Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
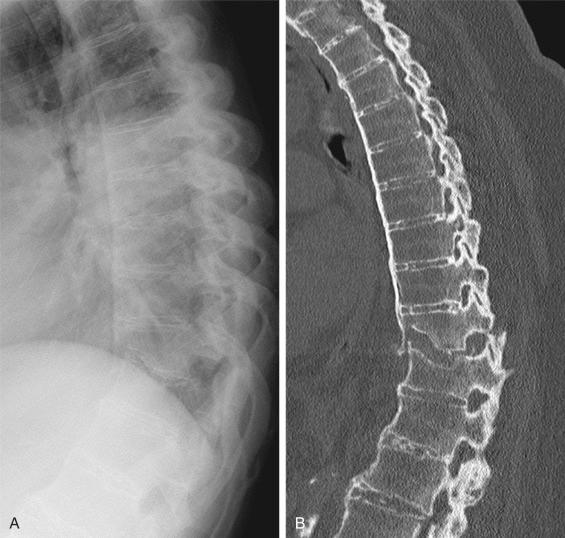
In general, nonosteoporotic spinal fractures are the result of high-impact trauma and may be associated with spinal cord injuries. However, trauma physicians should be extra aware of the ankylotic spine because stiff ankylotic spines can fracture with lower forces, are associated with a fourfold increased risk for fractures, and have a high risk up to 58% of spinal cord injury, and the fractures can be subtle on imaging ( Figs. 34.1 to 34.4 ). Fractures of the ankylosed spine are more often associated with a hyperextension pattern, similar to a long bone fracture, in comparison to the nonankylosed spine (45.5% to 64.3% vs. 11.8%) and with greater spinal instability, a higher risk of spinal cord injury, and more complications. The majority of fractures in ankylotic spines show the unstable type B3 (hyperextension) or type C (displacement) configurations according to the AOSpine classification. Therefore knowledge in this field combined with a high level of clinical suspicion is essential to optimally manage trauma in this growing group of patients.
Fracture risk is increased in patients with an ankylosed spinal column.
Ankylosing spondylitis (AS) and diffuse idiopathic skeletal hyperostosis (DISH) are the two main conditions causing spinal ankylosis.
Clinical suspicion should be high even after low-energy trauma because fractures of the ankylosed spine can be subtle on imaging.
A patient with an ankylotic spine and pain after even relatively minor trauma should be considered to have an unstable spinal fracture until proven otherwise.
Percutaneous stabilization using a long pedicle-screw construct is the preferred treatment of an unstable fracture without neurologic impairment in the ankylosed thoracic or lumbar spine.

![Fig. 34.3, Sagittal reconstruction of computed tomography (CT) and magnetic resonance imaging (MRI) scan of the cervical spine of the same male patient as Figs. 34.1 and 34.2 at the age of 74 years. The patient was admitted to a hospital abroad after a fall from a standing position and was discharged after a CT was obtained and no fractures had been observed. Neurologic deficit (American Spinal Injury Association [ASIA] classification D) started to develop a week after the initial trauma, and 12 days later, a new CT was acquired (A) showing a fracture of C5. The diagnosis of an unstable type B3 fracture of C5 was confirmed by MRI scan (B; T2 weighted), and HALO stabilization was applied in anticipation of surgery. Fig. 34.3, Sagittal reconstruction of computed tomography (CT) and magnetic resonance imaging (MRI) scan of the cervical spine of the same male patient as Figs. 34.1 and 34.2 at the age of 74 years. The patient was admitted to a hospital abroad after a fall from a standing position and was discharged after a CT was obtained and no fractures had been observed. Neurologic deficit (American Spinal Injury Association [ASIA] classification D) started to develop a week after the initial trauma, and 12 days later, a new CT was acquired (A) showing a fracture of C5. The diagnosis of an unstable type B3 fracture of C5 was confirmed by MRI scan (B; T2 weighted), and HALO stabilization was applied in anticipation of surgery.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/FracturesintheAnkylosedSpine/2_3s20B9780323611145000343.jpg)
![Fig. 34.4, Lateral conventional radiograph of the same patient as in Figs. 34.1 to 34.3 showing the cervical spine 7 weeks after the initial trauma and 5 weeks after open stabilization from C3 to C7. The neurologic deficit improved after the surgery (American Spinal Injury Association [ASIA] classification E). Fig. 34.4, Lateral conventional radiograph of the same patient as in Figs. 34.1 to 34.3 showing the cervical spine 7 weeks after the initial trauma and 5 weeks after open stabilization from C3 to C7. The neurologic deficit improved after the surgery (American Spinal Injury Association [ASIA] classification E).](https://storage.googleapis.com/dl.dentistrykey.com/clinical/FracturesintheAnkylosedSpine/3_3s20B9780323611145000343.jpg)
The majority of cases of spinal ankylosis are the result of ankylosing spondylitis (AS) or diffuse idiopathic skeletal hyperostosis (DISH). AS is an inflammatory rheumatic disease affecting the axial skeleton, with occasional peripheral, mainly lower-limb, arthritis. This condition is a major subgroup of the spondyloarthritides, and the prevalence of AS ranges between 0.1% and 1.4% depending on the classification criteria used and ethnic background of the studied population. About 80% of patients with AS develop their first symptoms at an age of less than 30 years; there also appears to be a correlation between younger age of onset and worse clinical outcome. The most important clinical features are back pain and spinal stiffness caused by inflammation and/or structural damage of the spine. Diagnosis of AS is generally done using the modified New York criteria. These criteria require the presence of at least one clinical symptom (back pain, lumbar stiffness, or limited chest expansion) plus a radiologic criterion (sacroiliitis grade ≥ 2 bilaterally or grade 3 to 4 unilaterally). The fundamental pathogenetic mechanism driving the development of AS is poorly understood. A strong genetic link is, however, found between the presence of the major histocompatibility complex (MHC) class I molecule HLA-B27 and the presence of AS. About 90% of European Caucasians and 50% of African Americans with AS are positive for HLA-B27, compared with about 8% of the general population of European Caucasians and 2% to 4% of African Americans. Treatment options for AS are tumor necrosis factor-α blockers to reduce disease activity and improved physical function.
DISH is a growing and much more common contributor to spinal ankylosis than AS. DISH is characterized by the development of bone bridges at the anterolateral location of the vertebral body. Ossification at the location of entheses of the peripheral skeleton may also be present, for example, at the elbows, wrists, ankles, and shoulders. The prevalence of DISH is reported at between 2.9% and 42.0% depending on the classification criteria used and the risk factors in the studied population. The presence of DISH is associated with old age, obesity, hypertension, and diabetes mellitus. Clinical symptoms in patients with DISH can include back pain, spinal stiffness, dysphagia, airway obstruction, and lowered lung capacity. Most patients are unaware of the presence of DISH because of the lack of (severe) symptoms, and as a consequence, clinicians are seldom aware of the increased risks it presents in cases of spinal fracture. The most frequently applied criteria used to diagnose DISH, described by Resnick and Niwayama, consist of the presence of flowing ossification along the anterolateral aspect of at least four adjacent vertebral bodies and relative preservation of the intervertebral disk in the absence of bony ankylosis of the apophyseal or sacroiliac joints. The pathogenesis of DISH is unknown. Genetic, metabolic, vascular, and mechanical factors and signaling pathways, such as Wnt, NFκB, BMP2, PGI2, and endothelin 1, have all been suggested as potential elements promoting DISH bone formation. The treatment of patients with DISH is limited to symptomatic relief (analgesics, nonsteroidal antiinflammatory drugs [NSAIDs]) or preventive care to avert complications (e.g., precautions during endotracheal intubation).
AS and DISH are often described as two different conditions, but co-occurrences have been described in the literature. For both conditions, the resultant spinal stiffness is likely more important to the increased fracture risk and the ensuing unstable fracture patterns than the underlying cause. Spinal ankylosis predisposes to spinal fracture, with the prevalence of AS in a cohort with traumatic spinal injury of 8.5% (14/165 patients) and the prevalence of DISH of 24.2% (40/165 patients). The increasing prevalence of DISH among the elderly (up to 56% in males over 80 years old) may contribute to the increasing incidence of traumatic spinal cord injuries among elderly patients (84 to 131 cases/million in 1993 to 2012) accompanied by an increase in in-hospital mortality. In patients with over 42 years of disease duration of AS, the prevalence of a spinal fracture rises to 14% (15/107 patients) compared with an overall prevalence of 5.7% (990/17,297 patients). This expected increase of ankylotic spine fractures should be addressed in the clinical environment by improving the knowledge of clinicians of ankylotic spinal conditions.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here