Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
After reading this chapter you should be able to assess, diagnose and manage:
conditions presenting with the common symptoms of abdominal disease
conditions resulting in malabsorption
diseases and disorders of the pancreas
diseases and disorders of the liver
congenital malformations and surgical disorders of the gastrointestinal tract and liver
Gastrointestinal conditions commonly present with the following symptoms:
abdominal pain
changes in stool consistency and frequency
vomiting
faltering growth
GI bleeding
Abdominal pain is a common problem in childhood, and a full history and examination is important. Taking a history can be a challenge in younger children as their parents and carers can often interpret vague symptoms such as crying to be caused by abdominal discomfort, when there is little evidence to this as a cause.
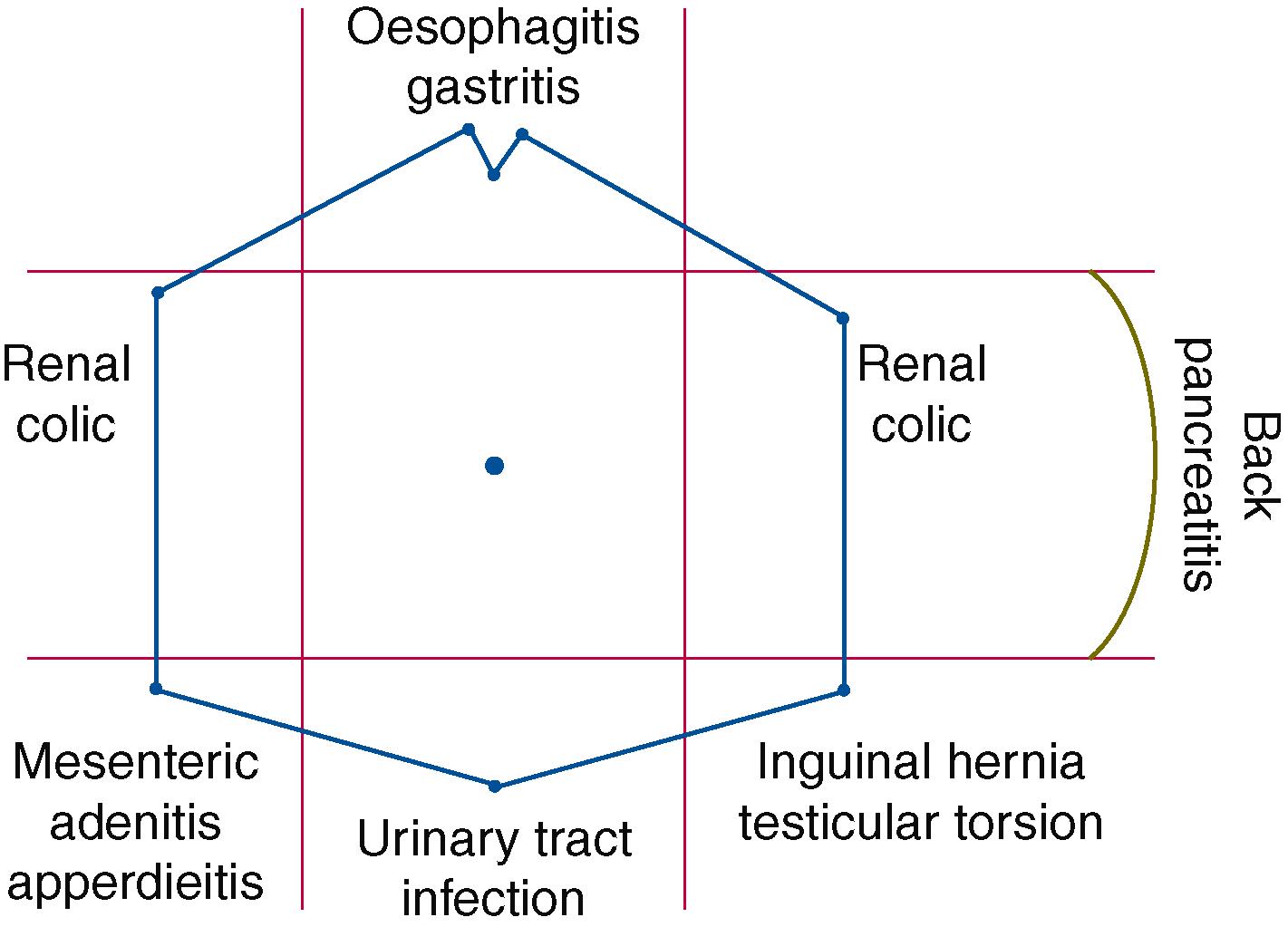
Acute abdominal pain is usually sharp and colicky in nature, and localisation within the abdomen will often suggest the underlying cause ( Figure 19.1 ).
| Symptom | Differential diagnosis |
|---|---|
| fever, nausea, vomiting, anorexia, diarrhoea | gastroenteritis |
| tiredness, jaundice | viral hepatitis |
| cough, shortness of breath | pneumonia or empyema |
| blood in stool | infection |
| necrotising enterocolitis | |
| inflammatory bowel disease | |
| intussusception | |
| bilious vomits | small bowel obstruction |
| urinary frequency, dysuria | urinary tract infection |
| vaginal discharge | pelvic inflammatory disease |
| Differential diagnosis | Investigation | Findings |
|---|---|---|
| pancreatitis | amylase and lipase | elevated |
| biliary colic | abdominal USS | gall stones |
| LFTS | episodic elevation | |
| amylase and lipase | elevated if pancreatic inflammation | |
| renal colic | abdominal USS | renal calculi |
| urea electrolytes | abnormal if obstruction | |
| intussusception | abdominal USS | ‘target sign’ seen |
| inflammatory bowel disease | faecal calprotectin | elevated with inflammatory changes |
| endoscopy—upper and lower | mucosal erythema, loss of vascular pattern, ulcers | |
| MRE (MR enterography) or ultrasound of small bowel | thickened bowel loops | |
| oesophagitis gastritis peptic ulcer disease |
FBC | anaemia |
| urea breath test | positive | |
| stool H. pylori antigen | positive | |
| upper GI endoscopy | inflammatory changes, aphthous ulcers | |
| coeliac disease | coeliac screen | elevated antibodies |
| upper GI endoscopy | abnormal histology—flattened villi | |
| constipation | thyroid function | excludes other causes |
| coeliac screen | ||
| small bowel obstruction | abdominal x-ray | dilated bowel loops |
| contrast study with follow through | abnormal anatomy |
Chronic abdominal pain is usually diffuse and dull in nature although some conditions may have acute episodes. The recognised causes can be divided into organic and nonorganic conditions, and the challenge of identifying the specific diagnosis in children and young people can be difficult.
A diagnosis of functional GI disorders should only be made after organic diseases have been excluded and repeated tests are known to be inappropriate. It can be helpful to raise the idea of a functional disorder at an early stage in the assessments so that patients and carers recognise this as a potential explanation.
The pain in these related conditions is the result of mucosal erosion although the formation of ulcers is uncommon in children. The children and young people usually present with:
abdominal pain
water brash and acid taste in mouth
vomiting
epigastric pain that is worse on eating
melaena stool
haematemesis
unexplained anaemia
The history is often sufficiently clear to warrant a short course of a proton pump inhibitor (PPI) or alginates without the need for more detailed investigations. A follow-up review is advised and, if symptoms do not improve with PPI or if there is evidence of upper GI bleed, then upper GI endoscopy should be considered.
Children and young people with a Helicobacter gastritis may develop chronic epigastric pain although many are asymptomatic. Some may be identified as part of investigations for iron deficiency anaemia whilst others are identified after adult members of the household are diagnosed with the condition.
The older child will be able to perform a urea breath test where radiolabelled carbon in urea is given by mouth. This is then converted to CO 2 and breath analysis will identify the rise in labelled CO 2 after about 20 minutes. The test has a high sensitivity and specificity for Helicobacter. Serology assessing IgG antibodies is less accurate and does not confirm current infection.
NICE recommend an initial treatment of 1 week with:
oral omeprazole
oral amoxicillin
oral clarithromycin or oral metronidazole
Chronic carriage is possible and transmission and reinfection with ‘kissing contacts’ and household members is recognised.
A 14-year-old girl was referred because of shortness of breath on exercise over the preceding 3 years. More direct questioning revealed that she developed a dull central chest pain without radiation and that this was also a significant symptom. There was no associated cough or attendant wheeze. The chest pain also occurred if she undertook heavy lifting. The pain never woke her during the night. Her symptoms did not stop her attending school but she had decided to miss games lesson. Her mother had a specialist referral impending to be assessed for a ‘gastric ulcer’.
On examination the patient looked well and her height and weight were both on the 75 th centile. Examination showed no adverse findings.
Although the initial problem had been that of shortness of breath on exercise, other aspects of the history suggested she may have significant gastro-oesophageal reflux rather than a primary cardiac or respiratory abnormality.
A pH monitoring study was performed and identified multiple episodes of significant low pH in the oesophagus indicating gastro-oesophageal reflux. A urea breath test was positive.
It is likely that the significant gastro-oesophageal reflux led to chronic aspiration and the respiratory symptoms. The increase in abdominal pressure during exercise would have enhanced the reflux and thereby explain the exacerbation of symptoms on these occasions. The presence of Helicobacter pylori also illustrates that two different pathologies can present at the same time and, interestingly, subsequent investigations of the mother revealed she was Helicobacter positive.
This term describes pain related to the gastrointestinal tract that fits with accepted diagnostic criteria for a nonorganic cause. The common characteristics are:
central or periumbilical pain
intermittent pain
pain worsens with stressors such as exams
no radiation of pain
no associated weight loss
A full and honest explanation of the pathway to this diagnosis is important for the patient and carers. In some situations, the exclusion of serious organic pathology can be sufficient to resolve the current symptoms, but the involvement of colleagues in mental health may be helpful for other patients.
The term describes chronic abdominal pain that is cramping in nature and which occurs at least 4 days per month. The pain is often related to defecation and associated with diarrhoea or constipation. Between these episodes, the patient is usually well with good weight gain. Clearly, it is important to exclude other possible causes of such symptoms.
Treatment options include peppermint oil, probiotics or a FODMAP elimination diet where fermentable sugars are removed from the diet. Behavioural treatments may also be able to support the patient in coping with the problem and many will continue with the problem into adult life.
Young people experience recurrent episodes of intense, incapacitating abdominal pain that lasts over an hour and is associated with nausea, headache and pallor. The episodes can be triggered by stress or fatigue and relieved by rest and sleep. Between episodes the patients are well and lead a full and active life.
Avoidance of obvious triggers will usually have been tried, but if the episodes are frequent then prophylactic beta blockers may have a role.
Diarrhoeal illness is common in children and most episodes reflect a transient infective cause. It can, however, be the presenting problem for more significant conditions and lead to dehydration, electrolyte disturbance, malabsorption and subsequent faltering growth.
The diarrhoea can be episodic, profuse, explosive and may contain blood or identifiable food particles.
The approach is twofold and requires an immediate assessment of potential dehydration and associated biochemical disturbances and a parallel series of investigations to determine the possible underlying cause of the diarrhoea. Investigations are not usually required for acute onset diarrhoea as it is often caused by an infective agent. Blood in the stool is a feature of certain organisms as detailed in Table 19.3 .
| Viruses | Bacteria | Parasites |
|---|---|---|
| Rotavirus | Campylobacter jejuni ∗∗ | Cryptosporidium |
| Noroviruses | Salmonella ∗∗ | Giardia lamblia |
| Adenoviruses | Escherichia coli ∗∗ | Entamoeba histiolytica |
| Enteroviruses | Shigella ∗∗ | |
| Cytomegalovirus | Yersinia entercolitica ∗∗ | |
| Hepatitis A | Clostridium difficile ∗∗ | |
| Listeria monocytogenes |
Children and young people presenting with acute diarrhoea need to be assessed promptly and an assessment of their cardiovascular stability made. Most young children are only mildly compromised and can be managed with oral rehydration fluids. Profuse, watery diarrhoea, however, can rapidly lead to significant dehydration and the patient may need parenteral fluids to correct any deficit. Details of the management of fluid and electrolyte problems are covered in Chapter 10 Fluids and electrolytes .
The episodes of diarrhoea can produce significant amounts of stool which may contain blood or identifiable food particles. The stools may be foul-smelling, greasy and will float in the toilet if they have high fat content usually due to malabsorption.
full blood count and CRP
electrolytes and urea
coeliac disease screen
stool culture (including Clostridium difficile and Giardia lamblia )
Subsequent blood tests would look for evidence of immunocompromise or autoimmunity.
| Test | Finding | Implications |
|---|---|---|
| alpha 1 antitrypsin level | raised | protein losing enteropathy |
| faecal reducing substances | present | carbohydrate malabsorption |
| faecal elastase | reduced | pancreatic dysfunction |
| chymotrypsin | reduced | pancreatic dysfunction |
| faecal calprotectin | raised | inflammation |
| fat globules | present | fat malabsorption |
| Investigation | Information identified |
|---|---|
| plain abdominal x-ray | abnormalities in bowel gas pattern |
| abdominal ultrasound | bowel wall thickness and biliary tree structure |
| contrast study with follow through | congenital or acquired structural malformations |
| MRI small bowel | small bowel thickness |
| MRI imaging of the pelvis | perianal disease in IBD |
| upper GI endoscopy | appearance and biopsies of bowel to first part duodenum |
| lower GI endoscopy | appearance and biopsies colonic disorders |
Children and young people with systemic or local GI disease are likely to have problems with digestion of food and malabsorption of calories and necessary nutrients.
Coeliac disease is now recognised as a multiorgan condition with a strong genetic predisposition. Children and young people usually present with gastrointestinal symptoms as the main effect is an immune-mediated, gluten-induced enteropathy that affects small intestine. Gluten is found in wheat, barley and rye and once these are excluded from the diet, a complete recovery takes place.
The close linkage between coeliac disease and specific human leucocyte antigens (HLA-DQ2 and HLA-DQ8) is recognised and most children diagnosed with coeliac disease are positive for the two listed HLA types. Iron is absorbed through the ileal mucosa and consequently anaemia is a common finding.
The introduction of gluten into the diet at 6 to 12 months heralds the start of the GI pathological process and the infant develops chronic diarrhoea, abdominal distension, pain and growth retardation. In older children the symptoms may be more subtle but again poor growth along with problems of malabsorption such as diarrhoea, anaemia, vitamin D deficiency and persistent mouth ulcers may suggest the diagnosis. Dermatitis herpetiformis is associated with coeliac disease but is not common in children.
Coeliac disease has a genetic basis with an autoimmune mechanism of action and is therefore associated with other conditions with a similar underlying pathophysiology. Some units would advocate routine testing for individuals in these groups even if asymptomatic:
first degree relatives of patients with coeliac disease
type 1 diabetes
autoimmune thyroiditis
selective IgA deficiency
juvenile idiopathic arthritis
Down syndrome
Turner syndrome
Specific serological testing is required if coeliac disease is suspected. Prior to blood sampling it is necessary for the child to be exposed to gluten in their diet. This requirement is roughly one slice of bread per day for at least 6 weeks.
The initial coeliac screen includes:
IgA level (those with IgA deficiency will have a negative IgA-TTG result)
serum IgA-TTG (IgA antibodies against tissue transglutaminase—high sensitivity and specificity for coeliac disease
anti-endomysial antibody (EMA—IgA antibodies against intestinal smooth muscle). The test is used to further investigate those patients with a weakly positive TTG-IgA
Previous practice used these blood tests as a screening tool and an elevated result indicated the need for a duodenal biopsy. Current practice, however, is that those with an IgA-TTG greater than 10x upper limit of normal and who are IgA-EMA positive can be recognised as having coeliac disease and a confirmatory biopsy is not necessary.
If these criteria are not met, however, or there is any diagnostic uncertainty, then duodenal biopsy is required. The presence of intraepithelial lymphocytosis and blunting of villi in the tissue sample will confirm the diagnosis.
The assessment of HLA status (DQ2 and DQ8) in the diagnosis can be helpful but should not be used in the initial diagnosis of coeliac disease in nonspecialist settings. The test result may be of value in children who are not having a biopsy, or in those who have limited their gluten ingestion and do not wish to have a gluten challenge.
Once the diagnosis is established, the patient is advised to remove all gluten products from their diet. The support and advice from an experienced dietitian are important at this stage.
Monitoring of the response to the change in diet is necessary along with review of growth parameters. Children will need to take specific supplements such as calcium or vitamin D if their dietary intake is insufficient.
Once clinical improvement is established, then the patients will be offered annual review where height and weight are plotted, symptoms reviewed and need for bone density assessment considered. Normal growth and development, without GI symptoms, would be expected if gluten continues to be omitted from the diet, but support and reinforcement of gluten avoidance are important particularly through the teenage years.
IBD is a chronic relapsing and remitting disease of the gut and includes ulcerative colitis (UC) and Crohn’s disease. The diagnosis is made by the combination of clinical features and recognised findings on endoscopy and histology. Crohn’s disease is characterised by focal, patchy, transmural and granulomatous inflammation affecting any part of the gastrointestinal tract from mouth to anus and can also have extraintestinal manifestations. Ulcerative colitis involves colonic mucosa and therefore extends from the rectum to the ilio-caecal junction.
The presentation of IBD can vary depending on the area of gut involved and the severity of the disease but typically presents in late childhood or adolescence. The most common symptoms are diarrhoea with or without blood along with episodic abdominal pain. Other presenting features include:
faltering growth for either height or weight
delayed puberty
abdominal mass
perianal fissures or skin tags
fever
lethargy
Some features are less commonly seen in IBD and include:
erythema nodosum
uveitis
arthritis
A range of basic investigations is undertaken if there is a suspicion of the diagnosis although normal results do not rule out the diagnosis. Further investigations will be needed to clarify the diagnosis.
FBC—anaemia is common along with raised white cell and platelet count
ESR and CRP are usually raised
albumin levels are often low
stool occult blood—usually present
faecal calprotectin reflects disease activity in both UC and Crohn’s disease
small bowel imaging may include contrast studies, ultrasound of small bowel or MRE
upper and lower GI endoscopy with biopsies define the nature of the condition
Treatment of IBD based on the site, extent and severity of the disease and paediatric scoring systems have been developed to guide the treatment choices. The drugs used vary, depending on histological diagnosis, but the aim is to achieve steroid-free remission within one year of diagnosis. Patients with Crohn’s disease at presentation or with an acute, severe flare will be started on exclusive enteral nutrition to replace all enteral food intake for 6–8 weeks to achieve clinical remission and improve nutrition.
Surgical review and intervention will be required if medical treatment fails to control the disease or if complications such as bleeding, obstruction, perforation or fistulae develop. For Crohn’s disease, conservative surgery to relieve obstruction is recommended whilst for ulcerative colitis, a radical pan-proctocolectomy and ileal pouch is preferred. The gastroenterology MDT will always include a paediatric surgeon.
Corticosteroids will be used in the treatment of an acute flare-up in both UC and Crohn’s disease and IV or oral preparations are available. In an acute flare, steroids are usually given over an 8-week reducing course whilst the topical application of prednisolone (by enema or suppository) can be used for short periods (usually up to 2 weeks) for proctitis or left-sided disease.
Aminosalicylates (mesalazine or sulphasalazine) are used to reduce inflammatory pathways in UC, but not Crohn’s disease, and work topically on the gut.
Thiopurines (azathioprine or 6-mercaptopurine) reduces the number of cytotoxic T cells and plasma cells and thereby inhibits lymphocyte activity.
Biological therapies act to reduce inflammation and are given parenterally or subcutaneously. Anti-TNF agents will supress inflammatory pathways and so used to achieve and maintain remission. Infliximab is a monoclonal antibody and is highly effective at achieving remission in both UC and Crohn’s disease although efficacy can be lost due to antibody-mediated destruction of the drug.
Short bowel syndrome occurs when a section of small bowel is absent, usually secondary to surgical resection, which then leads to the child being unable to meet nutritional requirements without support. Common causes of short bowel syndrome include:
necrotising enterocolitis
malrotation with volvulus
multiple intestinal atresias
trauma
Children have diarrhoea and malabsorption that leads to impaired absorption of calories and nutrients.
This involves meeting calorific requirements and intensive intestinal rehabilitation with enteral or parenteral support. It is important in infancy as the small bowel, and in particular the terminal ileum, has the capacity for adaptation. Loperamide may help some patients by reducing diarrhoea.
This is a rare condition where children have significant protein loss into the gut. It can be associated with:
inflammatory bowel disease
coeliac disease
giardia
intestinal lymphangiectasia.
The intestinal loss will include protein, immunoglobulins and lymphocytes.
Patients will present with peripheral oedema or dyspnoea due to fluid retention and the diagnosis should be suspected in those with a low albumin without a recognised explanation. Some infants may have diarrhoea and weight loss.
Assessment of dietary intake is important and introduction of a diet based on medium-chain triglycerides (MCT) which is low in fats and high in protein. MCT fats enter the portal system directly and avoid the gut lymphatic system. Any identified underlying causes will also need treating.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here