Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Whereas in the past, reconstructive microsurgery mainly consisted of defect coverage by free tissue transfer, today this technique allows a continual integration of improved aesthetic appearance and functional reconstruction.
Thus, the main goal of functional reconstructive surgery is to optimally address both functional and aesthetic requirements. Sophistication in surgical techniques has enabled the surgeon to address a wide variety of individual exigencies with one or more operations. In this respect, free and local functional muscle transfer has proven to be a valuable reconstructive procedure in patients with substantial defects and loss of function in various locations, including the extremities, abdominal wall, or facial musculature. The gracilis, latissimus dorsi, and gastrocnemius are the muscles most commonly used for functional muscle transplantation.
In cases of combined tissue deficiency and functional impairment, where local repair or tendon transfer and/or nerve grafting are not practicable due to extent of the trauma, free functional muscle transplantation will be the treatment of choice. Several previous studies have confirmed the applicability of this concept.
As with all tissue transfers, the principle of replacing like with like while minimizing donor site morbidity should be adhered to. Specifically, muscle type, blood supply, innervation, volume, excursion, contractility, and expendability need to be taken into consideration when choosing a donor for free microvascular transfer.
Basic functions of skeletal muscles include maintenance of posture, joint stabilization, and active motion. A wide variety of muscles are available for functional muscle transfer, each of which has distinctive characteristics regarding its size, shape, and strength.
Generally, there are two main types of muscles, which differ in their anatomic structure and mechanism of contraction: parallel (strap) and pennate muscles. In parallel muscles, fascicles are arranged in line with the axis of the muscle. During contraction, these muscles shorten to about 50% of their original length and diameter increases; they show moderate strength, but are able to contract over long distances. Examples include the gracilis, serratus, pectoralis, sartorius muscles, and others. In pennate muscles, fascicles attach in an oblique angle (pennation angle) in relation to its tendon. When these muscles contract, the pennation angle increases. They have different lengths of muscle fibers originating from the tendinous part of the muscle. Compared with strap muscles, pennate muscle fibers have less range of excursion and can only shorten by about 25%, but demonstrate significantly more power on contraction. Examples include biceps femoris, soleus, gastrocnemius muscles, and others.
These specific muscle characteristics need to be remembered when choosing a muscle for functional reconstruction. For instance, if a patient requires a large range of motion, as in forearm reconstruction, the surgeon should select a strap muscle. If a patient requires more strength than range of motion, for example, for reconstruction of a lower extremity muscle, a pennate muscle should be selected.
Another critical surgical principle in functional muscle transfer is to restore the resting muscle tension. Efficiency of a skeletal muscle contraction largely depends on its state of tension as it is stretched between insertion and origin. Shortening of muscle fibers results in a functional reduction of contraction force. Since a muscle shows its maximum potential for contraction when it is almost fully stretched, adequate adjustment of tension on inset of the muscle is important in order to obtain maximum strength. Resting tension and range of contraction must be marked with a suture or similar in situ before the muscle is detached at its origin or insertion. This resting tension must be adjusted precisely on muscle inset in order to supply sufficient resting tension, while at the same time providing an optimal range of motion, depending on the individual functional requirements of the recipient site. Therefore, muscle selection must be targeted to optimally meet these functional requirements.
The necessity of meticulously precise technique regarding the neurovascular anastomoses cannot be overemphasized, since this is the key step to ensure survival of the muscle. Ischemia time is a critical factor to ensure functional muscle recovery. Revascularization of the transplanted muscle has to be achieved within a maximal time frame of 3 h. Beyond this time, ischemia negatively affects flap survival and function.
Nerve coaptation requires viable motor fascicles at the recipient site to innervate the transferred muscle. As in vascular anastomosis, meticulous microsurgical nerve coaptation is essential. The nerve coaptation site should be placed as close as possible to the neuromuscular junction of the transferred muscle, in order to provide a minimal distance for nerve regeneration and to avoid a long period of muscle denervation.
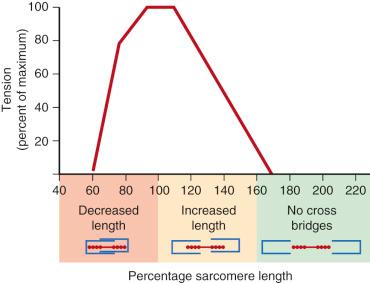
Precise adjustment of muscle resting tension before and after muscle transplantation is another key principle in functional muscle reconstruction. Actin and myosin filaments must be optimally aligned in order to exert maximum strength. Muscle sarcomeres produce maximum force when they contract from between 80% and 120% of their resting length ( Fig. 23.1 ). The patient must be prepped and draped in a fashion that allows full range of motion of the muscle to be transferred. Prior to detachment, the muscle is adjusted to optimal tension within the above-mentioned range prior to placing the marking sutures. The author utilizes a technique in which the muscle is segmentally marked with a Prolene suture every 2 cm for transfer of shorter muscle portions (i.e., gracilis muscle for lower lip reconstruction) and 5 cm for transfer of longer muscles (i.e., latissimus dorsi muscle) prior to detachment. On transplantation, the muscle is inset accordingly. This guarantees optimal force and range of contraction following reinnervation.
While a large number of muscle transfers have been described in the literature, in this chapter we will mostly focus on established flaps for novel functional indications as originally introduced by Ninković et al. As such, harvest of the flaps will not be elaborated on here, but the focus will lie on appropriate patient selection, pearls regarding the inset of the flaps, as well as discussion of expected outcomes and possible complications.
Specifically, we will describe four novel indications for functional muscle transfers:
Functional lower lip reconstruction utilizing the free innervated gracilis muscle
Functional abdominal wall reconstruction utilizing the innervated latissimus dorsi muscle
Functional bladder detrusor myoplasty utilizing the free innervated latissimus dorsi muscle (LDDM)
Neuromusculotendinous gastrocnemius muscle transfer for the treatment of drop foot.
The lips are highly visible structures on the face and serve important and diverse functions, such as articulation, mastication, oral competence, and expression of emotion. The lips are also particularly expressive facial features and convey emotional and sexual connotations. After the eyes, the lips may be the second most important organs of attraction, infatuation, fascination, and imagination for the opposite sex. The shape, thickness, formation, composition, and texture of lips play pivotal roles in the overall beauty of a human face.
The principal function of the lips is oral competence, which contributes to deglutition and word articulation. The sphincter muscle, the orbicularis oris, provides this competence, together with a supporting cast of paired elevators and depressors. The unreplaced loss of a significant segment of orbicularis muscle precludes competence. Ideally, the reconstructed lip should be sensate to retain the sphincter function; to oppose vermilion to vermilion of the upper lip in a watertight continent seal; and to allow a sufficient opening for food and dentures; and finally it should have an acceptable aesthetic appearance. On some occasions, particularly in subtotal and total lip loss, not all these criteria can be satisfied completely with conventional reconstructive techniques. However, one should avoid the postoperative result of a tight, inverted lower lip that disappears beneath the curtain of the upper lip when the mouth closes.
The classic guidelines of lower lip reconstruction include repair utilizing local tissues of similar color and texture, as well as the concept of entire subunit reconstruction, introduced as a fundamental principle to achieve optimal aesthetic results. Subdividing the lips into aesthetic subunits can prove to be very beneficial when planning reconstructive procedures. The lower lip should be considered a single aesthetic unit, while the upper lip can be divided into two lateral, and one median (philtrum) subunit. Lower lip reconstruction is functionally more important because oral competence depends greatly on a functional lower lip, with good muscular tone and adequate height and sensation.
When reconstructing the lips, it is important to save or restore the muscular modiolus and to preserve the orientation of this symmetric structure in order to achieve good functional results, as the modiolus is the site of insertion for the oral sphincter musculature.
The ultimate reconstructive goal is both aesthetic and functional, leading to a near normal appearance and functional recovery.
In the literature, several procedures have been reported for reconstruction of large defects (>75%) of the lips. The lower lip can be reconstructed using local flaps (e.g., cheek advancement flaps, rotation or nasolabial, regional pedicled flaps, and free flaps.
In our opinion, local flaps can provide good aesthetic results, especially in elderly people with skin and tissue laxity. Regarding the functional results and potential restoration of sensitivity, some doubts exist. Using local tissues for reconstruction, the lower lip is usually tight with a bulky upper lip, and a large amount of healthy tissue in the nasolabial and chin–labial area has to be sacrificed for reconstruction. At present, there is no universally accepted gold standard for subtotal or total reconstruction of the lower lip, especially if adjacent chin tissue is included in the resection.
Other techniques, such as the Karapandzic and modified Gillies's fan flaps, may preserve orbicularis function and lip sensation, but they change the position of the oral commissure. Jackson recommended this technique especially in subtotal (up to three-quarters) reconstruction of the lower lip. Microstomia often results, even if significant problems are rarely reported. Total lower lip reconstruction is also possible using an extended Karapandzic flap, but with this procedure microstomia results are even more frequent, requiring additional Abbé flaps and commissuroplasties. Considering regional flaps, such as the sternocleidomastoideus or deltopectoral flaps, these flaps appear very voluminous, without capacity to contract, and require a two-stage procedure. They cause bulkiness on the neck and an unpleasant appearance of the donor sites.
Finally, free flaps may provide impressive results in head and neck reconstruction, especially when used for large defects. The main advantages of a free flap are that the residual tissues are well preserved and the surgeon does not need to be concerned about the total amount of the initial tissue resection. The flap most often performed for total lip reconstruction remains the radial forearm flap. Good aesthetic and functional results have been reported using this flap. However, the radial forearm flap does not have its own motility, and the color and texture match is not perfect. In an effort to improve motility and symmetry, different technical solutions such as using palmaris longus tendon and looping it around the modiolus have been attempted. However, even these refinements are unable to provide spontaneous symmetrical lower lip movement. Finally, donor site morbidity is not inconsiderable. Given the first author's experience in functional muscle transfer, we considered an innervated gracilis muscle as the ideal flap for lip reconstruction.
In the literature, the gracilis muscle has been reported in reconstructive surgery for the repair of different types of defects: facial palsy, total tongue reconstruction, muscle replacement in the upper limb, and several soft tissue repairs. The presented approach is the first on subtotal and total reconstruction of the lips using a gracilis muscle. The combination of this flap with the Pribaz facial artery musculomucosal flap and sensitive neurotization, is a new concept.
In the case of subtotal resection of the lip, our technique allows maintaining the symmetry of the mouth, avoiding distortion of the residual commissure and sparing all facial tissues around the lip defect. This characteristic is of advantage when a part of the cheek also has to be removed during resection of a larger tumor; in fact, it is not advisable to use cheek advancement flaps in such a case. In total lip reconstruction, the gracilis muscle can restore the oral sphincter completely, with symmetry of the mouth and normal opening.
The use of a facial artery musculomucosal flap was used to reconstruct the inner surface of the gracilis muscle and to achieve a natural looking vermilion, given appropriate amounts of available mucosa and the good length and mobility of its pedicle; it is an axial flap, consisting of mucosa, submucosa, a small amount of buccinator muscle, the deeper plane of the orbicularis oris muscle, and the facial artery and its venous plexus. The facial artery musculomucosal flap has the advantage of being a single-stage procedure, as compared with tongue flaps and cross-lip flaps, which require secondary division.
We have thus employed the free innervated gracilis flap when faced with extensive soft tissue defects of the lips.
The appropriate patient should, in case of malignancy, have undergone staging as well as a pathologically confirmed R0 resection prior to any reconstructive effort. In suitable patients, tumor resection, trauma, or congenital vascular malformations must affect full-thickness tissue of at least 75% of the lower lip.
In cases of non-malignant lesions, a second team harvests a gracilis muscle free flap in standard fashion simultaneously during resection of the lip lesion. The average vascular pedicle length of the gracilis is approximately 6 cm, the branch of the obturator nerve to the muscle is usually at least of equal length.
The pedicle is divided after completing the dissection of the recipient vessels at the neck, usually the facial artery and vein. The pedicle should be kept long enough to reach the superior thyroid vessels in the event of very extensive resection of the perioral tissue. To perform a functional muscle transfer, care needs to be taken to identify and spare the ipsilateral marginal branch of the facial nerve during the resection. This nerve should be left as long as possible, and the obturator nerve shortened as much as possible, in order to minimize the length necessary for nerve regrowth and hence, the time necessary for muscle reinnervation. This basic principle holds true for all functional muscle flaps described in this chapter. Additionally, if it is possible, the mental branch of the trigeminal nerve has to be spared and prepared at the end to be inserted into the gracilis muscle, in an attempt to achieve neurotization of this muscle and recovery of sensation.
The required length of the orbicularis muscle to be reconstructed is equal to the length of the lip during maximal stretch, and should be measured prior to resection. In cases of extensive tumor or vascular malformation involvement or traumatic muscle loss, one cannot but give reference to the unaffected contralateral side and use one's own judgment. It is important, however, that whatever needed length determined, is transposed to the gracilis muscle and the appropriate length and tension marked with sutures prior to harvesting. For the gracilis muscle, optimal tension is achieved by placing the leg in a 45° abducted and 45° hip flexed position. Again, this is a technical principle of resting muscle tension, which should be adhered to in all cases of functional muscle transfers.
The gracilis muscle flap is then harvested and trimmed to the required dimensions of width and length under microscopic magnification on the back-table. In order to thin and tailor the muscle flap, the perimysium should be split longitudinally while sparing the neurovascular supply, which usually runs perpendicular to the muscle fibers. This also helps to decrease bleeding after muscle reperfusion. In doing so, one can shape the muscle nicely while sparing neurovascular structures of the muscle subunits.
Simultaneously, a facial artery musculomucosal (FAMM) flap is prepared to reconstruct the vermilion and the inner mucosa of the gracilis flap. Pribaz et al. showed that the facial artery musculomucosal flap can be inferiorly or superiorly pedicled. In all our cases, the recipient vessels were the facial artery and vein, combined with a superiorly pedicled facial artery musculomucosal flap. In case one FAMM flap is not enough for full inner lining reconstruction, a combination of a superior and inferior pedicled facial artery musculomucosal flap can be utilized from both sides for appropriate vermilion reconstruction. If the FAMM flap is not usable due to defect dimensions following radical resection, a submental pedicled flap can be used as an alternative for inner lining. At the final stage of the procedure, the gracilis muscle is covered with unmeshed split-thickness or full-thickness skin from an area with optimal color match for the lip, such as the scalp or the supraclavicular region.
The gracilis flap is inset using 2-0 Vicryl sutures, taking into account the aforementioned muscle resting tension length. The muscle edges should be sutured to solid structures, such as the remaining orbicularis oris or buccinator muscle. In cases when the oral commissure is involved, the gracilis has to be split, sutured to the residual opposite orbicularis muscle, and then passed through and looped around the residual commissural fibers at the level of the original commissure in order to reconstruct a new oral sphincter.
The vascular pedicle of the flap is anastomosed to the recipient vessels, subsequently the marginal branch of the facial nerve is coapted to the obturator and finally to the mental nerve to restore sensation.
Patients should be anticoagulated according to standard protocol (low-molecular heparin) and wear compression stockings at all times until full ambulation. No specific anticoagulation is indicated with respect to the microvascular free tissue transfer. The donor site is closed with a Jackson-Pratt drain in place, which can be removed once output is less than 30 cc/day.
The patients are instructed to minimize movement of the affected area by means of speech or food intake for 3–5 days. After take of the skin graft is confirmed, approximately 1 week after surgery, motion can be liberated and a simple chin strap compressive dressing with additional support to the lower face is applied. This chin strap is worn for 24 h until muscle swelling has completely diminished. The purpose of this suspension is to avoid an inverted lip deformity. We generally suggest the patient continues to wear the suspension garment whenever possible but at least during the night, until functional muscle recovery. The rehabilitation program is started within 3 weeks of the operation to reestablish voluntary active labial movement. An electromyographic study is performed every 3 months during the first year after surgery, to evaluate recovery of motor innervation, in addition to the scheduled physical examination of the patients. The sensory examination includes a touch-pressure sensation test using the Semmes–Weinstein monofilament test; a hot-and-cold discrimination test; and a static 2-point discrimination test.
Besides common surgical complications (bleeding, infection, dehiscence, hematoma/seroma formation), complications specifically related to this operation may include oral incontinence with subsequent development of drooling; persistent edema of the flap; poor reinnervation with insufficient regain of motion and/or sensation; contour irregularities; poor skin color match; poor speech; and partial or full flap loss.
To date we have applied the technique in a total of 10 patients.
There were no partial or full flap losses, but partial loss of skin grafts occurred in two patients, requiring secondary skin grafting. Most patients are expected to have a period of 1–2 weeks of drooling during the time of maximal tissue swelling. However, none of our patients suffered persistent drooling in the long-term follow-up. Presently, all our patients show no drooling or problems with word articulation, mouth opening, or eating. Oral continence was near perfect, without any air leakage during puffing, and the oral sphincter function had been completely restored in all patients. Two patients among the 10 are even able to whistle.
Motoric reinnervation of the muscle flap can be expected to occur at approximately 1 mm/day and can therefore usually be expected around 3–6 months postoperatively. All our patients showed full reinnervation at 1-year follow-up, as evidenced by regain of motion including oral competence, speech, and puckering of the lips.
While requiring up to 1 year, sensation was ultimately regained in all cases, as confirmed with Semmes–Weinstein monofilament tests. Patients should be counseled that secondary surgeries (debulking, scar corrections, gracilis muscle reinsertion, commissure corrections, etc.) may become necessary in approximately 50% of cases. These procedures can be carried out under local anesthesia in an outpatient setting. In our series, both surgeons and patients were ultimately satisfied with the functional and aesthetic results.
Luce observed, in 1995, that the reconstructed lower lip often resulted in an immobile, insensate block of tissue that, in the best of circumstances, serves as a dam rather than an effective and dynamic structure. To effectively reconstruct the lower lip, one must provide not only skin and mucosa, but also a functioning mimetic muscle.
In our opinion, the functional gracilis fulfills all these requirements; it allows for near normal motion in all portions of the reconstructed lips. The new commissure is symmetric and moves simultaneously with the residual commissure due to the innervation by the facial nerve. Furthermore, all our patients regained sensitivity of the reconstructed lips. Regarding the recovered lip sensation, we cannot be sure that it is a consequence of the neurotization of the gracilis via the stump of the mental nerve, or if it is caused by using the facial artery musculomucosal flap; probably both play a role for recovery of sensitivity. Neurotization has been well described experimentally and clinically for motor nerves, but we are not aware of any publications on the neurotization of sensitive nerves. The regaining of sensation in the case of a flap transposed into the oral cavity has already been studied; the most probable explanation considers the large area dedicated to mouth sensitivity in the brain homunculus. There are also many sensitive receptors in the mouth mucosa, which may promote migration of the sensitive fibers into the flap.
The goal of a reconstructive procedure should be an optimal functional and aesthetic result, with minimal donor site morbidity. According to the reconstructive requirements of lower lip reconstruction, local flaps seem to be the best option in elderly patients with limited size full-thickness defects. However, extensive local flaps may be unsuitable when a total lower lip resection is performed, especially in young patients who do not have enough laxity of tissue and who could be discouraged by multiple perioral scars. We believe that our technique using an innervated gracilis free flap, combined with a superior pedicled facial artery musculomucosal flap and skin grafting, allows for very good functional and aesthetic reconstruction of the lower lip, restoring dynamic, spontaneous, and voluntarily controlled lower lip movement and good appearance, achieved with just one surgical procedure and minimal donor site morbidity.
Full-thickness abdominal wall defects constitute a particular challenge in reconstructive surgery. A distinction must be made between partial abdominal wall weakness, limited to the fascia but with sufficient soft tissue coverage, and full-thickness defects, requiring restoration of functional strength and stabilization, as well as adequate soft tissue coverage. Established methods to stabilize abdominal wall defects include utilization of artificial mesh and acellular dermal matrices, component separation, fascia lata allografts, as well as pedicled and free flaps. While fascial defects in cases of hernias can in general be adequately treated using synthetic mesh or other matrices, full-thickness defects including fascia, muscle, and skin require more complex treatment. An ideal reconstruction must provide functional strength and stabilization, while at the same time leading to an acceptable aesthetic appearance. Current options for full-thickness abdominal wall reconstruction include local myo- and myocutaneous flaps from the adjacent abdomen, pedicled and free fascia lata flaps, rectus femoris, and sartorius flaps.
Here, we describe utilizing the free latissimus dorsi flap as a means of restoring both functional stability as well as aesthetic appearance.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here