Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
(see Fig. 27.1A–I )

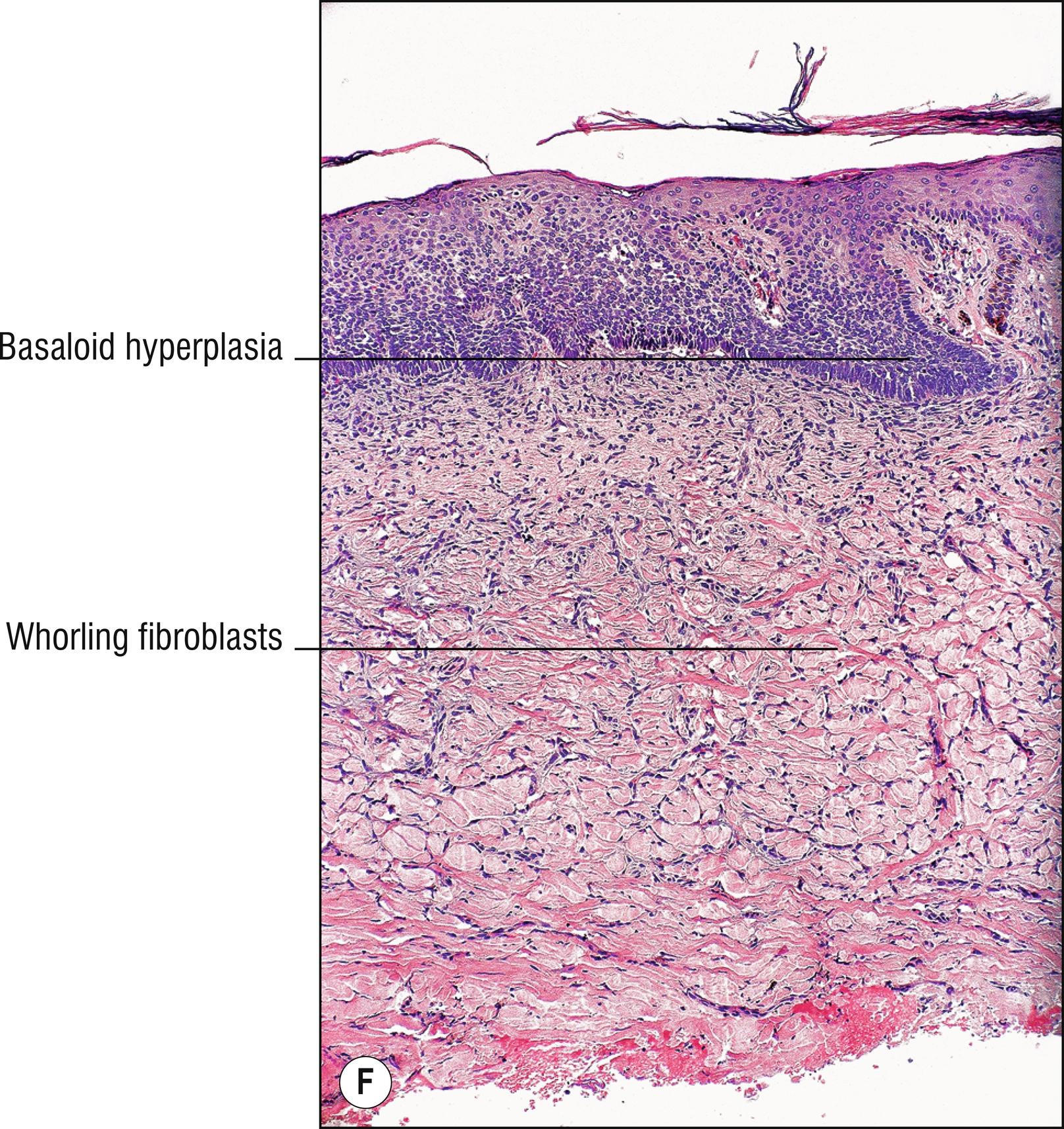

Brownish (1.18) nodules most common on the legs (1.67), also seen on upper extremities and trunk, rarely on the head or neck, probably originating from folliculitis, arthropod bites, or some other initial inflammatory condition. Some authors prefer to think of a dermatofibroma as fibrosing dermatitis rather than a neoplasm (an –oma). Often mistaken for “nevi” (20.5) by the non-dermatologist, but they are more indurated than nevi. DFs often have the dimple sign when inwardly compressed.
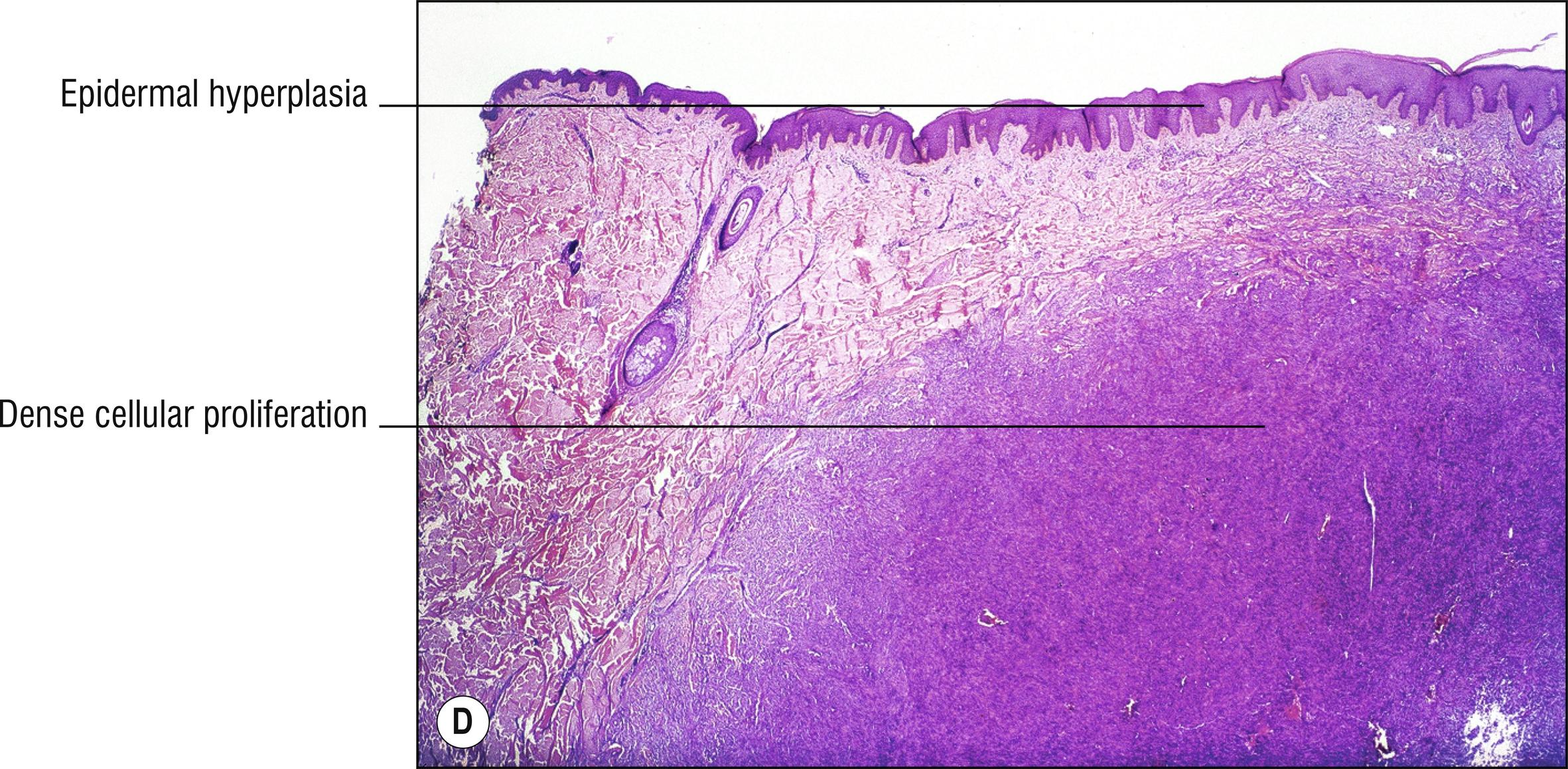
Epidermal hyperplasia (1.61) often, sometimes with flattened “ tabled ” rete ridges or basaloid proliferation simulating a basal cell carcinoma
Hyperpigmented basal layer often
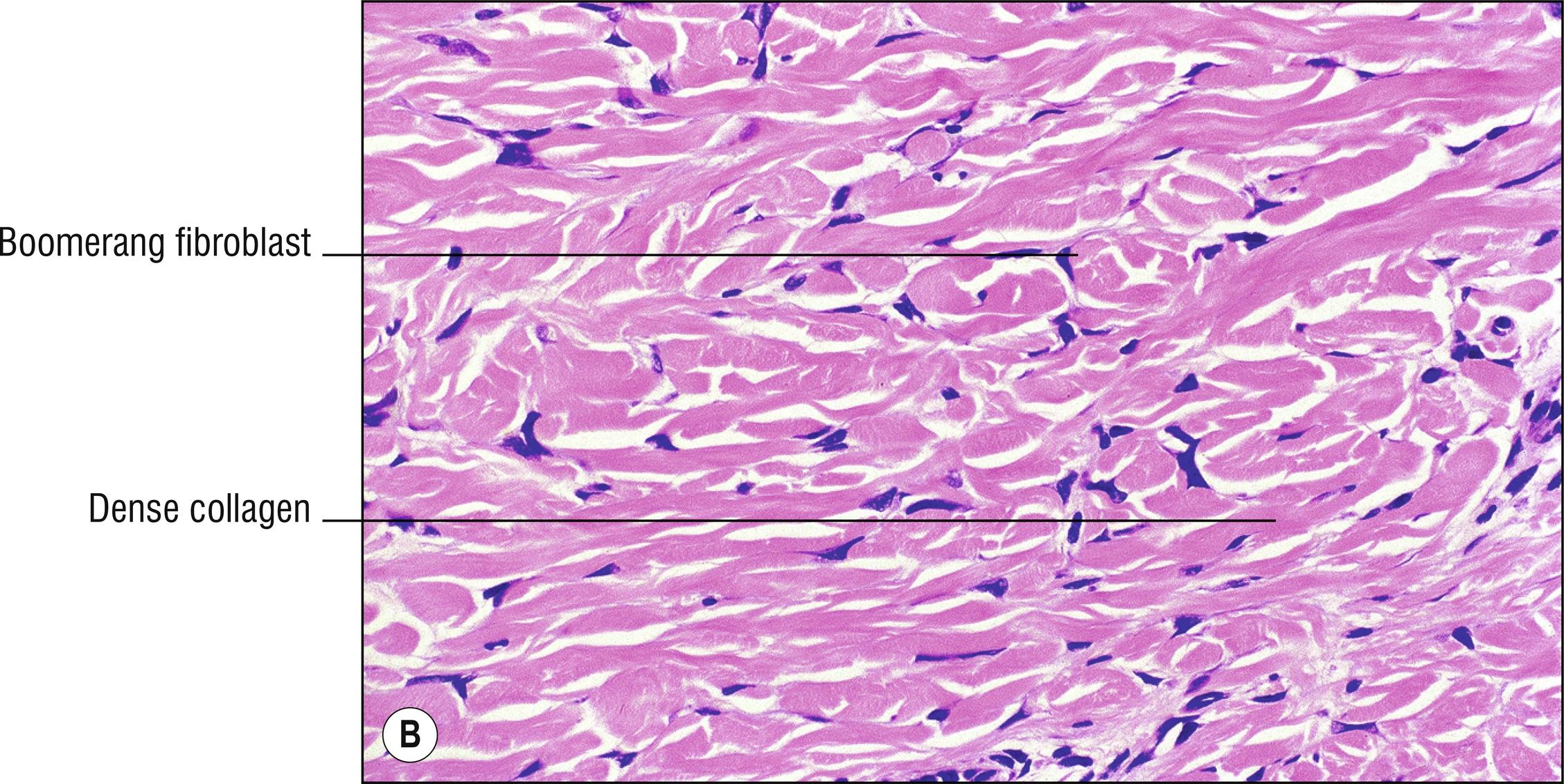
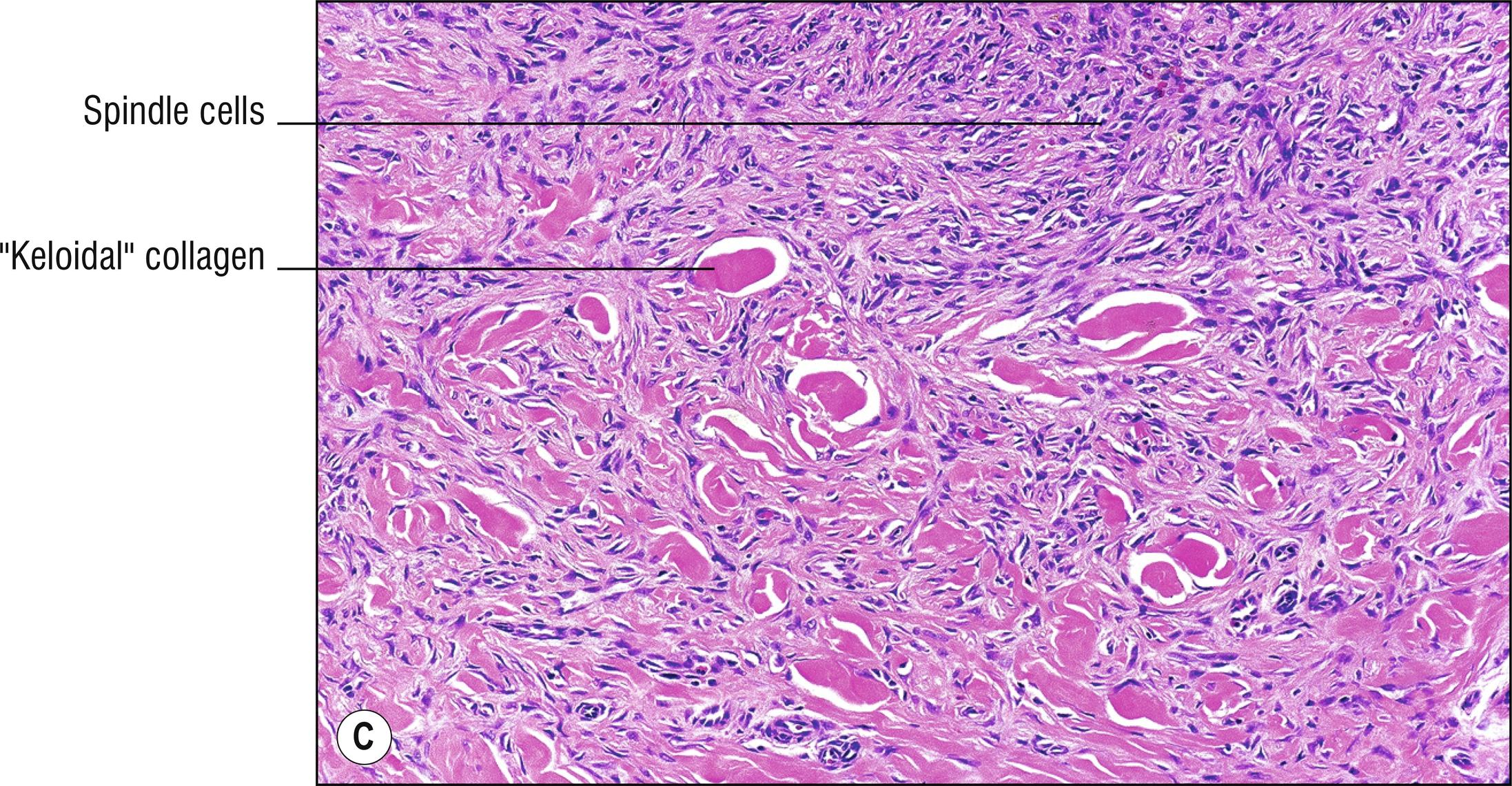
Poorly circumscribed proliferation of boomerang-shaped spindled fibroblasts or histiocytes in the dermis, often whorling about, blending into the surrounding dermis like a bomb was dropped in the dermis, sometimes extending into the subcutaneous fat
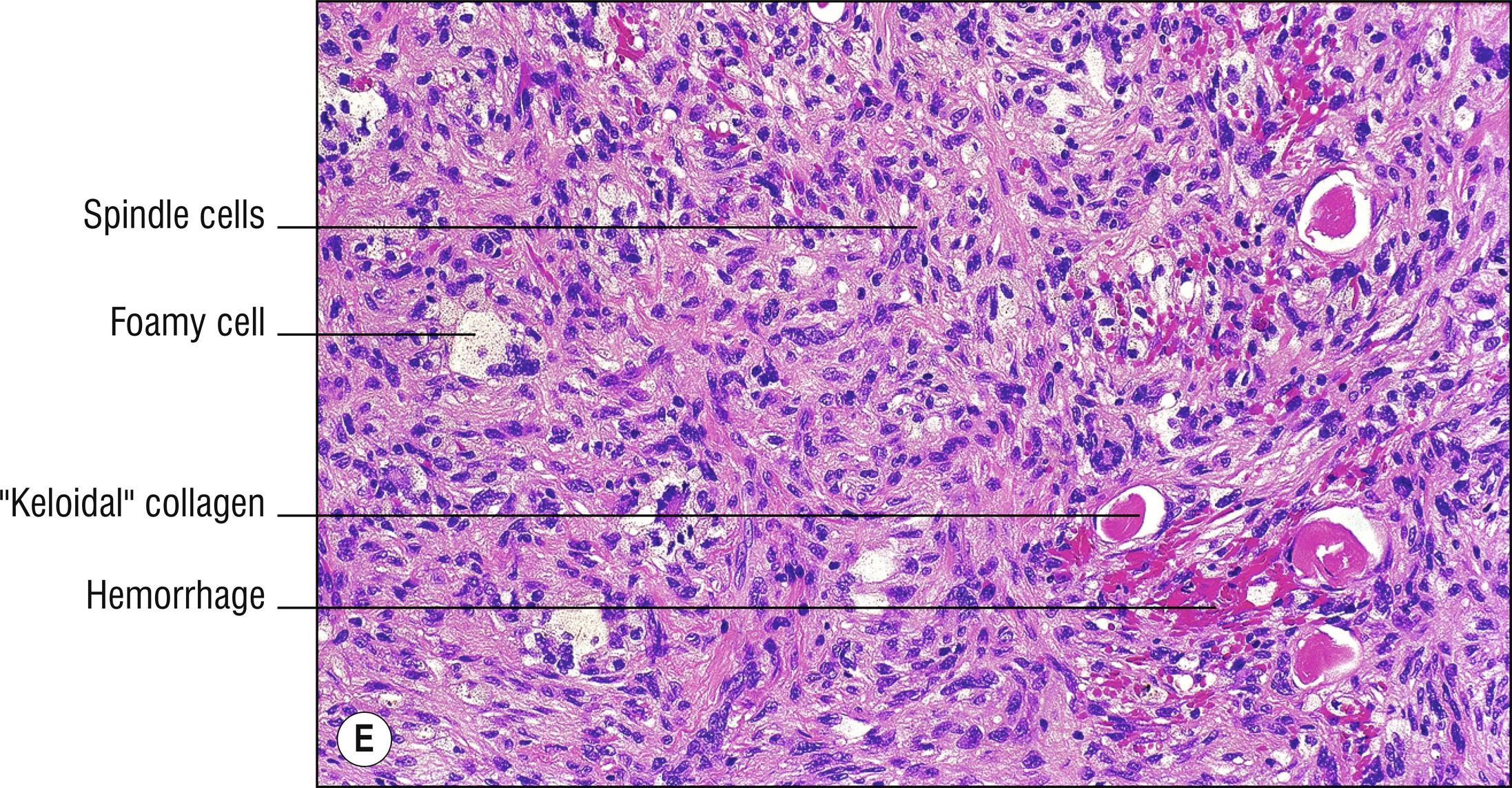
Multinucleated giant cells (1.84), Touton giant cells, or foamy histiocytes (1.46) sometimes
Hemosiderin often (1.58)
Large bundles of collagen (“ keloidal collagen ”) often present at periphery of lesion, with fibroblasts around the bundles (“collagen trapping”)
Positive for CD68 and CD163 like most of the lesions in this chapter. Also factor XIIIa + and CD34neg
Hemosiderotic DF (aneurysmal DF, sclerosing hemangioma): hemosiderin (1.58), prominent pseudovascularity, erythrocyte extravasation (1.40), may resemble Kaposi sarcoma (25.9).
Xanthomatous DF: foamy histiocytes, sometimes Touton giant cells (1.46).
Atrophic DF: atrophic epidermis (1.9) instead of hyperplastic.
DF with monster cells: occasional bizarre atypical giant cells are present, but still has benign behavior.
Palisading DF: Verocay-like bodies may resemble a schwannoma (26.2).
Cellular DF: larger, more numerous fibroblasts, may infiltrate fat, may closely resemble dermatofibrosarcoma protuberans (DFSP, 27.10).
Epithelioid cell fibrous histiocytoma: majority of cells are epithelioid (1.38), often with angulated shapes that may resemble Spitz nevus (20.6) or reticulohistiocytoma (7.8), with 88% of these expressing ALK1 ( chapter 30 ).
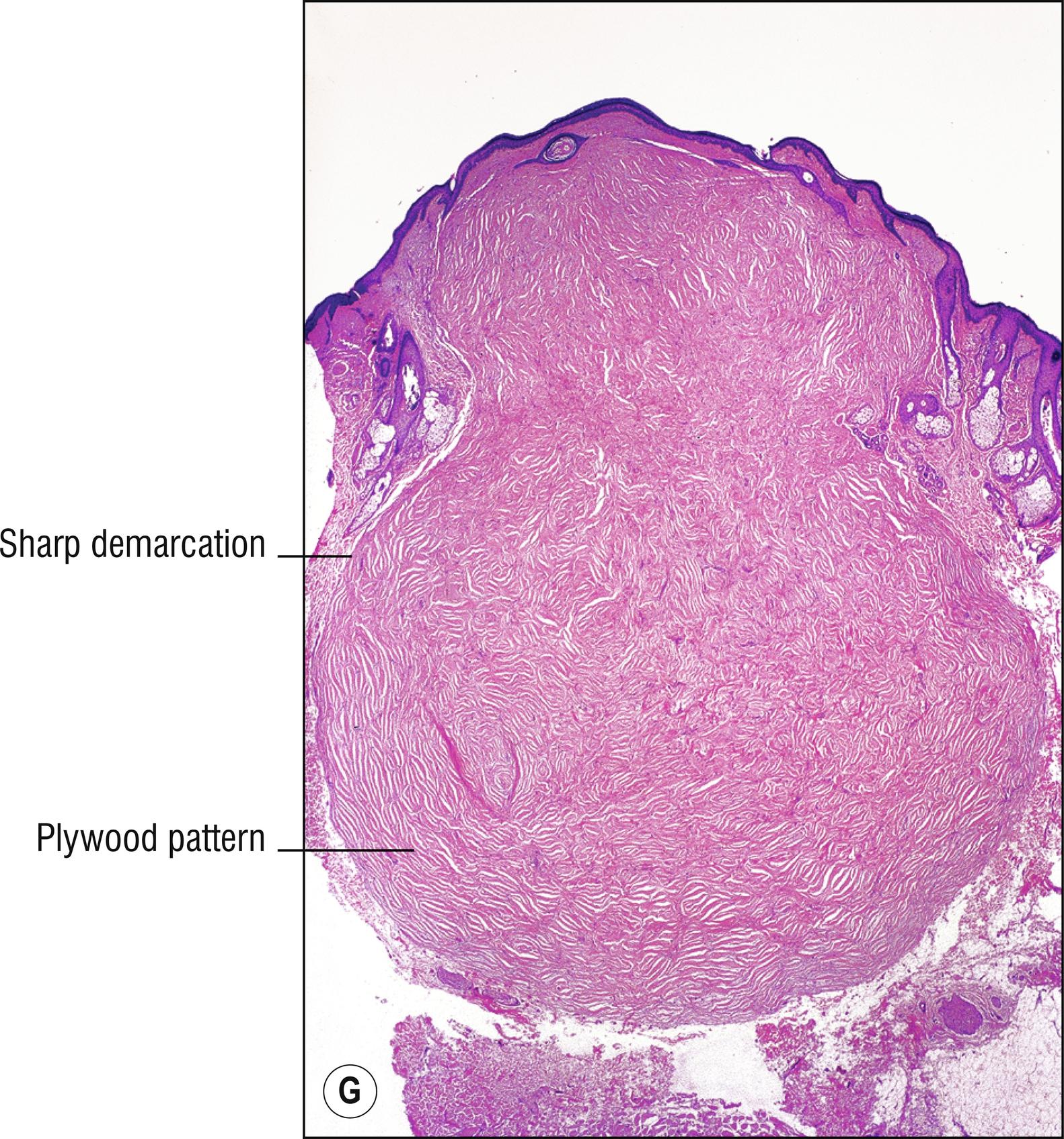
Sclerotic fibroma (circumscribed storiform collagenoma, plywood fibroma): sharply circumscribed, hyalinized plywood pattern of dense collagen, clefts between thick collagen bundles (1.23), mucin sometimes in the clefts (1.83), very few CD34 + and factor XIIIa + fibroblasts (hypocellular), some cases associated with Cowden’s disease (22.5). Giant cell collagenoma is a rare variant with multinucleated cells. The presence of ongoing type I collagen synthesis and positive staining for PCNA and Ki-67 suggest that it is a growing neoplasm rather than just a DF variant. Similar sclerotic changes may occur within an ordinary DF, however. EMA is negative.
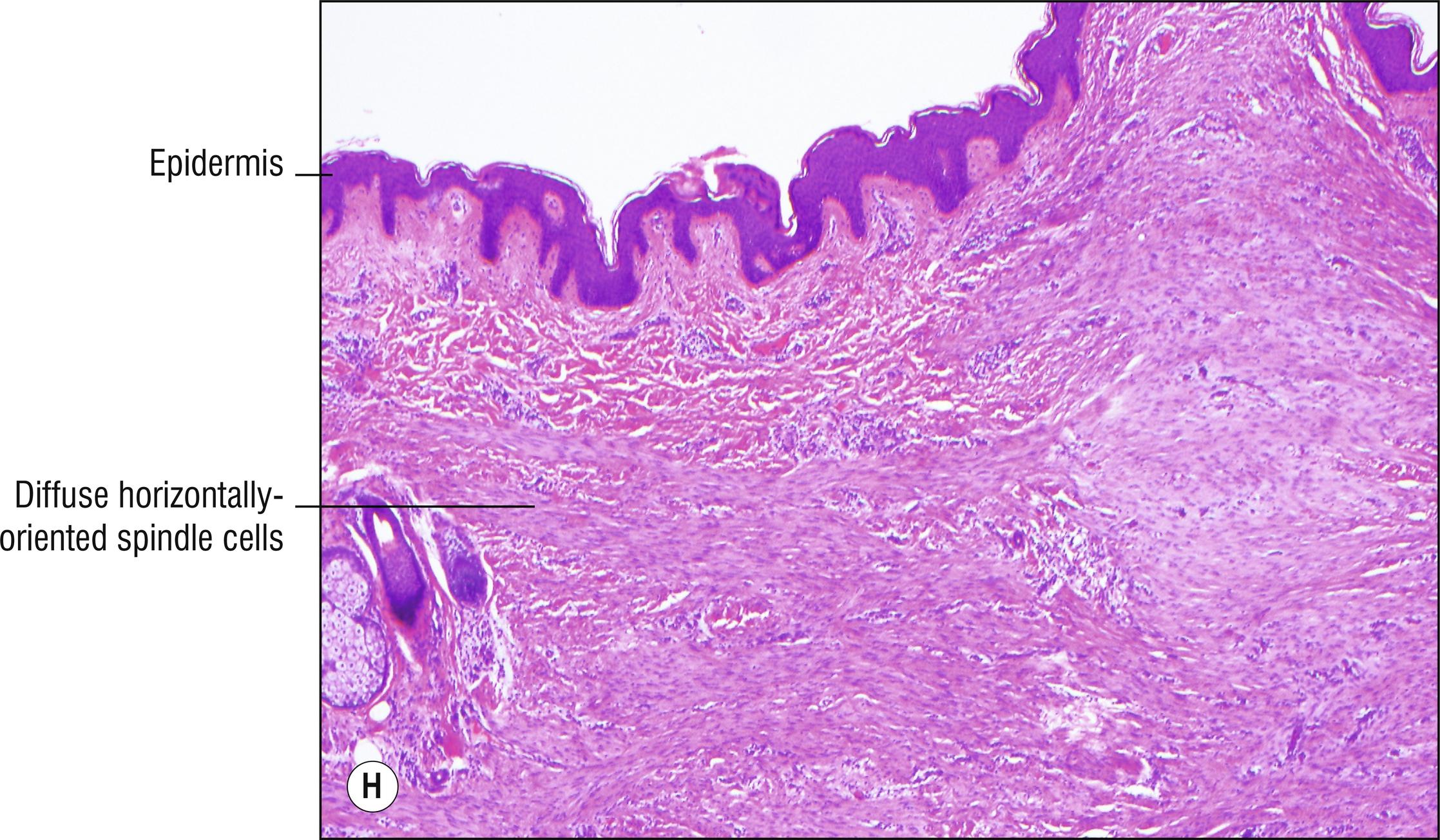
Dermatomyofibroma (myoid fibroma): red or white plaque of upper trunk or neck of young adults, slowly growing to several centimeters, usually does not recur. Myofibroblasts are oriented parallel to the epidermis , resemble leiomyoma or DFSP, and are actin positive and negative for CD34, factor XIIIa, and desmin.
Oral fibroma (mucosal fibroma, bite fibroma): very common mouth (1.82) nodule (especially buccal mucosa, lower lip, lateral tongue) related to trauma in the mouth.
Nuchal fibroma: Firm nodule, usually on posterior neck, may infiltrate muscle. Lesions not on the neck are related to desmoid tumors (27.15) and may be associated with Gardner syndrome. Dense sclerotic collagen, few fibroblasts, CD34 +, CD99 +, SMA-neg.
Scar (27.2): epidermal atrophy, fibroblasts tend to be oriented more parallel to the epidermis instead of whorling, with blood vessels more perpendicular.
Dermatofibrosarcoma protuberans (27.10): large size, location usually on the trunk, infiltrating bands of spindle cells extend into adipose, more prominent storiform pattern, mild cytologic atypia, no epidermal hyperplasia, usually no multinucleated giant cells or foam cells. DFSP is typically CD34 +, nestin +, factor XIIIa-neg, stromelysin-3-neg, D2-40-neg (all five stains are the opposite in DF). Intermediate lesions with worrisome histology and equivocal immunostaining are not rare and might be called fibrous neoplasm of uncertain malignant potential (FRUMP).
Leiomyoma (29.6).
Neurofibroma (26.1).
Desmoplastic nevus (20.5).
Other spindle cell neoplasms (1.131), epithelioid cell neoplasms (1.38), or granulomas (1.51).
(see Fig. 27.2A–C )



Although not a neoplasm, a scar is included here for comparison with other fibrohistiocytic proliferations. Scars are red initially, and then may become white (1.150) and sometimes indurated papules or plaques.
Epidermis atrophic or normal, often with loss of rete ridges
Subepidermal blister artifact is common (1.147)
Bands of fibroblasts and dense collagen, often oriented parallel to the epidermis
Young scars may have a pale or mucinous stroma and more fibroblasts, sometimes extravasated erythrocytes, while older ones have more collagen, less paleness, and fewer fibroblasts (more sclerotic)
Blood vessels tend to be more perpendicularly oriented with respect to the epidermis
Hypertrophic scar: thick scar that is significantly elevated above the skin surface to a greater degree than average.
Keloid: large nodule or plaque that grows like a neoplasm beyond the original site of injury , more in black skin, thicker hyalinized bands of collagen (“keloidal collagen”).
Striae distensae: linear tears in the skin, violaceous lesions later become white, usually in areas of tension, loss of elastic fibers in these areas.
Anetoderma (9.11): perhaps an unusual variant of scar.
Dermatofibroma (27.1), and other fibrous neoplasms (Chapter 27).
Other spindle cell neoplasms (1.131).
Other alterations of connective tissue (1.125, Chapter 9 ).
(see Fig. 27.3A–E )





Common small (1.5 mm), red to skin-colored papule , usually on the nose (1.95) or central face (1.44).
Collagen oriented concentrically around follicles or oriented more perpendicular to the epidermis
Sometimes increased numbers of stellate, plump fibroblasts
Few dilated blood vessels
Tuberous sclerosis (epiloia, Bourneville’s disease): autosomal dominant, type 1 due to mutation in TSC1 gene which codes for hamartin, type 2 is more common, more severe, and due to mutation in TSC2 gene which codes for tuberin. Multiple angiofibromas (misnamed adenoma sebaceum) on the central face that begin at puberty and are mistaken for acne (10.1), forehead angiofibrotic plaques, periungual fibromas (1.85), ash leaf white macules (1.150) since early childhood, café-au-lait macules (20.2), connective tissue nevi (Shagreen patch of the sacral area; 27.6), enamel teeth pits, epilepsy, and low intelligence (epiloia stands for this plus adenoma sebaceum), basal ganglia calcification, and a variety of internal neoplasms such as cerebral tubers and gliomas, retinal phakomata, cardiac rhabdomyomas, renal angiomyolipomas, and many other systemic lesions.
Pearly penile papules: multiple tiny 1-mm or smaller papules around the coronal sulcus of the penis (1.107) sometimes mistaken for warts (14.1).
Perifollicular fibroma: perifollicular accentuation of the fibrous tissue.
Familial myxovascular fibromas: rare papules on the hands (1.56).
Multiple endocrine neoplasia type 1 (MEA type 1, Wermer syndrome): facial angiofibromas, collagenomas (27.6), lipomas, parathyroid, pancreatic (glucagonoma, 3.2), pituitary tumors (1.105).
Multinucleate cell angiohistiocytoma (7.13).
Fibrofolliculoma and trichodiscoma (22.6), trichilemmomas (22.5), and trichoepitheliomas (22.2) can also be multiple on the face.
Fibrosing melanocytic nevus (20.5).
At first glance, these subtle papules may resemble normal skin (1.94).
Folliculitis (10.2) or acne (10.1) with fibrosis.
(see Fig. 27.4 )

Very common, often pedunculated (1.106), skin-colored (1.129) to brown, papules of eyelids (1.43), neck (1.86), axilla (1.10), or groin (1.55). Increased incidence with aging and obesity, controversial association with intestinal polyps.
Pedunculated papule (1.106), epidermis often extends almost completely around the specimen when it is sectioned
Papillomatosis and acanthosis common, sometimes epidermal atrophy (1.9)
Dermis consists of loose connective tissue that is often pale
Dilated blood vessels often
Dermatosis papulosa nigra (18.2).
Birt–Hogg–Dube syndrome (22.6).
Lipofibroma (“fibroma molle”): larger tag with adipose in the stroma , especially common on buttock and thigh, not to be confused with nevus lipomatosus (29.1).
Pleomorphic fibroma (pseudosarcomatous polyp): large atypical fibroblasts and histiocytes in the stroma, sometimes multinucleated, a pseudomalignancy (1.118).
Other papillomas (1.102).
Improper orientation of a thin, folded shave biopsy can resemble a tag.
(see Fig. 27.5A,B )


Uncommon finger-like projection from a digit or acral skin (1.56, 1.48).
Massive orthokeratosis , usually no parakeratosis, with acanthosis
Thickened collagen in the dermis, often oriented parallel to the long axis of the lesion
Supernumerary digit: congenital, mostly related to the fifth digit where a sixth digit would be expected, increased peripheral nerves present (26.3).
Acrochordon (27.4): different location, softer and less hyperkeratotic, less dense connective tissue.
Viral wart (14.1): more papillomatosis, hypergranulosis, koilocytosis, columns of parakeratosis, less dense connective tissue.
Periungual fibroma (27.3): association with tuberous sclerosis, more blood vessels, plump fibroblasts.
Other lesions with hyperplasia of epidermis (1.61) or scars, sclerosis, or fibrosis (1.125).
(see Fig. 27.6A,B )


Uncommon skin-colored (1.129) papules , nodules or plaques , present at birth , or arising in childhood. Clinically and histologically, may be subtle and may resemble normal skin (1.94).
Poorly demarcated nodule with increased collagen and normal, decreased, or increased elastic fibers. Sometimes the changes are easily missed unless surrounding normal skin is biopsied for comparison
Shagreen patch of tuberous sclerosis (27.3): pigskin cobble-stoned plaque most common in the sacral area , no increased elastic tissue.
Nevus elasticus: increased elastic fibers (1.31).
Buschke–Ollendorff syndrome (BOS): rare, autosomal dominant, mutation resulting in loss of function of LEMD3, affecting BMP signaling, resulting in upregulation of SMAD and transforming growth factor (TGF)-β. Multiple scattered papules are mostly connective tissue nevi with increased elastic fibers (nevus elasticus), but some have mostly increased collagen (dermatofibrosis lenticularis disseminata), osteopoikilosis (spotted bones; 1.16).
Other diseases with altered connective tissue ( Chapter 9 ), and scars, sclerosis, and fibrosis (1.125).
Elastofibroma: actually no resemblance to nevus elasticus except its name, large subcutaneous mass on shoulder with increased clumped elastic fibers.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here