Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
About Dance Smart
Balance – Airplane Test
Function – Battement Développé
Function – Over Turn Out 1st to 5th
Function – Dance and Street Shoe
Function – Petit Jeté
ROM – Neural Mobility: Straight Leg Raise with Dorsiflexion
Function – Yard Stick Test
Function – 4th Pirouette en Dehors
Balance – Plié, Relevé, Passé
Function – Plié
ROM – Beighton Laxity Scale
ROM – Hip Rotation
Function – Sauté Test
Stability – Hip: Penguin, Pigeon
Stability – Toes
Stability – Core: Pelvis and Spine
Function – Tendu
Alignment – Hip and Knee. Femoral or Tibeal Torsion
Gait – Triple Hop Test
Alignment – Observation: Anterior, Lateral, Posterior Views
Stability – Hip: Perturbations
ROM – Full Body Rotation
ROM – Plantarflexion, Dorsiflexion
ROM – Inversion, Eversion, Navicular Drop
ROM – Toe Flexion, Extension, Doming, Abduction
Balance – Shift Weight to One Leg
Gait – Landing Error Score System
Gait – Jump
Function – Demi Pointe and Pointe
Ballet has all the elements of the arts in its makeup—drama, poetry, literature, painting, sculpture, design, music, and, of course, dance. Dancers, both male and female, are the physical means by which the choreographer sculpts a composition of expressive motion. The grace and art of the ballet performance belie the great physical strain on the body as a whole and the foot and ankle in particular. From an early age the dancer must learn to be an artist, a gymnast, and an athlete. Most ballet dancers train for a minimum of 10 years before attaining the skill set necessary to join a corps de ballet. Very few dancers develop into soloists and fewer still attain the role of principle ballerina. Throughout this time of training, the body is placed under great strain, and it is by a process of natural selection that those dancers who are flexible and technically proficient survive the rigors of training to advance further. Hamstring strains, foot and ankle pathologies, and low back pain are the most commonly diagnosed musculoskeletal injuries.
Female dancers spend a considerable time en pointe , or on the points of the toes ( Fig. 24.1 ), whereas male dancers do not dance on their toes and spend much of their time in turning, lifting, and holding female dancers. As such, male and female dancers tend to present with distinct injuries. In addition to the myriad of physical injuries related to female dancers that follows, female dancers also are prone to the triad of anorexia, amenorrhea, and osteoporosis (see Chapters 4 and 28 ). This unfortunate triad stems from the significant pressure on dancers to weigh less and less. The most disturbing data suggest that female dancers weigh more than 15% below the ideal weight for height. This has metabolic consequences leading to stress fractures and slower union rates in injured female dancers. In contradistinction, male dancers have fewer metabolic problems but are prone to overuse injuries from repetitive motion and to stress fractures (see Chapter 3 ) from the sudden deceleration of large leaps, volé , sauté , or jeté . Dancers’ feet are the instruments on which their art depends. They require, in addition to an extraordinary flexibility and strength, a particular anatomic profile.
Over time a dancer’s foot will evolve and only the strongest will survive. Dancers’ feet typically are ‘‘intrinsic plus:’’ they have narrow metatarsal width with straight toes. (Intrinsic-minus feet have wider metatarsal splaying and clawing of the toes.) Apart from muscle strength, dancers’ feet require great flexibility. In the relevé position ( Fig. 24.2 ) the ankle is in a vertical position: 90 degrees of plantarflexion of the ankle-foot complex. The dancer also requires 90 to 100 degrees of dorsiflexion in the first metatarsophalangeal (MTP) joint to go from relevé to en pointe . These are extraordinary ranges of motion and can only be achieved with years of practice, which mold the young ballet dancer’s bones during the bone growth phase. As a result of endless practice barres, classes, and training, dancers’ feet tend to be cavus and have thickened metatarsals to support when en demi-pointe . Calluses abound secondary to pressure demands on the skin.

In general, five types of dancer’s feet have been described:
Grecian (also known as Morton) foot has a relatively long second and third metatarsal in relation to the first and fifth metatarsal. However, dancers do not have the same problems associated with transfer metatarsalgia as does the general population with this foot configuration.
Egyptian foot. Long first ray relative to the central metatarsals. This can predispose the first MTP joint to degenerative arthrosis or hallux rigidus.
Simian foot. Metatarsus primovarus with hypermobile first ray that causes transfer metatarsalgia to central metatarsal heads.
Peasant foot. Uniform metatarsal length, giving broad, square foot. Its stability makes it an ideal platform for dancing.
Model’s foot. This foot is long and slender with a taper exaggerated cascade from first to fifth metatarsal head. As such, it bears weight unevenly on demi-pointe and is a poor foot for dance.
The following is a review of the more common dance injuries and problems in the foot and ankle.
Although dancing has been said to play a role in the pathogenesis of bunions, it is unlikely that this is the case. Dancers, like the rest of the population, can be either resistant or prone to develop bunions. In those dancers that are prone to develop bunions, it is imperative to delay surgical intervention for as long as possible. Bunion surgery adversely affects dorsiflexion of the first MTP joint, a critical motion in dancers. Most bunions, specially the asymptomatic ones, can be treated with conservative methods, including toe spacers and horseshoe pads ( Fig. 24.3 ). The senior author has seen several aspiring young dancers whose careers were ended by well-meaning bunion surgery. If a bunion is precluding the dancer from activity and surgery is warranted, then a chevron or metatarsal osteotomy can provide pain relief and stability without compromising motion. A tarsometatarsal fusion will make the midfoot too stiff and limit the pointe position.

Any restriction to full dorsiflexion of the first MTP joint will prevent the dancer from performing relevé . Many dancers can accommodate by rolling out onto the lateral border of the foot, a process known as ‘‘sickling.’’
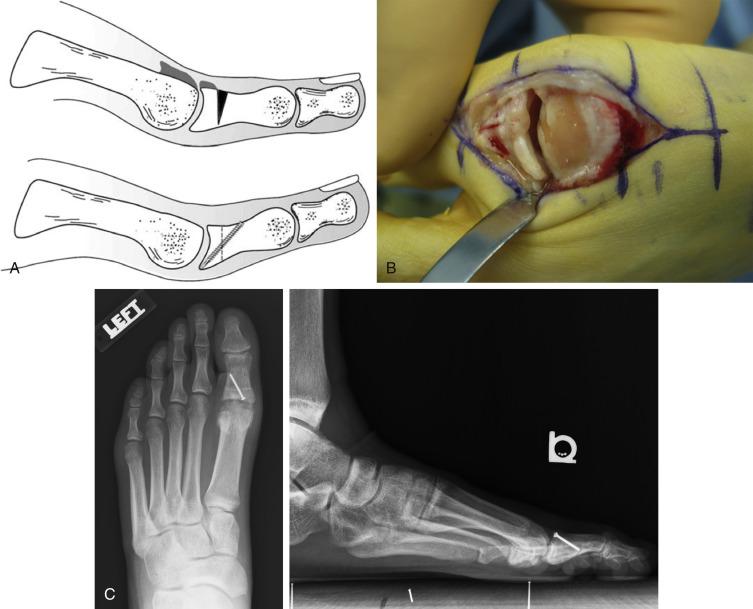
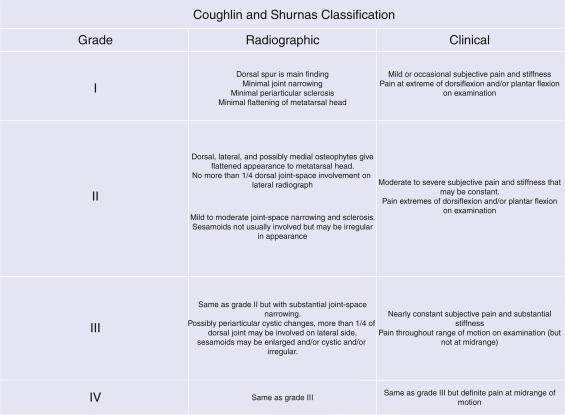
The treatment of hallux rigidus depends on the grade of the disease ( Fig. 24.4 ). A frequently used classification system was proposed by Coughlin and Shurnas ( Fig. 24.5 ) :
In grade I disease, the joint is preserved and marginal osteophytes can be resected (cheilectomy), either arthroscopically or open dorsal approach, with excellent outcomes.
In grade II disease, the joint is involved. There is minor cartilage destruction evident as joint space narrowing on plain radiograph, especially in its dorsal aspect. Surgical treatment involves a more extensive surgical debridement with cheilectomy and resection of the dorsal one-third of the metatarsal head. Intraoperative dorsiflexion of the hallux greatly overestimates the degree of motion that can be expected following surgery. Just over half of what is achieved at the time of surgery will be evident in the postoperative follow-up examination. It is important that dancers understand that, although surgery will make the condition better, the joint will never be normal. In addition, the length of recovery time must be discussed with the dancer, because a full functional recovery often takes 6 months. To improve functional motion following surgery, a dorsally based closing osteotomy (Moberg) can be used. This procedure improves dorsiflexion but at the expense of plantarflexion, and the dancer should be warned of this.
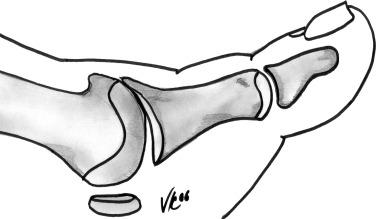
Grades III and IV hallux rigidus presents with dorsal and lateral osteophytes in addition to clear degenerative arthrosis on both sides of the joint. Arthrodesis is an acceptable surgical option in the general population but not feasible in a dancer. To preserve motion, we recommend similar surgical treatment utilized for grade II, with cheilectomy and Moberg osteotomy ( Fig. 24.6, A−C ), with good clinical outcomes.
The sesamoid bones lie within the substance of the flexor hallucis brevis tendons. They are commonly injured in dancers, particularly in those who fail to perform a plié on landing, absorbing the energy of the landing through partially flexed knees. Without such absorption built into a dancer’s technique, sudden deceleration with high impact of the sesamoid bones predisposes to injury.
The differential diagnosis of sesamoiditis is lengthy and requires careful history taking and clinical examination. Magnetic resonance imaging (MRI) aids diagnosis.
The following is a list of differentials:
stress fracture of the sesamoid bone,
avulsion fracture or sprain of the proximal pole of the sesamoid,
sprain of the distal pole,
sprain of a bipartite sesamoid,
arthrosis of the sesamoid metatarsal joint,
and
preradiographic osteonecrosis of the sesamoids.
Several mechanisms are responsible for producing sesamoiditis in dancers. Most of these can be treated with a felt pad around the sesamoid for relief (“dancer’s pad”) ( Fig. 24.7 ). In general, symptoms resolve without any additional interventions, although it may take up to 6 months for full resolution. In those cases requiring further diagnostic testing, an MRI can be useful. The medial sesamoid is often bipartite, with rounded edges on plain radiograph, distinguishing it from a recent fracture. In those cases with recalcitrant pain, surgery may be warranted. A medial-based incision can locate the medial sesamoid; in the surgical treatment of lateral sesamoid pathology we prefer a dorsal approach in the first web space. A plantar incision should always be avoided because of the increased risk of plantar scarring and chronic plantar pain. Surgery should be reserved only for patients with symptoms persisting for at least 6 months following initial conservative treatment.

Other conditions may mimic sesamoiditis, including bursitis and nerve entrapment:
Sesamoid bursitis: Swelling and inflammation within the sesamoid bursa may mimic sesamoiditis. However, careful clinical examination usually can identify a symptomatic bursa when present. Treatment consists of a well-directed local corticosteroid injection to the bursa. Bursitis still may take some time to resolve, and it can be complicated by a fibrous scar that causes repeated symptoms. In such cases, a bursectomy can be performed through a careful medial approach.
Joplin’s neuroma: Entrapment of the proper digital nerve, adjacent to and, rarely, under the tibial sesamoid, will cause symptoms similar to sesamoiditis. Joplin’s neuroma, however, will display a characteristic nerve compression sign with palpation. In those cases recalcitrant to conservative therapy, neurolysis, and transposition of the nerve are required.
Lateral proper digital nerve entrapment: The lateral proper digital nerve may be compressed under the deep transverse ligament, causing pain in the great toe on the lateral side. Because of the position of the nerve, a compression test cannot be performed. Diagnosis is made with a selective local anesthetic injection to the nerve. Surgical resection of the transverse ligament is often curative.
In young ballet dancers, hyperflexion of the great toe interphalangeal joint (IPJ) can occur when attempting en pointe . Here, weight is distributed over the nail and dorsum of the toe in the pointe shoe. Hyperextension of the great toe IPJ also occurs, usually to compensate for lack of motion in adjacent joints. Rarely does this need surgical intervention, despite radiologic appearances, because the joint is quite accommodating and typically asymptomatic. In those who do complain of symptoms, lamb wool wrapping can help to alleviate the discomfort problem ( Fig. 24.8 ).

Metatarsalgia is uncommon in dancers, and when it is encountered, the differential diagnosis must include plantar plate injury with MTP instability and Freiberg’s infraction.
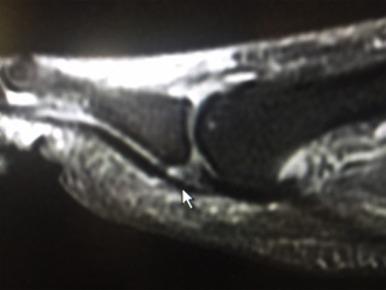
As the dancer relevés , the phalanx subluxes dorsally, pushing the metatarsal head plantarward and causing pain and overload of the plantar plate of the lesser MTP joints. In the demi-pointe position, excessive loads are transmitted through the second and third MTP joints. Clinical examination will elicit a translation in the anterior-posterior (AP) plane, positive drawer test, that is in excess of the adjacent joints. MRI can be a useful diagnostic tool, demonstrating either acute or chronic injury of the plantar plate ( Fig. 24.9 ). Treatment initially is directed at taping to neighboring toes and stress-relieving padding. We have used platelet-rich plasma (PRP) injections and prolotherapy (saline solution) with success. Surgical correction includes a very limited resection arthroplasty with a plantar condylectomy, through dorsal approach. Alternately, a limited Weil osteotomy may be used with screw fixation. A formal plantar plate repair should be used with care, since it can cause joint stiffness, which is not tolerated by professional dancers. Motion should always begin early. Scarring at the plantar aspect of the wound facilitates tightening of the redundant plantar plate.
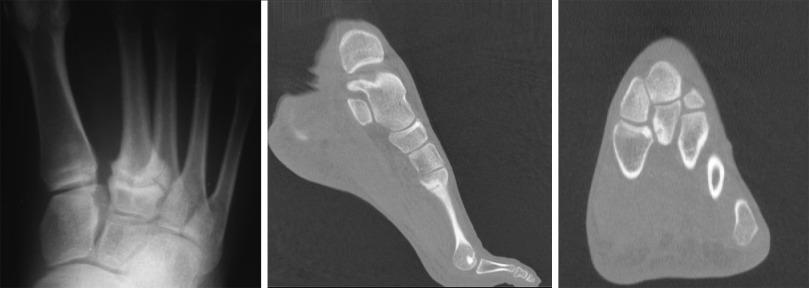
Dancers have a propensity to develop Freiberg’s infraction equal to that of the general population. In general, conventional radiography lags behind clinical symptoms by up to 6 months ( Fig. 24.10, A, B and C ). MRI facilitates early diagnosis.

Four types of infraction occur:
Type I: A localized osteonecrosis of the metatarsal head that heals by creeping substitution. No cartilage defect is seen.
Type II: Following metatarsal head osteonecrosis, the structural support of the head is lost. New bone formation occurs but is not sufficient to prevent collapse of the head. The articular cartilage is preserved; however, osteophytes on the dorsal lip limit dorsiflexion. Surgical debridement is curative, with exostectomy of the dorsal ridge to facilitate dorsiflexion.
Type III: In addition to metatarsal head collapse, the articular cartilage is destroyed. Surgical management includes excision of the dead bone and cartilage and osteophyte resection. The plantar aspect of the joint usually is intact and can be left alone.
Type IV: A rare entity with several heads involved. May represent a congenital epiphyseal dysplasia rather than a true infraction.
Most high-level dancers have a mild cavus foot. Despite the mechanical advantages it brings, this anatomy creates vis-à-vis technique where the rigidity of the foot places high stresses on the bones during impact. In those dancers who start their careers early in life, the metatarsals hypertrophy and the cortices broaden to accommodate the increased stresses placed on them. In certain cases, however, stress fractures occur despite cortical hypertrophy, because the repeated microtrauma of dancing exceeds the reparative capacity of the bone.
Because of the cuneiforms’ Roman arch configuration, the second metatarsal sits wedged between the medial and lateral cuneiform bones. This causes a relative rigidity to the second ray and consequently a potential site for a stress fracture. However, relative length of the second metatarsal is not considered a risk factor for fracture occurrence. In fact, this is the most common site for a stress fracture in the dancer’s foot, and when a patient complains of pain and tenderness in the base of the second metatarsal, it should be regarded as a stress fracture until proven otherwise.
The fracture line is usually transverse. Conventional radiographs may not show the fracture, but a computed tomography (CT) scan or an MRI will confirm clinical suspicion in such instances ( Fig. 24.11 ). As the second metatarsal hypertrophies from years of pressure in the demi-pointe position, it may have the appearance of a healing fracture. Again, MRI can be useful in determining the true diagnosis.
Acute injuries require a cam walker for up to 6 weeks to allow time for the fracture to consolidate. Cast immobilization usually is not required, provided that the dancer can be trusted to keep the cam walker in place as prescribed. Rarely, a fracture may progress to a delayed union, and in these cases a small ultrasound bone stimulator can be used to accelerate healing. Occasionally, internal fixation with a small plate and screws, associated with bone grafting, may be required.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here