Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The authors acknowledge the contributions of Drs. Jeffrey D. Browning and Jayaprakash Sreenarasimhaiah to this chapter in previous editions of the book as well as the contributions of colleagues in the gallstone field. This work was supported in part by research grants DK54012, DK73917, DK101793, DK106249, DK114516, and AA025737 (D.Q.-H.W.) from the National Institutes of Health (U.S. Public Health Service).
Cholesterol cholelithiasis is one of the most prevalent and costly digestive diseases in Western countries. At least 20 million Americans (≈12% of adults) have gallstones. The prevalence of gallstones appears to be rising due to the epidemic of obesity, associated with insulin resistance and the metabolic syndrome. Each year, roughly 1 million new cases are discovered. Although many gallstones are “silent,” about one third eventually cause symptoms and complications. An estimated 700,000 cholecystectomies are performed for gallstone disease, and medical expenses for the treatment of gallstones exceeds $6 billion annually. In addition, unavoidable complications of gallstones result in 3000 deaths (0.12% of all deaths) per year. In the USA, persons with gallstone disease have increased cardiovascular disease, cancer, and overall mortality.
Based on chemical composition and macroscopic appearance, gallstones are divided into 3 types: cholesterol , pigment , and rare stones . The majority (≈75%) of gallstones in the USA and Europe are cholesterol stones, which consist mainly of cholesterol monohydrate crystals and precipitates of amorphous calcium bilirubinate, often with calcium carbonate or phosphate in one of the crystalline polymorphs. These stones are usually subclassified as either pure cholesterol or mixed stones that contain at least 50% cholesterol by weight. The remaining gallstones are pigment stones that contain mostly calcium bilirubinate and are subclassified into 2 groups: black pigment stones (≈20%) and brown pigment stones (≈4.5%). Rare gallstones (≈0.5%) include calcium carbonate stones and fatty acid–calcium stones. Gallstones also are classified by their location as intrahepatic , gallbladder , and bile duct (choledocholithiasis) stones . Intrahepatic stones are predominantly brown pigment stones. Gallbladder gallstones are mainly cholesterol stones, with a small group of black pigment stones. Bile duct stones are composed mostly of mixed cholesterol stones.
Investigations of gallstone prevalence are more common than those of gallstone incidence because of the nature of the statistical analyses. Prevalence is often defined as the number of cases of gallstones at any one point or period of time divided by the population at risk of forming stones. Incidence is usually defined as the number of new cases of gallstones occurring in a time period divided by the population at risk of forming stones. Therefore, the determination of incidence requires that investigation for gallstones be performed at a minimum of 2 different times—that is, at the beginning and at the end of an interval of time. By contrast, prevalence can be determined by sampling at only one point in time—for example, at US screening or autopsy.
Although determining the true incidence of gallstones in a given population is not easy, a large study of the incidence of gallstones in the Danish population has been performed. The 5-year incidence of gallstones was 0.3%, 2.9%, 2.5%, and 3.3% for Danish men, and 1.4%, 3.6%, 3.1%, and 3.7% for Danish women ages 30, 40, 50, and 60, respectively. Women have a higher incidence than men at ages 30 and 40 years, but the difference declines with increasing age. These incidence rates may reflect an interaction between genetic and environmental factors on gallstone formation in the specific populations studied because they are in accordance with estimated prevalence rates reported for Denmark and other populations. In a major Italian study, the incidence of gallstones was obtained at 10 years’ follow-up in an originally gallstone-free cohort in the town of Sirmione. This study revealed that new cases of gallstones developed at a rate of 0.5% per year. Although age, female gender, parity, obesity, and hypertriglyceridemia were associated with gallstones in the cross-sectional prevalence study of Sirmione, multivariate analysis of risk factors for the formation of gallstones in the longitudinal study identified only age and obesity as risk factors.
Differences in the incidence of gallstone formation among different populations are striking, suggesting that genetic factors play a crucial role in the pathogenesis of cholesterol gallstones. Pathogenic factors are likely to be multifactorial and to vary among populations. Most relevant studies have found that the prevalence of gallstones in women ranges from 5% to 20% between the ages of 20 and 55, years and from 25% to 30% after the age of 50 years. The prevalence in men is approximately half that of women of the same age.
US screening or autopsy data are often used to estimate the prevalence of gallstone disease in different populations, as illustrated in Fig. 65.1 . Although US screening cannot be used to distinguish cholesterol from pigment stones, 70% to 80% of detected gallbladder gallstones are assumed to be cholesterol stones.
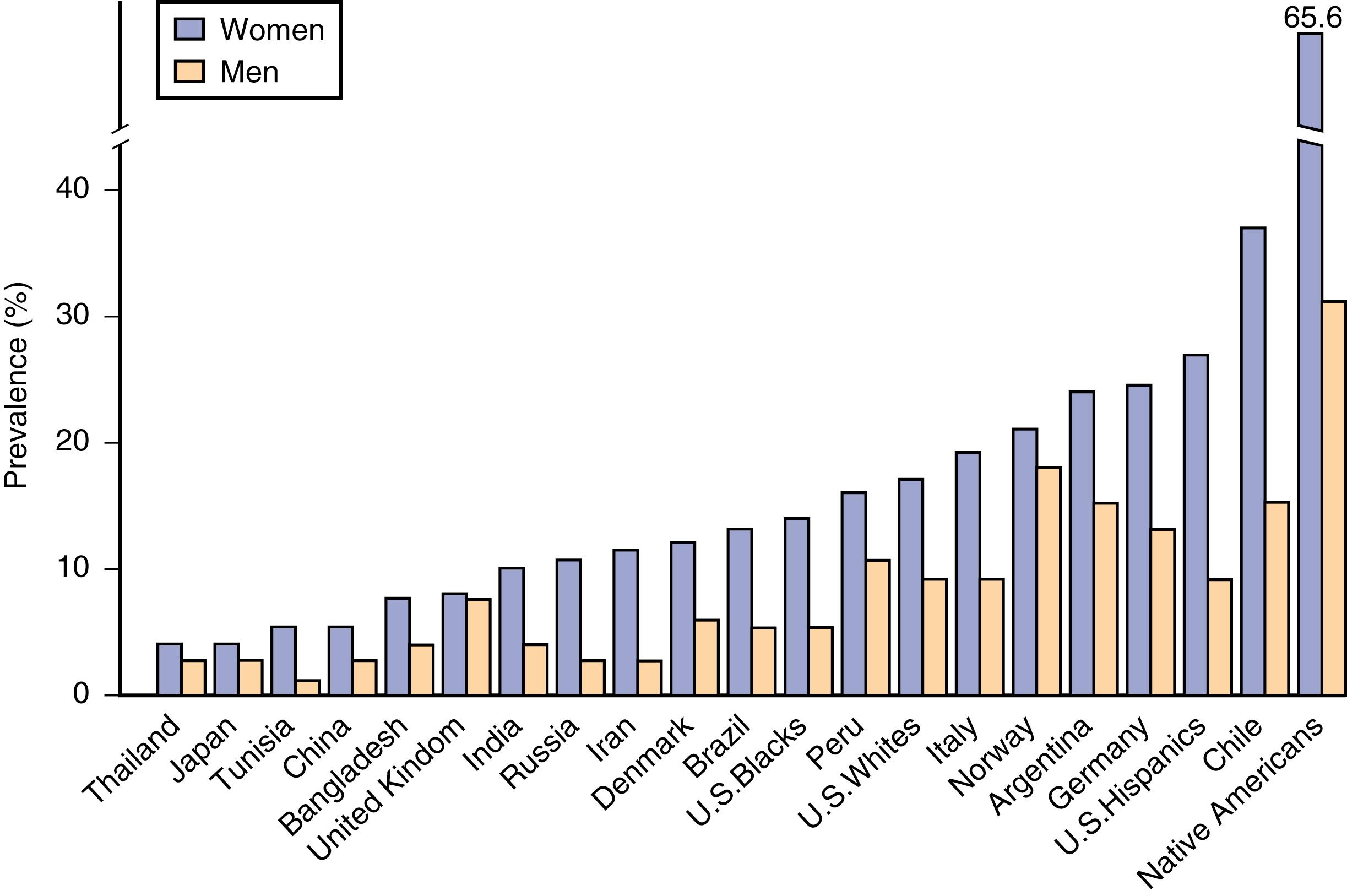
The prevalence of gallstones in American Pima Indians was investigated by oral cholecystography (OCG). The well-studied Pima Indians in southern Arizona exhibit a high prevalence of gallstones, which occur in 70% of the women after the age of 25 years. Subsequently, real-time US was used for screening in nationally representative samples of civilian Mexicans, Hispanic white Americans, non-Hispanic white Americans, and non-Hispanic black Americans of both genders ages 20 to 74. The cross-sectional prevalence rates of gallstones were found to be highest in certain tribes of Native Americans (e.g., Pima Indians), higher in Hispanic Americans than in whites, and lowest in black Americans.
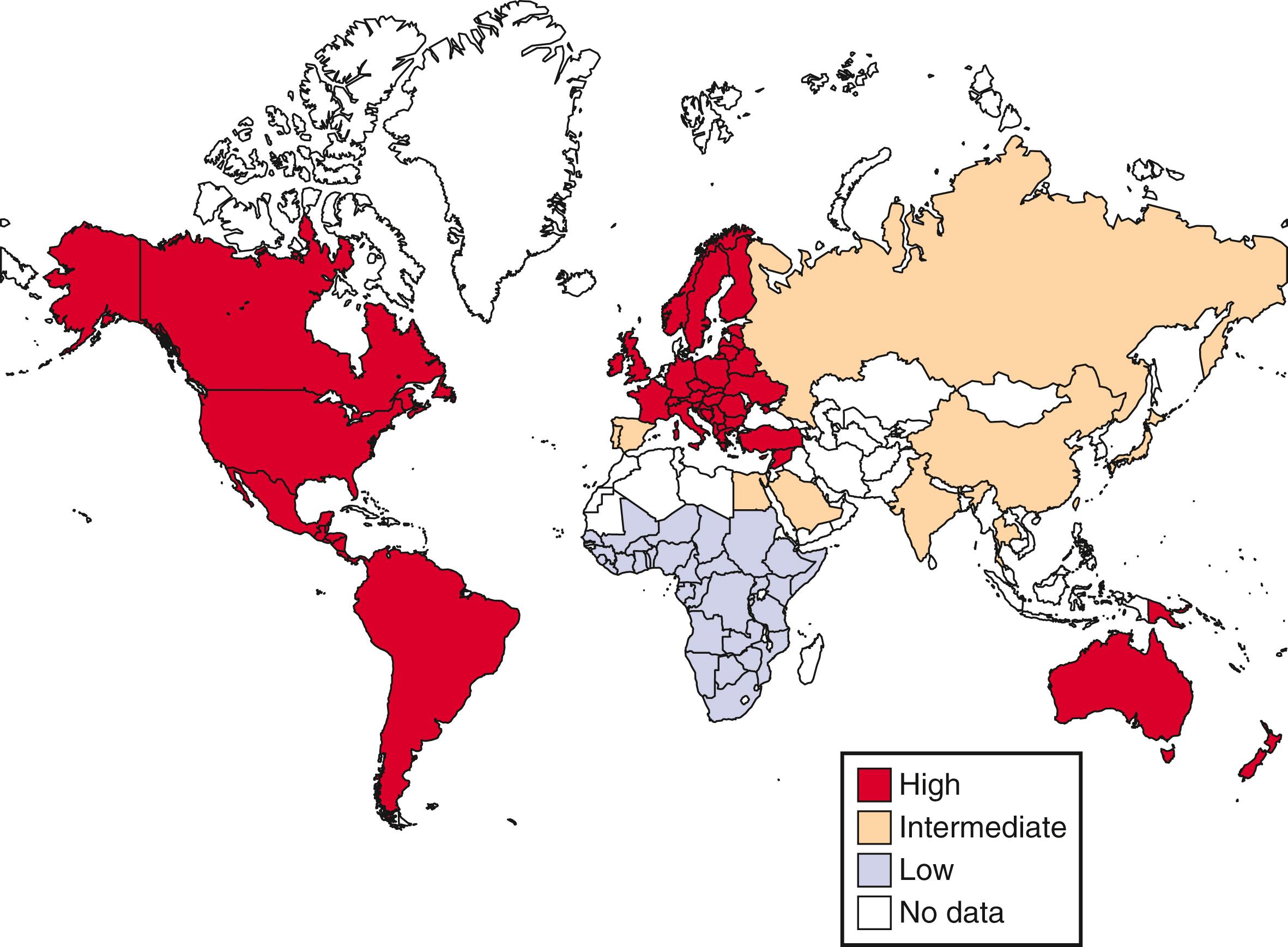
Fig. 65.2 shows the world distribution of cholesterol gallstones. American Pima Indians are an extremely high-risk population. Other high-risk populations include Native American groups in North and South America and Scandinavians, of whom 50% develop gallstones by age 50. By contrast, African populations show the lowest risk of gallstones. The prevalence of gallstones in Asian populations is intermediate. Within a given population, first-degree relatives of index cases of persons with gallstones are 4.5 times as likely to form gallstones as matched controls, thereby underscoring the importance of genetic predisposition.
Epidemiologic and clinical studies have found that cholesterol gallstones occur infrequently in childhood and adolescence, and the prevalence of cholesterol gallstones increases linearly with age in both genders and approaches 50% at age 70 years in women. Furthermore, older adults are at higher risk for complications of gallstones, and mortality from surgery is often unacceptably high in patients older than 65 years. Cholesterol saturation of bile is significantly higher in older Swedes and Chilean women than in younger controls, and age correlates positively with an increased hepatic secretion rate of biliary cholesterol. In animals, aging has been shown to be associated with increased cholesterol gallstone formation as a result of increased biliary secretion and intestinal absorption of cholesterol, decreased hepatic synthesis and secretion of bile salts, and reduced gallbladder contractility.
Epidemiologic investigations have found, and clinical studies have confirmed, that at all ages, women are twice as likely as men to form cholesterol gallstones. The difference between women and men begins during puberty and continues through the childbearing years because of the effects of female sex hormones and differences between the sexes in metabolism of cholesterol by the liver in response to estrogen. Human and animal studies have shown that estrogen increases the risk of cholesterol gallstones by augmenting hepatic secretion of biliary cholesterol, thereby leading to an increase in cholesterol saturation of bile.
Epidemiologic investigations have shown that cholesterol cholelithiasis is prevalent in populations that consume a Western diet consisting of high amounts of total calories, cholesterol, saturated fatty acids, refined carbohydrates, proteins, and salt, as well as a low amount of fiber. The prevalence of cholesterol gallstone disease is significantly higher in North and South American as well as European populations than in Asian and African populations. Several clinical studies have found an association between the increased incidence of cholesterol gallstones in China and westernization of the traditional Chinese diet. In Japan, cholesterol cholelithiasis was once rare, but since the 1970s, the adoption of Western-type dietary habits has led to a markedly increased incidence.
Pregnancy is a risk factor for the development of biliary sludge and gallstones. During pregnancy, bile becomes more lithogenic because of a significant increase in estrogen levels, which result in increased hepatic cholesterol secretion and supersaturated bile. In addition, gallbladder motility is impaired, with a resulting increase in gallbladder volume and bile stasis. These alterations promote the formation of sludge and stones in the gallbladder. Increased progestogen concentrations also reduce gallbladder motility. Because plasma concentrations of sex hormones, especially estrogen, increase linearly with duration of gestation, the risk of gallstone formation is high in the third trimester of pregnancy. Increasing parity is probably a risk factor for gallstones, especially in younger women.
Rapid weight loss is a well-known risk factor for the formation of cholesterol gallstones. As many as 50% of obese patients who undergo gastric bypass surgery form biliary sludge and eventually gallstones within 6 months after surgery. Gallstones also develop in 25% of patients who undergo strict dietary restriction. Furthermore, about 40% of these patients display symptoms related to gallstones within the same 6-month period. The mechanisms by which rapid weight loss causes gallstone formation include enhanced hepatic secretion of biliary cholesterol during caloric restriction, increased production of mucin by the gallbladder, and impaired gallbladder motility. Gallstones may be prevented in this high-risk population by prophylactic administration of UDCA, which, in a dose of 600 mg/day, has been reported to reduce the prevalence of gallstones from 28% to 3% in obese patients on a very-low-calorie diet (see later).
TPN is associated with the development of cholelithiasis and acalculous cholecystitis. As early as 3 weeks after initiation of TPN, biliary sludge often forms in the gallbladder because of prolonged fasting. In addition, the sphincter of Oddi may fail to relax, leading to preferential flow of bile into the gallbladder. Approximately 45% of adults and 43% of children form gallstones after 3 to 4 months of TPN. Because patients who receive TPN often have serious medical problems and are not good candidates for abdominal surgery, prophylactic treatment to prevent gallstones should be prescribed if no contraindication exists. CCK octapeptide administered twice daily via an IV line to patients on long-term TPN has proved to be safe and cost effective and should be used routinely in TPN-treated patients.
Biliary sludge is a crucial intermediate stage in the pathogenesis of both cholesterol and pigment gallstones because it facilitates crystallization and agglomeration of solid plate-like cholesterol monohydrate crystals, as well as precipitation of calcium bilirubinate, and ultimately develops into macroscopic stones. In addition, biliary sludge can induce acute cholecystitis, cholangitis, and acute pancreatitis. Furthermore, biliary sludge is associated with many conditions that predispose to gallstone formation, including pregnancy, rapid weight loss, spinal cord injury, long-term TPN, and treatment with octreotide. Although biliary sludge is reversible in most cases, it persists or disappears and reappears in 12% to 20% of affected persons and eventually leads to gallstones. UDCA treatment of patients with persistent biliary sludge decreases the frequency of clinical complications of biliary sludge (see later).
Most, but not all, relevant clinical studies have shown that use of oral contraceptive steroids and conjugated estrogens in premenopausal women doubles the prevalence of cholesterol gallstones. Moreover, in a large French study of 45,984 postmenopausal women, use of hormone replacement therapy was associated with an increased risk of cholecystectomy (hazard ratio [HR], 1.10); the increase in risk was limited to women who received unopposed estrogen (HR, 1.38).
Administration of estrogen to postmenopausal women and estrogen therapy to men with prostatic carcinoma have similar lithogenic effects. Therefore, estrogen has been proposed to be an important risk factor for the formation of cholesterol gallstones. In mice, the hepatic estrogen receptor α, but not β, plays a crucial role in cholesterol gallstone formation in response to estrogen. The hepatic estrogen receptor α, which is activated by estrogen, interferes with the negative feedback regulation of cholesterol biosynthesis by stimulating the sterol-regulatory element binding protein-2 (SREBP-2) pathway, with the resulting activation of the SREBP-2–responsive genes in the cholesterol biosynthetic pathway. These alterations lead to increased hepatic secretion of newly synthesized cholesterol and supersaturation of bile, thereby predisposing to precipitation of solid cholesterol monohydrate crystals and formation of gallstones. Moreover, genetic analysis in mice reveals that the G protein–coupled receptor 30 (GPR30), a novel estrogen receptor, is a gallstone gene named Lith18 . GPR30 exerts a synergistic lithogenic action with estrogen receptor α to enhance estrogen-induced gallstone formation. In addition, estrogen induces a decrease in plasma LDL cholesterol levels and an increase in plasma HDL cholesterol concentrations. The decrease in plasma LDL levels is a result of increased expression of the hepatic LDL receptor, which increases the clearance of plasma LDL. The increased uptake of LDL by the liver may also result in increased secretion of cholesterol into bile. High levels of estrogen may induce gallbladder hypomotility and consequently bile stasis.
Lipid-lowering drugs may influence the formation of gallstones because they regulate key pathways in cholesterol and bile salt metabolism. Clofibrate is a lipid-lowering drug associated with gallstone formation. Clofibrate induces cholesterol supersaturation in bile and diminishes bile salt concentrations by reducing the activity of cholesterol 7α-hydroxylase (the rate-limiting enzyme in bile salt synthesis of classical pathway) (see Chapter 64 ). The 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (statins) reduce the biliary cholesterol saturation index (CSI), but their role in the prevention or therapy of gallstone disease requires further investigation in humans. The potent cholesterol absorption inhibitor ezetimibe prevents formation of cholesterol gallstones and facilitates dissolution of gallstones in gallstone-susceptible C57L mice. Ezetimibe may also act as a potent biliary cholesterol-desaturating agent in patients with gallstones. Cholestyramine and nicotinic acid have no association with gallstone formation.
The somatostatin analog octreotide increases the prevalence of gallstones when administered to patients as treatment for acromegaly, with approximately 28% of treated acromegalic patients forming gallstones. Acromegalic patients who are treated with octreotide display dysfunctional gallbladder motility, sluggish intestinal transit, and increased colonic deoxycholic acid formation and absorption, all of which facilitate formation of cholesterol gallstones.
The third-generation cephalosporin ceftriaxone has a long duration of action, with much of the drug excreted in the urine. Approximately 40% of the drug, however, is secreted in an unmetabolized form into bile, where its concentration reaches 100 to 200 times that of the concentration in plasma and exceeds its saturation level in bile. Once its saturation level is exceeded, ceftriaxone complexes with calcium to form insoluble salts, thereby resulting in formation of biliary sludge. Up to 43% of children who receive high doses of ceftriaxone (60 to 100 mg/kg/day) have been reported to form biliary sludge, and about 19% of these patients experience biliary symptoms. The sludge usually disappears after ceftriaxone is discontinued.
Epidemiologic investigations have shown that plasma HDL cholesterol levels are inversely correlated with the prevalence of cholesterol gallstones. By contrast, hypertriglyceridemia is positively associated with an increased prevalence of gallstones. These seemingly independent variables are actually interrelated because high plasma TG levels tend to increase with increasing body mass and are inversely correlated with plasma HDL levels. Interestingly, high plasma total and LDL cholesterol levels are not likely to be risk factors for the formation of gallstones.
Obesity is a well-known risk factor for cholelithiasis, and the prevalence of gallstone is rising with the worldwide obesity epidemic and the increasing incidence of insulin resistance. A large prospective study of obese women demonstrated a strong linear association between BMI and the prevalence of cholelithiasis. In this study, the risk of gallstones was 7-fold higher in women with the highest BMI (>45 kg/m 2 ) than in nonobese control women. Obesity is associated with increased hepatic secretion of cholesterol into bile, possibly because of higher enzymatic activity of HMG-CoA reductase and increased cholesterol synthesis in the liver. As a result, gallbladder bile is more lithogenic in obese than in nonobese persons, and a higher ratio of cholesterol to solubilizing lipids (bile acids and phospholipids) is observed in the former group. These alterations predispose to cholesterol crystallization and gallstone formation. Gallbladder motility is often impaired in obese persons, thereby promoting mucin secretion and accumulation, as well as cholesterol crystallization. The effect of pronucleating and antinucleating factors on cholesterol crystallization and gallstone formation in gallbladder bile warrants further investigation in obese and nonobese subjects.
Patients with diabetes mellitus have long been considered to be at increased risk of developing gallstones because hypertriglyceridemia and obesity are associated with diabetes mellitus and because gallbladder motility is often impaired in patients with diabetes mellitus. Proving that diabetes mellitus is an independent risk factor for gallstones has been difficult, however. Mice with hepatic insulin resistance induced by liver-specific disruption of the insulin receptor are markedly predisposed to formation of cholesterol gallstones. Hepatic insulin resistance promotes hepatic secretion of biliary cholesterol by increasing expression of the hepatic cholesterol transporters Abcg5 and Abcg8 through the forkhead transcription factor FoxO1 pathway. It also reduces expression of the bile salt synthetic enzymes, particularly oxysterol 7α-hydroxylase, thereby resulting in a lithogenic bile salt profile.
Disease or resection of the terminal ileum has been found to be a risk factor for gallstone formation. For example, intestinal bile salt absorption is often impaired in patients with Crohn disease, who are at increased risk of gallstones. The loss of specific bile salt transporters (e.g., ileal apical sodium-dependent bile acid transporter) in the terminal ileum may result in excessive bile salt excretion in feces and a diminished bile salt pool size, presumably with a consequent increase in the risk of cholesterol gallstones. These changes may also lead to formation of pigment gallstones because increased bile salt delivery to the colon enhances solubilization of unconjugated bilirubin, thereby increasing bilirubin concentrations in bile.
Spinal cord injuries are associated with a high prevalence of gallstones, which have been reported in some 31% of such patients, who have an annual rate of biliary complications of 2.2%. Although the complication rate associated with gallstones in patients with spinal cord injuries is at least 2-fold higher than the rate of gallstones in the general population, the relative risk is still low enough that prophylactic cholecystectomy is probably not justified. The mechanisms responsible for the association between spinal cord injuries and gallstone formation remain unclear. Gallbladder relaxation is impaired in these patients, but gallbladder contraction in response to a meal is normal. Therefore, the increased risk of gallstones is unlikely to be due to biliary stasis alone.
Both gallstone disease and NAFLD are highly prevalent in the general population and often co-exist in the same populations (see Chapter 87 ). These epidemiologic and clinical studies raise the possibility that both disorders could be casually related, similar risk factors influence the natural history of NAFLD and gallstone disease, or NAFLD is indeed an independent risk factor for cholesterol cholelithiasis. Although many clinical studies have investigated the association between NAFLD and gallstone disease, the results have been variable. The relationship among insulin resistance (evaluated with the homeostatic model assessment), liver fibrosis, NASH, and gallstone disease has been studied in morbidly obese patients with NAFLD before bariatric surgery. The prevalence of NASH is 18% in a morbid obese population with gallbladder disease. The third large U.S. National Health and Nutrition Examination Survey (NHANES) between 1988 and 1994 investigated 12,232 subjects by US and reported an association between gallstone disease, with a prevalence of 7.4% for gallstones and 5.6% for cholecystectomy, and NAFLD, with a prevalence of 20.0%. The prevalence of NAFLD was significantly higher in the group that underwent cholecystectomy (48.4%) and in the gallstone group (34.4%) than in the gallstone-free group (17.9%). These findings suggest that both conditions are tightly associated with metabolic disturbances such as obesity, insulin resistance, dyslipidemia, and the metabolic syndrome.
Celiac disease is a chronic, small intestinal, autoimmune enteropathy caused by an intolerance to dietary gluten in genetically predisposed individuals (see Chapter 107 ). Clinical studies have found that, because of defective CCK release from the proximal small intestine caused by enteropathy in patients with celiac disease before they start a gluten-free diet, gallbladder emptying in response to a fatty meal is impaired. Lack of CCK markedly enhances susceptibility to cholesterol gallstones via a mechanism involving dysmotility of both the gallbladder and the small intestine. Because a gluten-free diet can significantly improve celiac enteropathy, early diagnosis and therapy in celiac patients is crucial for preventing the long-term impact of CCK deficiency on biliary and intestinal function. When gluten is reintroduced in the diet, clinical and histologic relapse often occurs in patients with celiac disease. Moreover, some patients do not respond well to a gluten-free diet. Patients with celiac disease should routinely undergo US to determine whether gallbladder motility function is preserved and whether biliary sludge (a precursor to gallstones) is present in the gallbladder. Impaired intestinal CCK secretion is the link between celiac disease and cholesterol gallstone disease. Because neither epidemiologic investigations of gallstone prevalence rates in patients with celiac disease nor clinical studies of the impact of celiac disease on the pathogenesis of gallstones have been reported, whether celiac disease is an independent risk factor for gallstone disease remains largely unknown.
Use of statins has been associated with a decreased risk of gallstone disease in 2 large case-control studies. The first study compared 27,035 patients with gallstone disease who required cholecystectomy with 106,531 matched controls and showed a benefit to long-term statin use (>20 prescriptions filled and use of statins for >1.5 years) ; statin use was associated with a decreased risk of gallstone disease requiring cholecystectomy (adjusted odds ratio [OR], 0.64). Similar results were observed in a population study from Denmark of 32,494 patients with gallstone disease matched with 324,925 controls. The odds ratios of having gallstone disease in current and prior users of statins (>20 prescriptions filled) were 0.76 and 0.79, respectively, compared with controls.
The observation that deficiency of ascorbic acid (vitamin C) is associated with the development of gallstones in guinea pigs prompted investigation of the relationship between ascorbic acid levels and gallstones in humans. Serum ascorbic acid levels have been correlated with clinical or asymptomatic gallstones in 7042 women and 6088 men who were enrolled in the third NHANES. Among women, but not men, each standard deviation increase in serum ascorbic acid levels was associated with a 13% lower prevalence rate of clinical gallbladder disease.
In a 10-year follow-up of 46,000 male health professionals, subjects who consistently drank 2 to 3 cups of regular coffee per day were approximately 40% less likely to develop symptomatic gallstones. Drinking 4 or more cups per day was even more beneficial (relative risk 0.55), but there was no benefit to drinking decaffeinated coffee. A similar benefit to regular coffee was noted in a cohort study involving 81,000 women.
Cholesterol, phospholipids, and bile salts are the 3 major lipid species in bile, and bile pigments are minor solutes. Cholesterol accounts for up to 95% of the sterols in bile and gallstones; the remaining 5% of the sterols are cholesterol precursors and dietary sterols from plant and shellfish sources.
Concentrations of cholesteryl esters are negligible in bile and account for less than 0.02% of total sterols in gallstones. The major phospholipids are lecithins (phosphatidylcholines), which account for more than 95% of total phospholipids; the remainder consists of cephalins (phosphatidylethanolamines) and a trace amount of sphingomyelin. Phospholipids constitute 15% to 25% of total lipids in bile. Lecithins are insoluble amphiphilic molecules with a hydrophilic zwitterionic phosphocholine head group and hydrophobic tails that include 2 long fatty acyl chains. Biliary lecithins possess a saturated C-16 acyl chain in the sn -1 position and an unsaturated C-18 or C-20 acyl chain in the sn -2 position. The major molecular species of lecithins (with corresponding frequencies) in bile are 16:0 to 18:2 (40% to 60%), 16:0 to 18:1 (5% to 25%), 18:0 to 18:2 (1% to 16%), and 16:0 to 20:4 (1% to 10%). Lecithins are synthesized principally in the endoplasmic reticulum of the hepatocyte from diacylglycerols through the cytidine diphosphate-choline pathway. The common bile salts typically contain a steroid nucleus of 4 fused hydrocarbon rings with polar hydroxyl functions and an aliphatic side chain conjugated in amide linkage with glycine or taurine. In bile, more than 95% of bile salts are 5β,C-24 hydroxylated acidic steroids that are amide-linked to glycine or taurine in an approximate ratio of 3:1. Bile salts constitute approximately two thirds of the solute mass of normal human bile by weight. The hydrophilic (polar) areas of bile salts are the hydroxyl groups and conjugated side chain of either glycine or taurine, and the hydrophobic (nonpolar) area is the ringed steroid nucleus. Because they possess both hydrophilic and hydrophobic surfaces, bile salts are highly soluble, detergent-like, amphiphilic molecules. Their high aqueous solubility is due to their capacity to self-assemble into micelles when a critical micellar concentration is exceeded.
The primary bile salts are hepatic catabolic products of cholesterol and are composed of cholate (a trihydroxy bile salt) and chenodeoxycholate (a dihydroxy bile salt) (see Chapter 64 ). The secondary bile salts are derived from the primary bile salt species by the action of intestinal bacteria in the ileum and colon and include deoxycholate, ursodeoxycholate, and lithocholate. The most important of the conversion reactions is 7α-dehydroxylation of primary bile salts to produce deoxycholate from cholate and lithocholate from chenodoxycholate. Another important conversion reaction is the 7α-dehydrogenation of chenodeoxycholate to form 7α-oxo-lithocholate. This bile salt does not accumulate in bile but is metabolized by hepatic or bacterial reduction to form the tertiary bile salt chenodeoxycholate (mainly in the liver) or its 7β-epimer ursodeoxycholate (primarily by bacteria in the colon).
Bile pigments are minor solutes and are formed as a metabolic product of certain porphyrins. They account for roughly 0.5% of total lipids in bile by weight. They are mainly bilirubin conjugates with traces of porphyrins and unconjugated bilirubin. Bilirubin can be conjugated with a molecule of glucuronic acid, which makes it soluble in water. In human bile, bilirubin monoglucuronides and diglucuronides are the major bile pigments. Other bile pigments are monoconjugates and diconjugates of xylose, glucose, and glucuronic acid and various homoconjugates and heteroconjugates of them.
Proteins and inorganic salts are also found in bile. Albumin appears to be the most abundant protein in bile, followed by immunoglobulins G and M, apolipoproteins AI, AII, B, CI, and CII, transferrin, and α 2 -macroglobin. Other proteins that have been identified but not quantitated in bile include EGF, insulin, haptoglobin, CCK, lysosomal hydrolase, and amylase. Inorganic salts detected in bile include sodium, phosphorus, potassium, calcium, copper, zinc, iron, manganese, molybdenum, magnesium, and strontium.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here