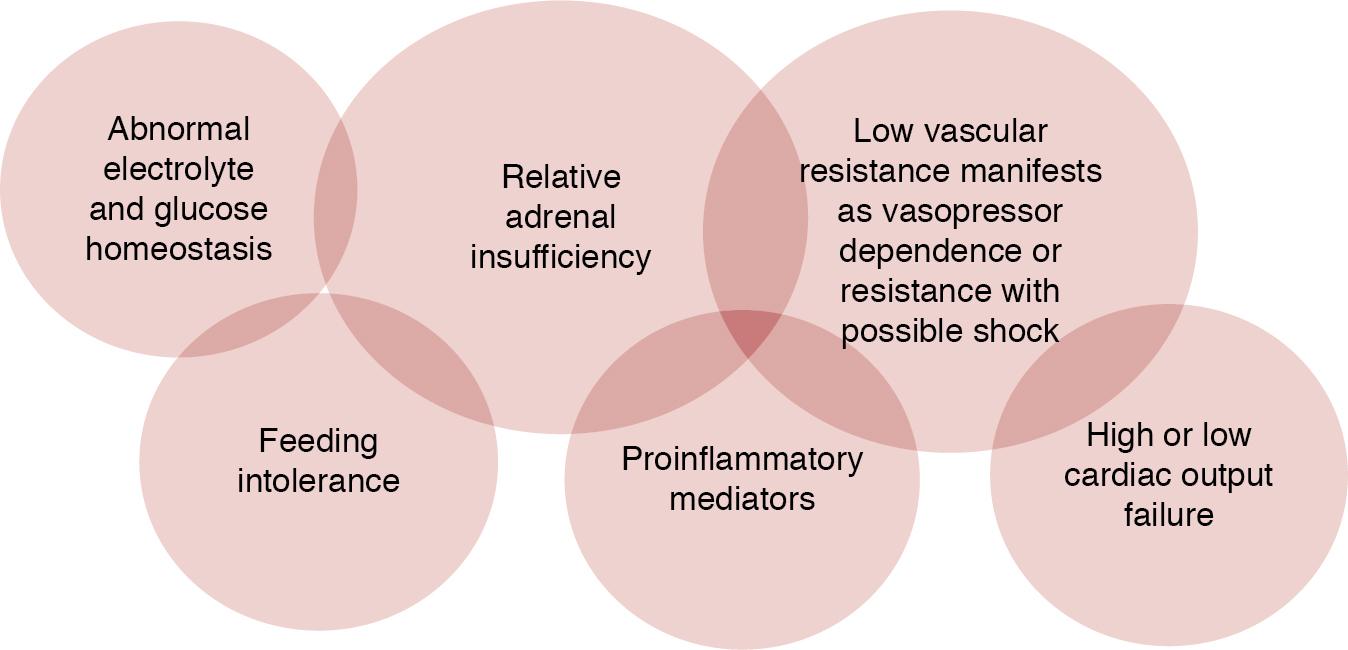
The most common clinical presentation in the newborn infant who may be responsive to corticosteroids is hypotension and, in particular, those with “vasopressor-resistant hypotension”. Vasopressor-resistant hypotension is present when hypotension persists despite vasopressor administration. There are varying definitions of vasopressor-resistant hypotension based on varying inotrope levels but it is most often defined as when dopamine dose is at least >10 mcg/kg/min. Dopamine is usually considered the first line for treatment of hypotension because, despite the fact that small studies showed no difference between hydrocortisone and dopamine as first-line treatment in morbidity or mortality, it is the most studied. Hypotension in the critically ill newborn has been associated with adrenal insufficiency. However, regardless of the presence of adrenal insufficiency, corticosteroids elevate systemic blood pressure, so it is important to understand the populations and disease states in which corticosteroids have been studied. Until there is more information on the effect of corticosteroids on developing organs and their safety, corticosteroids should be limited to those infants requiring “rescue” treatment for vasopressor-resistant hypotension versus prophylaxis. The clinical presentation of infants with adrenal insufficiency often includes hypotension but may also include other signs and symptoms of classic adrenal insufficiency, such as hypoglycemia, hyponatremia, hyperkalemia, acidosis, tachycardia, and weakness ( Figure 23.1 ). However, these signs are often masked by the tightly controlled fluid, electrolyte, and temperature management of infants in the newborn intensive care unit.
While this chapter focuses mainly on infants with transient medical conditions which may be responsive to short-course corticosteroids, the clinical presentation may look the same as for those infants with chronic conditions of adrenal insufficiency. An example of a chronic condition is congenital adrenal hyperplasia which requires an extensive workup and will need long-term glucocorticoid replacement. , Fortunately, these chronic diseases are rare (10–15 per 100,000 for chronic primary adrenal insufficiencies and 150–280 per million for central adrenal insufficiencies). However, it is important not to miss these diagnoses and, when faced with a critically ill newborn with vasopressor-resistant hypotension, it may be prudent to obtain a cortisol level prior to initiating corticosteroids to help guide the potential future evaluation for these chronic conditions. Although a singular random cortisol value is often of limited use in these chronic conditions, a random cortisol value >18–22 mcg/dL most often rules out most chronic conditions of adrenal insufficiency, while those with cortisol values <5–7 mcg/dL in critical illness may prompt further evaluation including, at the minimum, an adrenocorticotrophin hormone stimulation test.
Relative adrenal insufficiency is characterized by its transience because most patients who recover will have normal HPA axis function and corticosteroid activity. Relative adrenal insufficiency is defined as a condition when there is inadequate corticosteroid activity compared with the level of illness in a critically ill patient , and may arise from inadequate cortisol levels resulting from problems anywhere along the HPA axis from synthesis to function or tissue resistance to corticosteroids. Adrenal insufficiency in critically ill patients is also known as “functional adrenal insufficiency”, “transient adrenocortical insufficiency of prematurity”, or “critical illness-related corticosteroid insufficiency”. For the purposes of this chapter, the term “relative adrenal insufficiency” is used interchangeably with these terms. The diagnosis of relative adrenal insufficiency in a critically ill patient should not make one complacent about, or underestimate, the potentially life-threatening nature of this type of adrenal insufficiency. Since the 1980s, relative adrenal insufficiency has become increasingly recognized in sick premature and term neonates, infants, children, and adults. , ,
The overall incidence of relative adrenal insufficiency in critically ill adult patients is approximately 10–20% in general and around 60% in patients with severe sepsis, and septic shock in particular. , Reported proportions of critically ill pediatric patients with “inadequate” cortisol response vary widely, from as low as 2% often up to 87%. , Overall, in the critically ill neonate the incidence is less well understood because there is no consensus on the diagnostic criteria of relative adrenal insufficiency of the ill newborn. , , , However, it has been reported that almost 20% of ill, mechanically ventilated late preterm and term newborns and up to 33% of all extreme preterm newborns in the United States are receiving corticosteroids for cardiovascular insufficiency. ,
The timing of presentation of relative adrenal insufficiency is most often reported in the first few postnatal days in critically ill newborn infants. There is some evidence from a Japanese cohort that adrenal insufficiency can also occur later in life (4–7 days of age) in ill newborn infants with respiratory distress or sepsis. Surveys in Japan found that approximately 4–8% of VLBW infants are receiving postnatal corticosteroid therapy after 7 days of age, with symptoms suggestive of relative adrenal insufficiency, including hypotension and high cortisol precursors. ,
Postulated pathophysiologic mechanisms for relative adrenal insufficiency in ill patients include adrenergic receptor insensitivity due to receptor downregulation ( Figure 23.2 ), proinflammatory cytokine-mediated suppression of the function of the pituitary and adrenal glands, inadequate HPA axis response to stress, limited adrenal reserve, gestational age–associated immaturity of the adrenal gland, corticosteroid tissue resistance, and limited adrenal perfusion ( Figure 23.3 ). , , ,
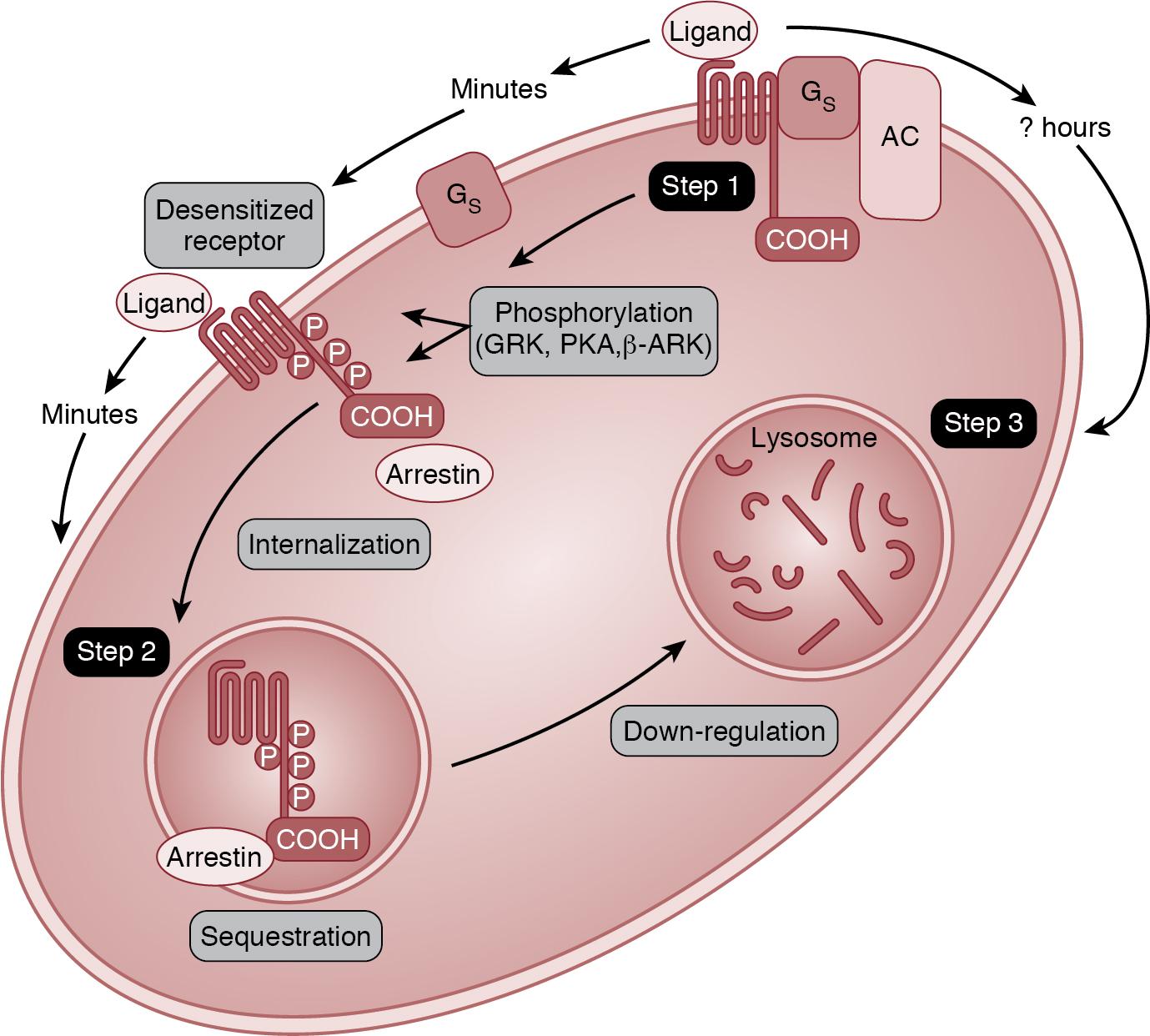
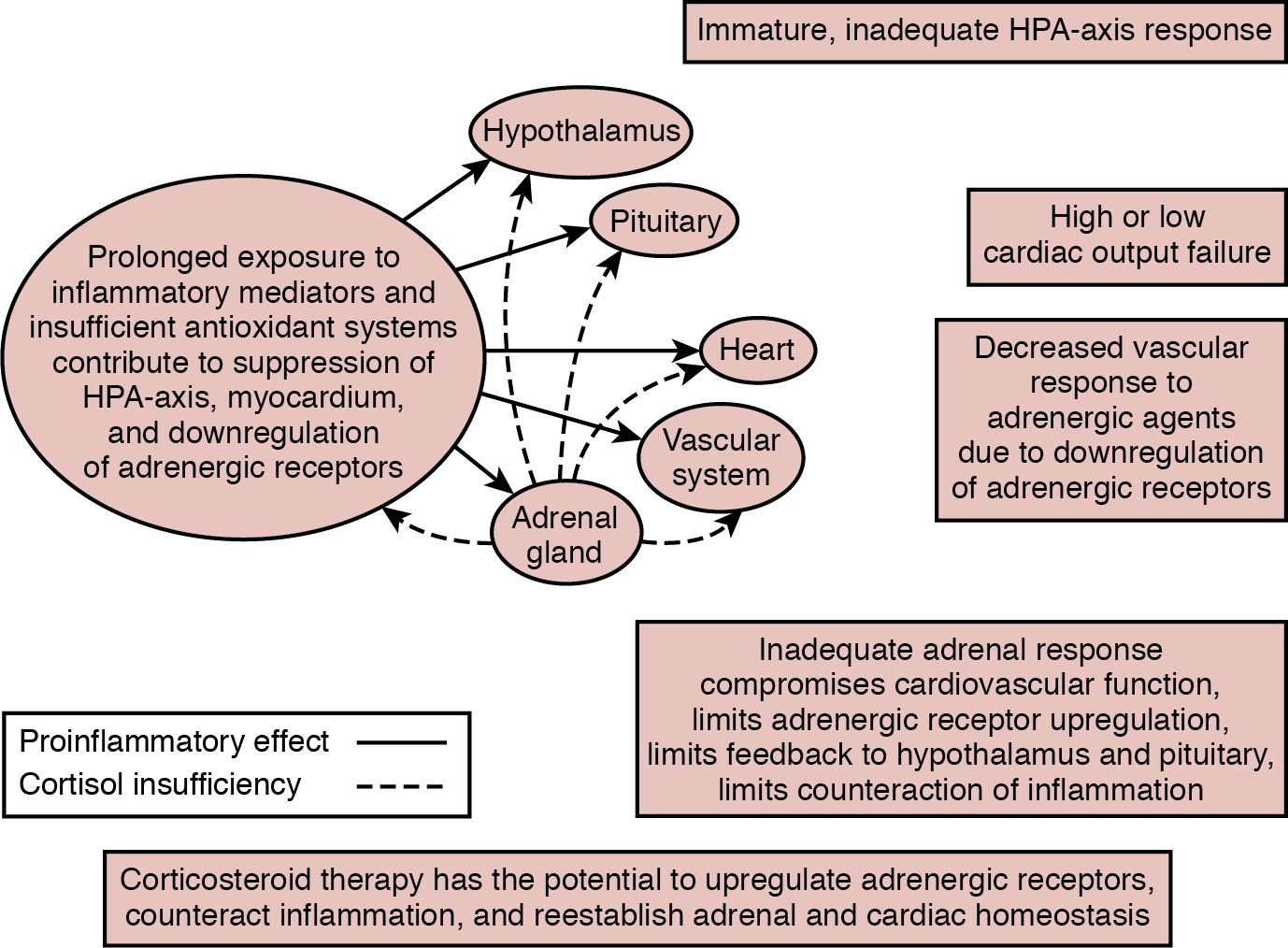
Prolonged exposure to inflammatory mediators is one of the proposed mechanisms for both vasopressor-resistant hypotension manifesting via receptor downregulation and relative adrenal insufficiency presenting with suppression of the function of the adrenal gland and/or HPA axis. Decreased vascular responsiveness to adrenergic agents is due to downregulation of adrenergic receptors. Downregulation of adrenergic receptors in clinical conditions occurs within hours due to prolonged exposure to intrinsic (stress response) or extrinsic (vasopressor therapy) catecholamines and inflammatory mediators such as nitric oxide (NO), tumor necrosis factor, and other inflammatory cytokines (interleukin-1 [IL-1], IL-2, IL-6, interferon-gamma). , Thus production of proinflammatory cytokines also contributes to decreased vascular reactivity to catecholamines and thus to the development of vasopressor-resistant hypotension and has been described in patients with septic shock. In the scenario in which severe illness promotes inflammation and concomitant cortisol insufficiency–associated decreased cardiovascular responsiveness to catecholamines, corticosteroid therapy re-establishes vascular responsiveness and counteracts inflammation.
Newborns, especially those born prematurely, have unique susceptibilities to relative adrenal insufficiency, which is, at least in part, due to the immaturity of their HPA axis and especially the cortical function of the adrenal gland. In addition, the changes in adrenal cortical hormone production, especially cortisol during the transition to extrauterine life and the gestational age–dependent changes in placental 11β-hydroxysteroid dehydrogenase type 2 activity, and thus the effect of maternal corticosteroids on fetal corticosteroid production, pose special challenges for the newborn, especially the preterm neonate. Fetal adrenal glands begin to synthesize cortisol de novo at approximately 22–24 weeks’ gestation, followed by a steady increase throughout the rest of the pregnancy. Corticotrophin-releasing hormone (CRH) production by the placenta also increases through gestation, resulting in maternal and fetal serum CRH concentrations at term that are much higher than at any other time in life. Placental CRH stimulates cortisol production in the fetal adrenal gland. At birth, the very high placental CRH production ceases to have an effect on the newborn. The pituitary gland of the newborn, which has been exposed to high concentrations of CRH during fetal life, may become transiently insensitive to the lower concentrations of CRH produced by the hypothalamus of the neonate. Therefore it may not be able to increase ACTH production to appropriately stimulate the adrenal gland for several days after delivery. Healthy term newborns tolerate this period of relative HPA insufficiency. However, this situation may predispose the newborn to the development of relative adrenal insufficiency in critical illness. Relative adrenal insufficiency could then contribute to the severity of systemic hypotension and attenuate the response of the cardiovascular system to treatment.
Relative adrenal insufficiency has been described in ill preterm infants who present with cardiovascular instability in addition to random and/or stimulated cortisol levels that are inadequate for the degree of illness severity and by rapid clinical and hemodynamic improvement following corticosteroid therapy. , , , , In 1989, Ward and Colasurdo were the first to describe a small cohort of ventilated, sick, extremely premature infants who presented with signs consistent with adrenal insufficiency or “Addisonian crisis”. These infants had signs of relative adrenal insufficiency, including hypotension, oliguria, and hyponatremia and had cortisol values less than 15 mcg/dL (414 nmol/L).
Since this time, subsequent investigations have further elucidated the clinical and laboratory presentation of relative adrenal insufficiency in ill, hypotensive premature infants. , , , , , , , The study by Yoder and colleagues in very premature baboons has provided the most direct, albeit non-human, evidence that relative adrenal insufficiency, cardiovascular insufficiency, and prematurity are related. In earlier studies, this group of investigators documented that most extremely premature baboons, delivered at approximately 67% of baboon gestation (around 26 weeks’ human gestation), required volume expansion and vasopressor-inotrope therapy to treat the subjects’ hypotension, oliguria, and acid-base imbalance. Many of the premature baboons (38%) also required hydrocortisone to successfully treat their hypotension despite receiving vasopressor-inotrope therapy. This group of researchers also demonstrated that decreased urinary free cortisol excretion in the first postnatal day correlated with decreased left ventricular function. Furthermore, hydrocortisone therapy (0.5–1.0 mg/kg/day for 1–2 days) corrected the hypotension and the left ventricular dysfunction, reduced vasopressor-inotrope requirement and mortality, and increased serum cortisol to levels comparable to those seen in baboons with no evidence of relative adrenal insufficiency or cardiovascular dysfunction.
Investigators have documented two intriguing observations regarding cortisol levels in well and sick premature infants. Many healthy premature infants , with no signs of relative adrenal insufficiency, have random cortisol levels that are not detectable or less than 5 mcg/dL (138 nmol/L), a threshold considered to indicate adrenal insufficiency. , , , , , , , , On the other hand, there is a population of sick premature infants with serum cortisol levels similar to or lower than cortisol levels in well preterm or term infants. , , , , , , , The finding that sick premature infants do not have the expected increase in random cortisol levels commensurate with their illness acuity is supportive of the presence of relative adrenal insufficiency in this population.
Relative adrenal insufficiency has been described more often in those ill preterm infants whose predominant clinical presentation is hypotension. Blood pressure has been found to positively correlate with the cortisol production rate, where patients with low random or basal serum cortisol values were more likely to have low blood pressure. In an RCT of hydrocortisone administration in hypotensive preterm infants, the overall baseline (control) median serum cortisol concentrations were 3.3 and 4.1 mcg/dL in the treated and placebo groups, respectively. These values are considered low for the degree of illness severity in preterm infants when compared to the 50th percentile of the serum cortisol values in ill infants (7.2 mcg/dL). In 54 surfactant-treated, 1-day-old preterm infants of 24–36 weeks’ gestation, serum cortisol values were lower in those with left ventricular output ≤180 mL/min/kg compared to those >180 mL/min/kg. , ,
Further support for relative adrenal insufficiency in the preterm population comes from studies that have found that adrenal insufficiency results from immature cortisol synthesis in the adrenal gland. Ng et al. reported normal pituitary response to CRH, but blunted adrenal response, in sick premature infants with vasopressor-resistant hypotension and low serum cortisol values. These findings led Ng et al. to speculate that, in preterm neonates, the adrenal gland was responsible for the adrenal insufficiency. Findings from other investigators support this notion because sick premature infants have been found to have low random cortisol levels, elevated cortisol precursors, and blunted response to ACTH stimulation. , , , , , , , Watterberg et al. reported that, compared with term infants, sick premature infants had higher cortisol precursor concentrations (17α-OH pregnenolone, 17α-OH progesterone, and 11-deoxycortisol) and lower serum cortisol concentrations. In another small prospective study of infants born at less than 30 weeks’ gestation, Huysman et al. demonstrated that critically ill, ventilated infants, compared with less sick, non-ventilated infants, had lower cortisol levels, elevated cortisol precursor levels of 17-hydroxyprogesterone, and insufficient cortisol response to ACTH (0.5 mcg/kg) stimulation. Korte et al. also reported an abnormal adrenal response to cosyntropin (ACTH) in 51 ventilated, premature infants of less than 32 weeks’ gestation who had baseline cortisol levels of less than 5 mcg/dL (138 nmol/L). Among the 51 infants, 64% and 37% had inadequate cortisol response (<9 mcg/dL) to stimulation with 0.1 and 0.2 mcg/kg cosyntropin, respectively. Preterm infants, due to immaturity of the HPA axis, may be at unique risk for adrenal insufficiency and may be considered candidates for corticosteroids when not responsive to otherwise routine management, including volume and vasopressors.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here