Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
By the end of this chapter the reader should:
Understand the anatomy and embryology of the gastrointestinal tract and how this relates to congenital disorders
Know about normal gut function and the principles of motility, absorption and secretion
Understand the basic histopathology and cellular dysfunction of important disorders, including coeliac disease and inflammatory bowel disease
Know about the role of the gut in acute and chronic diarrhoea
Understand about the genetic and environmental factors in the aetiology of gut disease, in particular coeliac disease and inflammatory bowel disease
Know about the investigations of the gastrointestinal tract
Know about the scientific principles of the common pharmacological agents used to treat gastrointestinal disorders
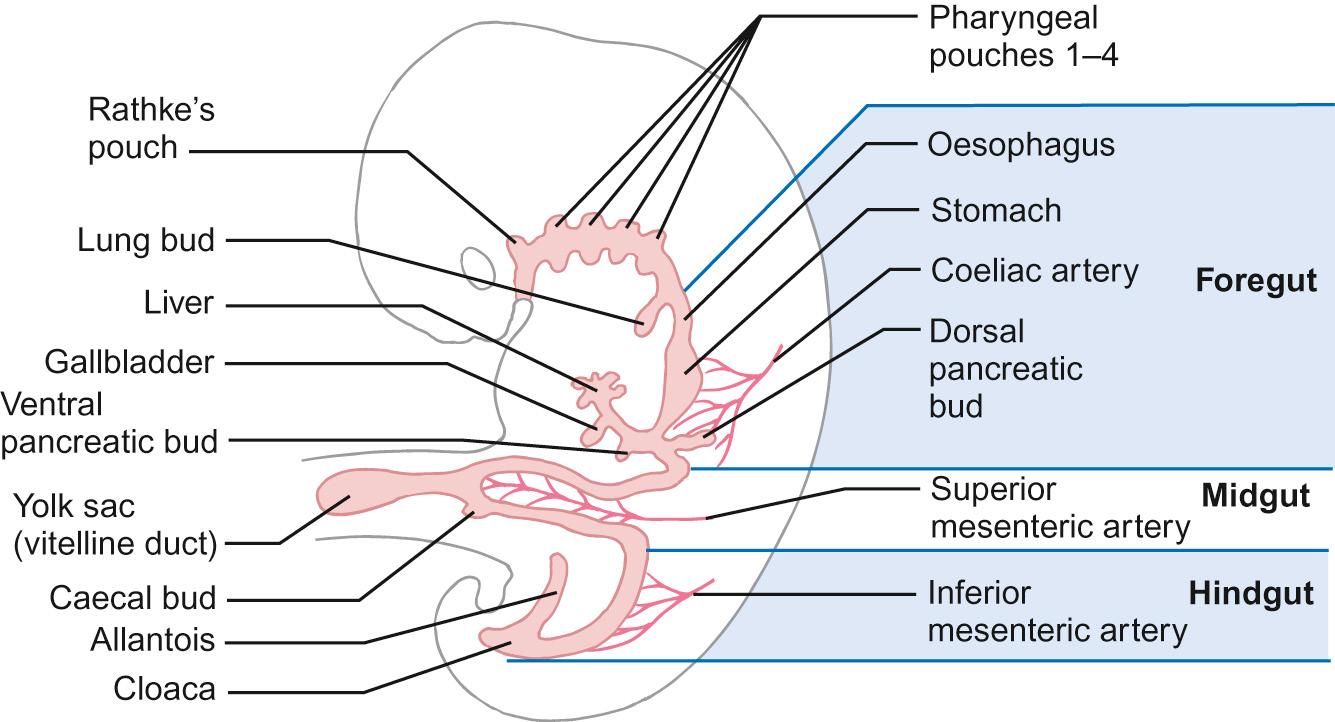
An understanding of the embryology is helpful in understanding why particular problems arise. The human gastrointestinal tract first appears at 4 weeks' gestation and is complete by 12 weeks' gestation. At the 4th week of gestation, the embryo consists of three parts: the endoderm, the ectoderm and the mesoderm. Eventually all three layers form important constituents of the gut: the endoderm gives rise to the epithelial lining of the gastrointestinal tract; the mesoderm, the smooth muscle; and the ectoderm will develop into the enteric nervous system.
Embryonic folding results in a tubular structure with a craniocaudal distribution. Further folding results in the cranial and caudal sections forming into blind-ending tubes which later become the foregut and hindgut, respectively, separated by a section which is still attached to the yolk sac – this later becomes the midgut. As the embryo further develops, the yolk sac becomes smaller and the midgut becomes a separate structure that is still attached to the yolk sac by the vitelline duct. The gastrointestinal tract now has three different structures ( Fig. 14.1 ):
Foregut – forming the pharynx, oesophagus, stomach, proximal duodenum
Midgut – forming the distal duodenum, small bowel and distal colon
Hindgut – forming the distal colon and rectum
The intestine undergoes a number of changes in position ( Fig. 14.2 ):
By week 5, the intestine elongates and begins to form a loop, which protrudes into the umbilical cord.
By week 6, the stomach and duodenum have rotated 90° clockwise.
At week 8, the duodenum and jejunum herniate further from the abdominal cavity and rotate around the axis of the superior mesenteric artery (counterclockwise) by 90° and take up a position behind the superior mesenteric artery.
At week 11, the intestine retracts into the abdomen, although the control mechanism for this is not understood. The jejunum returns first (to the left half of abdomen) followed by the ileum (to the right half) and then the rest of the small intestine and the colon last. By the end of week 11, the caecum has moved downwards and the intestines have reached their final adult position.
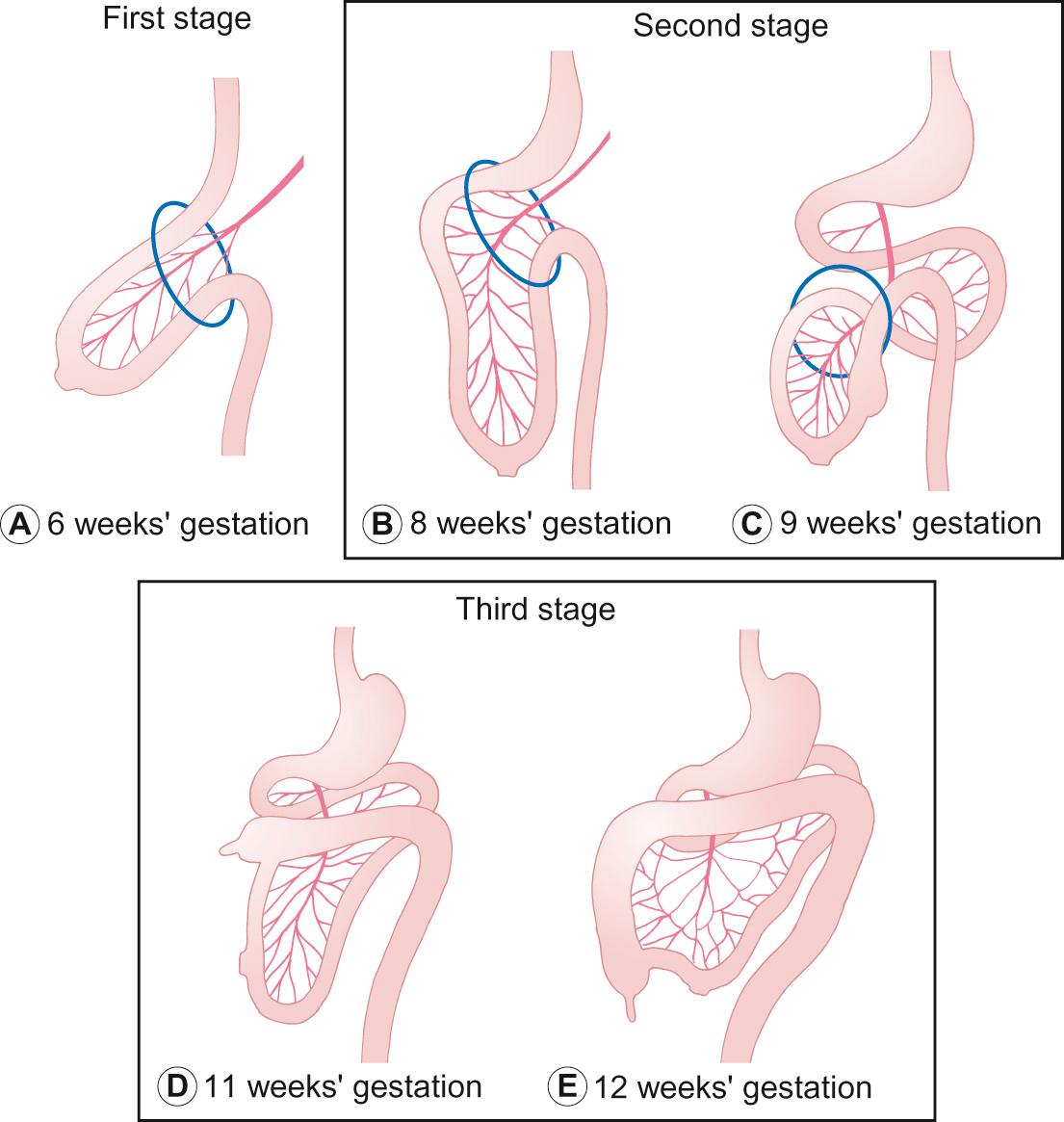
During this period of movement of the gut, the intestinal endoderm is uniform and it only starts to differentiate after the final positions are reached.
Atresias can occur at any point along the gastrointestinal tract, and may be singular or multiple, complete or incomplete. The duodenum is one of the most common sites of atresia; the incidence is 1 in 10,000–30,000 live births. Most occur at the ampulla of Vater, either due to a complete mucosal membrane or a blind-ending proximal loop, probably due to failure of canalization of the duodenum after the 7th week of life due to ischaemia. Associated anomalies occur in about 50% of cases, including Down's and Prader–Willi syndromes. Presentation may be antenatal with polyhydramnios, or a ‘double bubble’ on ultrasound scan. Bilious vomiting is a presenting feature, usually immediately after the first feed.
With an incidence of 1 in 3000, this is a midline defect of the anterior abdominal wall, where some of the organs lie outside the abdominal cavity. The organs are encased in a membranous sac derived from the amniotic membrane. The organs that are contained within the sac vary but can include stomach, intestine, liver and spleen. The defect is classified according to size (major being >4 cm abdominal wall defect and minor <4 cm). Exomphalos is associated frequently with other congenital abnormalities, including trisomy 13, 18 and 21, and 75% of cases also have other associated structural problems such as cardiac anomalies. It is usually identified on antenatal scanning. Surgical closure is required but, depending on the size of the defect and whether the sac remains intact, this is generally not an emergency providing the intra-abdominal structures are well perfused.
The incidence is 4 per 10,000 births and risk factors include low maternal age, drug misuse, low socio-economic status, smoking and ethnic origin. The abdominal muscles are normal but the stomach and intestines herniate through the anterior abdominal wall on the right-hand side of the umbilicus. Associated atresias are found in up to 10% of cases (due to ischaemic events) but other congenital anomalies are not usually present.
The cause is spontaneous herniation of the intra-abdominal wall in utero (possibly at the site of the right omphalomesenteric artery) or from incomplete reduction of the abdominal contents following rotation during the first weeks of fetal life. The abdominal contents are not covered by a membrane and therefore are exposed to amniotic fluid. This results in serositis with matting together of the intestines, which may need resection after birth.
There is a high risk of intrauterine death (15%) due to ischaemia and thus serial antenatal ultrasound scans are recommended. Delivery can be either vaginal or operative, but should take place in a specialist paediatric surgical centre. A protective membrane is placed over the eviscerated abdominal contents to prevent them drying out and urgent surgery is usually required to close the defect. The surgery may be a primary closure, or secondary if the defect is too large to replace all the contents in one stage without causing respiratory compromise from splinting of the diaphragm. In this case, a silo may be used to preserve the intestinal contents while complete closure is awaited.
It often takes time for feeding to be established due to poor intestinal motility. A prolonged course of parenteral nutrition may be necessary. Overall survival is 90%.
This is common (2–4% of newborn infants) and occurs when the remnant of the omphalomesenteric duct does not fully regress and remains attached to the ileal mucosa ( Fig. 14.3 ). The diverticulum contains gastric mucosa, which produces acid. It can often be detected using a technetium-99m scan (the sensitivity of this is 85% in children with a specificity of 95%).

A Meckel's diverticulum may present with lower gastrointestinal bleeding, intussusception, small bowel volvulus or it may never cause any problems, depending on the size of the sac. If problems occur, surgical resection is necessary.
Rarely, failure of the omphalomesenteric duct to regress results in an intestinal fistula that may present with an umbilical discharge. It may appear similar to an umbilical granuloma, but it is possible for a catheter to be inserted. Surgical resection is required.
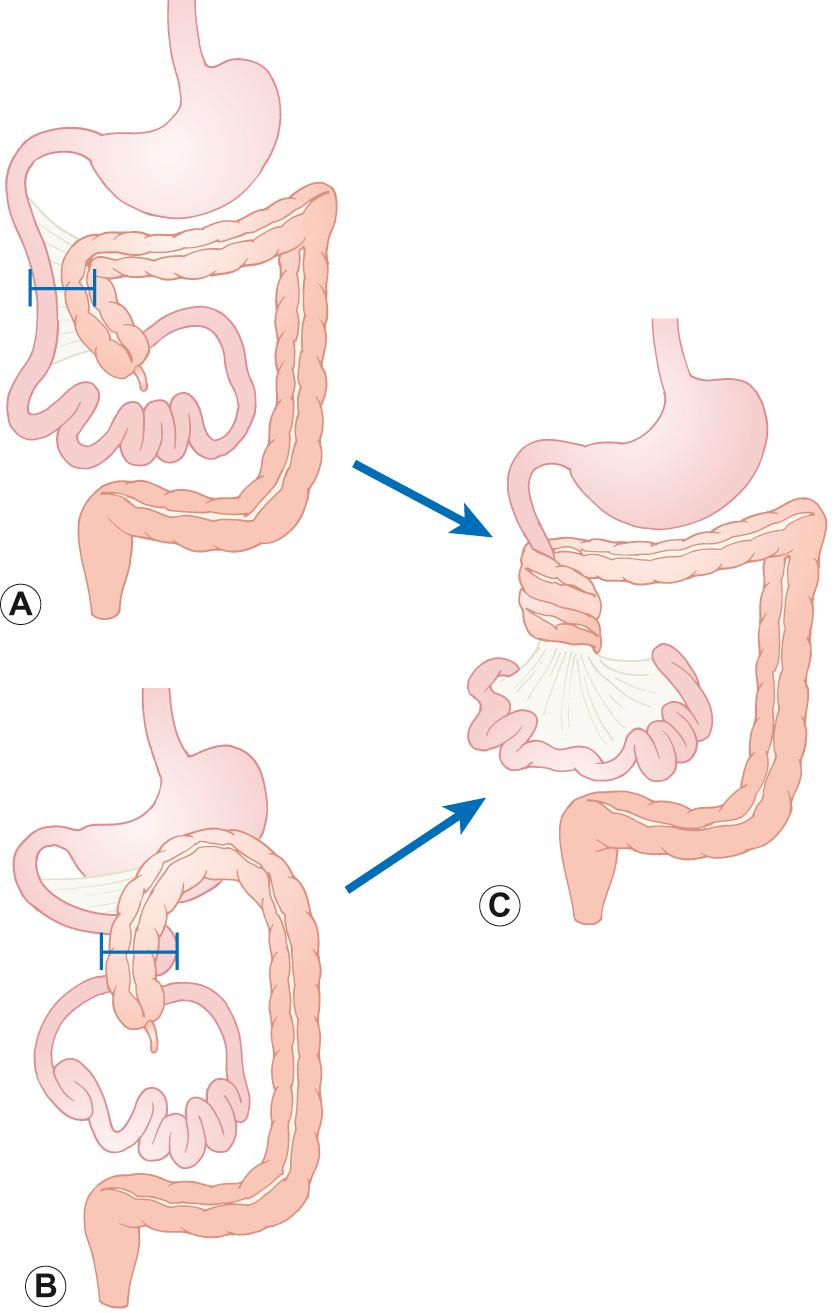
This occurs when the intestine lies in an abnormal position within the peritoneal cavity. It is subsequently at risk of torsion (volvulus) around the superior mesenteric artery axis ( Fig. 14.4 ). Malrotation is due to incomplete rotation of the gut contents during the first 11 weeks of embryogenesis. The most common defect results in the duodenum lying to the right of the vertebral column instead of the left, with the caecum lying in the upper abdomen to the left of the duodenum (Pattern A in Fig. 14.4 ). Bands of peritoneum (Ladd's bands) pass from the caecum, across the duodenum, to the posterior abdominal wall. This may cause extrinsic obstruction of the duodenum, resulting in bilious vomiting, usually in infancy. As a result, the midgut has a short attachment to the base of the superior mesenteric artery and so may twist clockwise around this pedicle, resulting in potentially fatal midgut ischaemia. Midgut volvulus should be suspected in any child with bilious vomiting, as the ischaemia can be potentially reversed if the Ladd's bands are divided and the pressure from the arterial supply to the midgut is relieved. Children may also present with subacute symptoms of intermittent abdominal pain and vomiting. A barium meal is then the investigation of choice as it can show the position of the duodenal–jejunal flexure. The true incidence is not known, as there are probably individuals with undiagnosed malrotation who never have any problems if the pedicle is long enough.
A thriving 3-year-old boy had intermittent vomiting from birth. Gastro-oesophageal reflux was diagnosed, but intermittent vomiting continued, with occasional bilious vomiting. A barium study was requested as an outpatient and was planned for a month later, but he was admitted in shock and was taken to theatre, where malrotation with infarction was diagnosed. He needed major gut resection and the child was maintained on long-term parenteral nutrition for 4 years.
Which segment of gut is most likely to have received the ischaemic insult? Select ONE correct answer only.
Distal gastric body, duodenum, small intestine and proximal colon, as these originate from the midgut and are supplied by the superior mesenteric artery
Distal small intestine and proximal colon, as these originate from the midgut and are supplied by the inferior mesenteric artery
Duodenum, small intestine and proximal colon, as these originate from the midgut and are supplied by the superior mesenteric artery
Duodenum, small intestine and colon, as these originate from the hindgut and are supplied by both the inferior and superior mesenteric artery
None of the above
C. Duodenum, small intestine and proximal colon, as these originate from the midgut and are supplied by the superior mesenteric artery.
Any child with intermittent bilious vomiting must have an urgent contrast study to diagnose an anatomical abnormality such as malrotation.
In cases of pancreatic insufficiency, the distal ileum becomes impacted with thick, viscous meconium. This is associated with cystic fibrosis in most cases, with 20% of newly diagnosed children developing meconium ileus.
Duplication cysts are congenital cysts attached to the gastrointestinal tract anywhere between the mouth and anus, but are found most commonly in the ileocaecal region. The histological nature of the cyst is related to the adjoining structure. Presentation may be with an abdominal mass, or obstruction. When problems occur, surgical excision is required.
In Hirschsprung's disease, there is an absence of ganglion cells in a variable segment of bowel (aganglionosis). The incidence is 1 in 5000 live births, and is more common in boys. The sigmoid and rectum are the most commonly affected sites, although the whole colon and, very rarely, the entire large and small bowel can be affected. The lack of ganglion cells causes an inability of the bowel to relax, resulting in a functional bowel obstruction.
It should be suspected in infants who have not passed meconium in the first 48 hours of life or in infants who present with bowel obstruction. Dramatic decompression occurs on digital examination of the rectum, with so-called ‘explosive diarrhoea’. Digital examination should be performed by a senior doctor, and limited to only one examination, where possible.
Diagnosis is confirmed by rectal suction biopsy to confirm the absence of ganglion cells (in older children, a strip rectal biopsy). Surgery is needed to remove the aganglionic section of bowel. Enterocolitis is one of the major complications after surgery, when children can present with malaise, fever, diarrhoea and generalized sepsis. The pathophysiology of this is incompletely understood, but is thought to be due to gastrointestinal stasis, altered gut flora and impaired mucosal immunity.
These occur in 1 in 2500 births. The pathophysiology is poorly understood, but it is thought to be due to failure of the breakdown of tissue at the caudal end of the gastrointestinal tract in week 3 of gestation. Most often identified on routine post natal check, 60% have other congenital malformations of the gastrointestinal tract and/or genitourinary tract; in boys there may be a fistula to the urethra, in girls to the vestibule adjacent to the vagina. Other anomalies (e.g. VACTERL) should be considered.
Intussusception is not classically considered as an embryological abnormality and can occur in the presence of a structurally normal gut. However, even minor gut abnormalities, such as a polyp or Meckel's diverticulum, may predispose a child to this condition. It occurs when one section of the intestine invaginates into another section and can result in obstruction. The most common site is at the ileocaecal junction, but it can occur at other sites if there is a lead point such as a polyp or a Meckel's diverticulum. Patients usually present with acute onset abdominal pain, drawing up of the legs and pallor. They may have ‘redcurrant jelly’ stool, but this is a late sign. Diagnosis is by ultrasound scan, which shows a target-shaped mass. Treatment aim is to reduce the intussusceptions with an air enema, but surgical reduction may be necessary.
The primary functions of the gut are to maintain fluid homeostasis and to facilitate absorption of dietary nutrients. There are complex mechanisms of secretion, digestion, absorption and motility that take place throughout the gastrointestinal tract to allow these functions to take place.
The digestive juices that are secreted throughout the GI tract are a mixture of water, electrolytes, enzymes, bile salts and mucins, which aid digestion. When there is excess secretion or a failure to reabsorb enough of these secretions, either vomiting or diarrhoea results.
This is the process by which complex food particles are broken down to smaller units that can be absorbed across the gut mucosa. Enzymes aid this breakdown.
Carbohydrates must be broken down to monosaccharides before absorption. The starch, glycogen and cellulose, the main sources of dietary carbohydrates, must be broken down to fructose, glucose and galactose to allow absorption.
Proteins are broken down to their constituent amino acids.
Fats (mainly triglycerides) are broken down to monoglycerides and fatty acids.
Most absorption takes place in the small intestine (see the later section on small intestine for details).
Motility is the function of the gastrointestinal tract that allows movement of the contents of the intestine in a craniocaudal direction. It is the food contents themselves that stimulate the contraction of the muscles above the food bolus and relaxation of the muscles below the bolus to produce craniocaudal progression.
The smell, thought and presence of food stimulates production of saliva from the sublingual, submandibular, parotid and buccal glands. Saliva contains mainly water, but also contains small quantities of the salivary enzymes amylase (which converts polysaccharides to maltose), mucus (to allow lubrication) and lysozyme (that lyses certain bacteria). Chewing of food particles is the first stage of breakdown of food and allows easier passage into the oesophagus. Whilst some drugs can be absorbed through the buccal mucosa (e.g. midazolam), no absorption of nutrients takes place here.
When a food bolus is moved to the back of the pharynx, the swallowing centre in the cerebral medulla is activated. This results in closure of the vocal cords and epiglottis, and facilitates safe passage of the bolus into the oesophagus. Sphincters at the lower and upper end of the oesophagus prevent food particles from refluxing back to the mouth.
The upper oesophageal sphincter remains tonically contracted and only relaxes to allow food particles through. It is under the control of cranial nerves V, IX and X. Peristalsis within the oesophagus is stimulated by swallowing of a food bolus. Inhibitory neurons induce lower oesophageal sphincter relaxation and coordinate proximal-to-distal peristaltic contraction. When the lower oesophageal sphincter fails to relax, achalasia results, and usually needs surgery to divide the muscles at the lower oesophageal sphincter to allow the passage of food into the stomach. Achalasia is a rare condition in children, but can still occur. No further digestion or absorption of food takes place here.
The stomach has a number of functions including storage of food, secretion of the digestive juices and mixing up the contents of the stomach into chyme.
The smooth muscle of the stomach wall has the unique property of ‘plasticity’. In fully grown children and young adults, this allows the stomach to hold between 50 mL and 1000 mL of stomach contents whilst the pressure or tone exerted on the contents remains the same. The folds of stomach mucosa, or ‘rugae’, stretch out as the stomach becomes fuller. Once the stomach has become fully distended, the individual will experience discomfort and usually this will prompt them to stop eating.
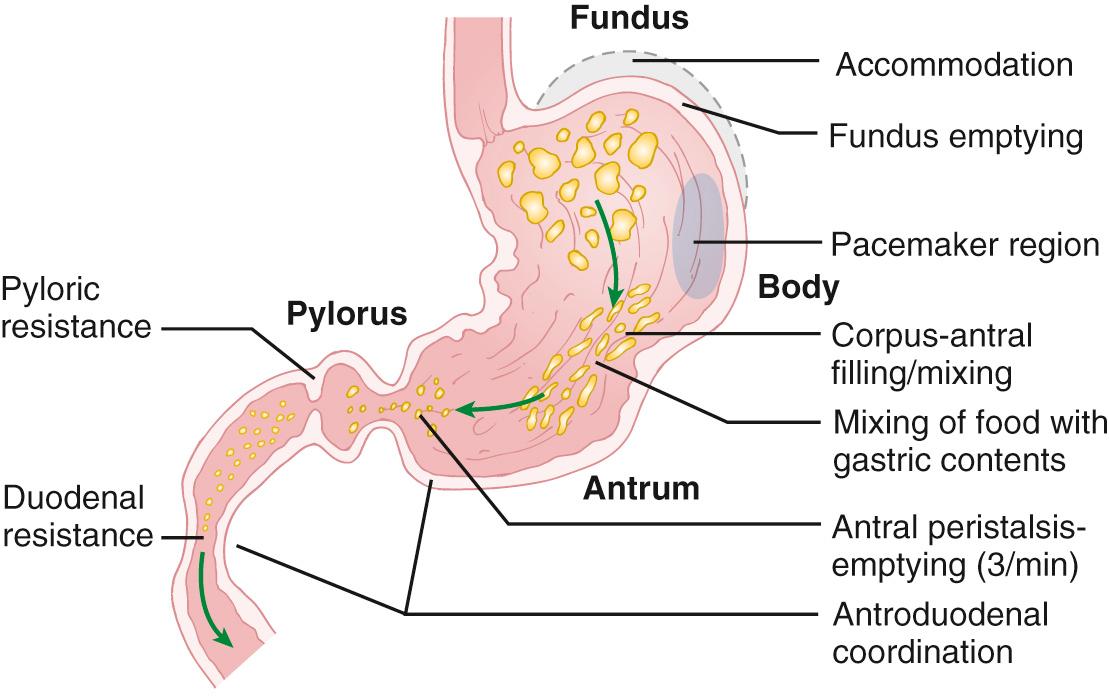
The cells in the fundus generate slow-wave potentials that move down the length of the stomach towards the pylorus at a rate of 3 per minute. This contraction occurs rhythmically and does not cause contraction of the circular muscles. The muscle layers in the fundus of the stomach are significantly thinner than the antrum, so the strength of these contractions is lower at the proximal end.
The antral peristaltic contractions are responsible for the mixing of food. The pylorus will only open enough to allow the very watery chyme through; the thicker chyme is not able to pass through, so as the peristaltic wave meets the pylorus, the majority of the contents of the antrum are actually propelled backwards against the pylorus and back into the antrum for further mixing.
In a well-hydrated typical child, the stomach produces between 10 and 20 mL/kg of gastric fluid per day. This includes water and a combination of secretions which arise from the gastric pits.
Mucous neck cells secrete bicarbonate and mucus. The latter provides a protective barrier against damage from mechanical trauma from peristalsis, autodigestion and acid.
Chief cells produce pepsinogen. Pepsinogen is actually a precursor of pepsin, and must be converted to pepsin in order to allow protein digestion to amino acids.
Parietal cells produce hydrochloric acid and intrinsic factor. Hydrochloric acid activates pepsinogen to its active form, pepsin, and helps break down connective tissue fibres within food contents whilst destroying microorganisms within the food. Intrinsic factor is important for the absorption of vitamin B 12 in the terminal ileum.
G cells are found in the pyloric area and secrete the hormone gastrin, which is integral in stimulation of the parietal and chief cells to produce their enzymes.
Enterochromaffin-like cells produce histamine, which in turn stimulates gastric acid secretion by the parietal cells. D cells produce somatostatin, whose functions include the inhibition of acid secretion.
At birth, gastric pH is in the neutral range (between 6 and 8), owing to the presence of alkaline amniotic fluids within the stomach. Within a day, the pH generally falls to between 1 and 3. However, gastric acidity is poorly maintained in neonates and is increased towards neutral following a milk feed. Only by age 3 years does the production of acidity reach adult capacity.
The stomach absorbs relatively few products of digestion but can absorb glucose, simple sugars, amino acids and some fat-soluble substances (notably ethanol). The gastric pH determines absorption for some drugs. For instance, at a low pH aspirin is absorbed from the stomach almost as rapidly as water, but, as the pH of the stomach rises, aspirin is absorbed more slowly. Water moves freely from the gastric contents across the gastric mucosa into the blood. The net absorption of water from the stomach is small, however, because water moves just as easily from the blood across the gastric mucosa to the lumen of the stomach. The absorption of water and alcohol can be slowed if the stomach contains foodstuffs and especially fats, probably because gastric emptying is delayed by fats, and most water in any situation is absorbed from the small intestine.
The rate of emptying of the stomach depends upon the physical and chemical composition of the meal. Fluids empty more rapidly than solids, carbohydrates more rapidly than proteins, and proteins more rapidly than fats.
A 6-week-old boy presents to the emergency department with a one week history of vomiting. The parents report that the vomiting has got much worse over the last two days and the child is now very hungry and unsettled. His older sister, who is now 5 years old, had pyloric stenosis as an infant, but neither parent had the condition themselves. A 10-year-old brother is unaffected. On examination, he has visible peristalsis (a slow muscular contracture, 3/minute) of the stomach visible in the upper part of the abdomen and ultrasound scan confirms pyloric stenosis.
Concerning the heritability of pyloric stenosis and assuming random mating in the future, which family member is MOST likely to conceive a child with pyloric stenosis in future pregnancies? Select ONE answer only.
The infant
The infant's father
The infant's mother
The older brother
The older sister
E. The older sister.
Pyloric stenosis is a classic example of a polygenic disease. There is an unequal sex distribution, with boys being more likely to be affected than girls. The explanation for this is thought to be that an affected female is more likely to have an affected child than an affected male. It is believed that the biological threshold for expression of pyloric stenosis is higher in females. It follows that an affected female must have a greater genetic predisposition than an affected male. Therefore, an affected female is more likely than any other member of this family to conceive a child with pyloric stenosis. This is a helpful example to consider in other polygenic diseases where there is an unequal sex distribution (and is called the Carter effect).
As the contents of the stomach pass into the duodenum, they are mixed with secretions from the exocrine pancreas and the liver. The acinar cells of the exocrine pancreas produce the proenzymes trypsinogen, chymotrypsinogen and procarboxypeptidase and also sodium bicarbonate, which is required to neutralize the hydrochloric acid from the stomach, and provide the correct pH environment for pancreatic enzymes to work. These enzymes are secreted as precursors to reduce the risk of autodigestion of the pancreas. Trypsinogen is activated by enterokinase in the brush border of the small intestine to the active form, trypsin. Pancreatic amylase is also produced to further aid carbohydrate digestion.
Pancreatic lipase is the only enzyme throughout the GI tract that can break down fats, and, when there is pancreatic insufficiency, for example in cystic fibrosis, the pancreatic lipase must be supplemented to prevent fat malabsorption. Pancreatic insufficiency often presents as steatorrhoea.
Pancreatic exocrine secretions are controlled by the hormones secretin and cholecystokinin. Secretin is produced in response to the presence of acidic chyme in the duodenum. Cholecystokinin is produced when fat is present in the duodenum.
The liver has many functions, but with regard to the GI system, it is involved in the metabolic processing of all major categories of our diet following their absorption from the intestine. The venous drainage of the stomach and small intestine is via the portal vein to take the nutrients to the liver for processing and storage. The other major role of the liver in the GI system is to make and secrete bile salts via the gall bladder.
Large volumes of fluid are secreted into and reabsorbed by the intestine. In adults, the daily fluid exchange is:
Input into small intestine: 9 L/day (diet: 1.8 L; endogenous secretions: 7.2 L)
Input into colon: 1.5–2.0 L/day
Output of fluid in faeces: 100–200 mL/day
The intestinal mucosa is a complex epithelium in which absorption and secretion occur simultaneously, with the majority of total water and electrolyte absorption occurring in the small intestine. The mucosa of the intestine acts as a semi-permeable membrane with pores in the membrane at intercellular junctions. Water movement is entirely passive, the majority passing paracellularly in response to osmotic gradients created by the transcellular absorption of solutes, particularly sodium.
The jejunum is the most permeable area of the small intestine and consequently there are rapid changes in luminal osmolality as food is digested and products absorbed. The most important absorptive mechanisms are those of sodium coupled cotransport of organic substrates such as glucose, galactose, amino acids and tripeptides.
The ileum is less permeable to water, though there is absorption of the same sodium and organic substrates as in the jejunum, but also with specific electrolyte absorptive mechanisms (sodium/chloride transport) becoming more significant.
Fat absorption is not as straightforward as monosaccharide and amino acid absorption, as the fat that enters the duodenum is not soluble. Fat that enters the duodenum is in the form of triglyceride droplets, which must be emulsified by the addition of bile salts from the gall bladder. Biliary components facilitate absorption of the fats by the formation of micelles. The bile acids are then reabsorbed in the terminal ileum via the enterohepatic circulation. Once the micelles cross the brush border of the intestine, they are re-assimilated into triglycerides and form fat globules once again, known as chylomicrons. These enter the central lacteals and are absorbed via the lymphatic system.
Vitamin absorption is facilitated by the absorption of water for water-soluble vitamins and micelles for fat-soluble vitamins (vitamins A, D, E and K).
A 2-year-old boy was admitted to his local children's assessment unit with a 48-hour history of vomiting and diarrhoea. Several other members of his nursery had similar symptoms. He had been unable to tolerate oral fluids and diet at home and had not had a wet nappy for 14 hours. On examination, he was clinically dehydrated but his abdomen was soft and non-tender. He was able to tolerate small but frequent amounts of oral rehydration solution (ORS) and was discharged 6 hours later.
Which of the following mechanisms BEST describes the known physiology of oral rehydration solution? Select ONE answer only.
Glucose is rapidly absorbed across the duodenum and this pulls a water molecule across the epithelial surface
Glucose is absorbed passively and sodium is absorbed actively in the small intestine
ORS is hypotonic and therefore water enters the GI tract through osmosis, ensuring rapid rehydration
Sodium and glucose are absorbed passively in the jejunum
Water is absorbed rapidly from the stomach providing that glucose and sodium are present within the mixture
B. Glucose is absorbed passively and sodium is absorbed actively in the small intestine.
Overall, water absorption is dependent on the movement of electrolytes, especially sodium. The primary mechanism of sodium absorption is by the glucose-sodium transporter 1. This promotes the active absorption of sodium, allied to the absorption of glucose, with water moving down the electrochemical gradient that is created as jejunal contents are broken down. This is the scientific basis for the use of oral rehydration solutions used in the management of gastroenteritis ( Fig. 14.6 ).
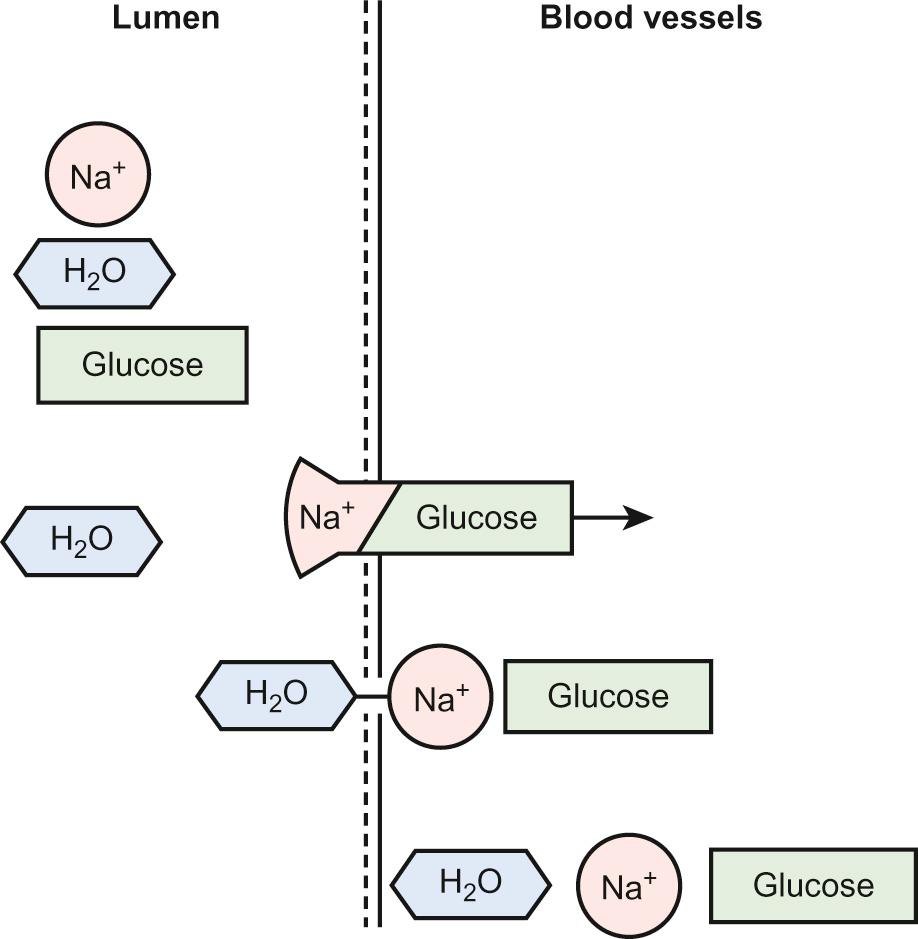
In gastroenteritis, giving oral saline solution is not helpful because normal sodium absorption is impaired in the diarrhoeal state and if the sodium is not absorbed, neither is water. In fact, excess sodium in the lumen of the intestine causes increased secretion of water and the diarrhoea worsens. If glucose is added to a saline solution then glucose molecules are absorbed through the intestinal wall. This is unaffected by the diarrhoeal disease state. In conjunction, sodium is carried through by a cotransport coupling mechanism. This occurs in a 1 : 1 ratio, one molecule of glucose cotransporting one sodium ion. Glucose does not cotransport water – rather, it is the relative increase in concentration of sodium ions across the intestinal wall which pulls water through after it. Several other molecules apart from glucose have a similar capacity to cotransport Na + including:
Amino acids (e.g. glycine)
Dipeptides
Tripeptides
The absorption of these molecules may occur independently of each other at different sites – thus, their effect can be additive. Research is currently being carried out to utilize these additive effects to develop a multi-component ‘super ORS’.
The movement of sodium provides energy for the active transport of amino acids, glucose and galactose across the membrane. Di- and tripeptide amino acid transport over the brush border is coupled with hydrogen ion reabsorption, and so helps to create the electropotential across the brush border, which again aids the transport of sodium.
The ATPase sodium/potassium pump is located in the basolateral membrane of the intestinal crypt and villus tip cells. The epithelial cells at the tips of the villi are active in net absorption, whereas the cells in the crypts of Lieberkühn function as net secretors of electrolytes and water via the ATPase sodium/potassium pump. In these crypts, there is also a luminal bidirectional sodium/chloride channel, which is opened when there are higher levels of cyclic AMP and calcium ions. When these channels are open, there is a net movement of sodium, chloride and water into the lumen. Consequently, if there is a slight change in the flow across this channel, then secretion dramatically increases. Cholera toxin and E.coli cause an increase in the levels of cAMP, so driving chloride flow across the brush border into the lumen, and hence the net movement of water with it. This results in watery, secretory diarrhoea.
Whilst the majority of water and electrolyte absorption takes place in the small intestine, the colon is also important for the adequate reabsorption of fluid. It is often the adequacy of colonic function that determines whether or not the patient experiences diarrhoea. The maximal absorptive capacity of the adult large bowel is 2–3 L/day and, if the amount of fluid secreted from the small bowel exceeds this, then diarrhoea results.
The motility of the colon is produced via the haustrations, but these usually contract very slowly and 30 minutes can elapse between haustral contractions in adults.
The gastrointestinal tract from the mouth to the anus is a tubular structure with four main layers:
Mucosa – epithelium, connective tissue and thin smooth muscle
Submucosa – connective and supporting tissue
Muscularis externa – two thick layers of smooth muscle
Serosa – thin outer layer of connective and supporting tissue
The oesophagus consists of non-keratinized stratified squamous epithelium. Peristaltic contractions of the muscularis externa propel the food boluses forward into the stomach.
The mucosa of the stomach is made of columnar epithelium with mucus-secreting cells that invaginate down, forming gastric pits. The gastric pits become deeper from the fundus to the pylorus. The gastric mucosa is populated with many immune cells, including plasma cells and lymphocytes.
The small intestine shares similar histological elements, including an inner lining formed of transverse ridges ( plicae circularis ), tall finger-like projections of mucosa (villi) between which are the crypts of Lieberkühn and the mucosal epithelium is columnar. Microvilli greatly increase the surface area of the small intestine, to approximately 250 m 2 in adults. The duodenum can be clearly distinguished by the presence of Brunner's cells. Brunner's cells are found at the hepatopancreatic sphincter (sphincter of Oddi) and produce an alkaline substance to aid digestion. The jejunum has the tallest villi, which extend from the permanent circular fold of the mucosa and submucosa. The ileum is identified by the presence of aggregated lymphoid follicles, known as Peyer's patches, which are found in the submucosa.
Throughout the gastrointestinal tract there are many immune cells, but predominantly lymphocytes in the surface epithelium and in the lymphoid follicles. Collectively, these make up the gut-associated lymphoid tissue (GALT). Other immune-mediating cells are found in the small intestine, called Paneth cells, which are located in the crypts and contain granular material important in the lysis of microorganisms.
The colon appears smooth when viewed macroscopically, but has a number of microscopic crypts that extend down to the muscularis mucosa. Many goblet cells, whose main function is the production of mucus, are found here.
Coeliac disease (CD) is a multisystem disease, including a small intestinal enteropathy secondary to exposure to gluten. The classic histological findings of coeliac disease include:
Flattened duodenal mucosa with loss of crypt architecture
Intraepithelial lymphocytosis
Glandular hyperplasia
These histological findings are completely reversible on a gluten exclusion diet.
Crohn's disease and ulcerative colitis both show typical histological findings.
Crohn's disease can demonstrate changes anywhere from mouth to anus. It typically shows areas of chronic inflammation, comprising increased lamina propria plasma cells and lymphocytes. So-called ‘skip lesions’ including patchy erosions or ulcers, vertical fissures, and fistulas are typical. Transmural inflammation with multiple lymphoid aggregates and granulomas are pathognomonic.
Ulcerative colitis affects only the large bowel with alteration of crypt architecture including cryptitis and crypt abscesses and increased chronic inflammatory cells in the lamina propria including lymphocytes and plasma cells.
Eosinophils are normally found throughout the GI tract. The normal number of eosinophils per high-powered microscopic field remains uncertain. However, in eosinophilic disease of the GI tract there is a markedly increased eosinophilic infiltrate in the mucosa. The symptoms associated with eosinophilic disease vary according to the site of the disease. For example, eosinophilic oesophagitis often presents with dysphagia and retrosternal chest pain or bolus dysphagia (food boluses lodged in the oesophagus), whereas eosinophilic intestinal disease may present with recurrent abdominal (often epigastric) pain, vomiting, dysphagia or diarrhoea. Data pertaining to eosinophilic oesophagitis is the most researched and better understood, with an accepted diagnostic range of 15 eosinophils per high-powered field. The disorder is described in more detail in Chapter 16, Allergy .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here