Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The coexistence of fever and rash suggests a relatively wide spectrum of pathologic entities for diagnostic consideration. This spectrum includes local or systemic infection with a wide range of microbial pathogens; toxin-mediated disorders, including those associated with bacterial superantigen production; inflammatory conditions including vasculitides and rheumatologic diseases; and hypersensitivity disorders. While most conditions causing fever and rash are benign and self-limited, a thorough clinical evaluation is crucial to identify those caused by life-threatening diseases or those requiring specific treatment. The essential elements for accurate diagnosis include a detailed history and a thorough physical examination including a careful systematic observation of the patient for evidence of toxicity. Because this approach lacks perfect sensitivity, the laboratory may play an important role in the diagnostic process.
Information about the features of the rash includes when it occurred in relation to the fever, its evolution or progression, its anatomic distribution, and whether it is pruritic or painful ( Table 53.1 ). Degree of illness should be evaluated, especially in the infant and toddler, by assessing oral intake, activity level, and urine output. A description of the fever pattern can be useful (see Chapter 52 ) and immunization status will help prioritize the differential diagnosis. Essential information from the epidemiologic and social history should include season of the year; geographic location of the patient’s residence; exposure to known ill contacts; recent travel or exposure to individuals from different geographic areas; exposure to pets, wildlife, or insects; recent immunizations; ingestion of raw meat or fish, unpasteurized dairy, and/or potentially contaminated meat or produce; a detailed list of medications; previous blood transfusion; and, for the adolescent patient, intravenous drug use and sexual activity.
| Demographic Data |
|
|
|
|
|
|
|
|
|
|
|
|
|
| Features of Rash |
|
|
|
|
|
| Associated Symptoms |
|
|
| Prior Health Status |
|
|
|
| Family History |
The medical and family history should be used to assess the overall health of the patient over time, as well as that of family members, to determine the possibility of underlying primary or acquired immunodeficiency or diseases associated with autoimmunity or chronic inflammation. A history of increased susceptibility to infection, as manifested by chronic or recurrent infections after infancy such as pneumonia, sinusitis, bronchitis, otitis media, diarrhea, and bacteremia, is an important indicator of underlying immunodeficiency disease (see Chapter 54 ). In addition, the occurrence of an unusually severe infection or an infection with a pathogen of low virulence (e.g., Pneumocystis jiroveci ) should raise suspicion for an immunodeficiency state. A history of hemolytic anemia, leukopenia, thrombocytopenia, or arthritis suggests an autoimmune disorder or malignancy, which may also be associated with impairment in immune function (see Chapter 44 ).
In a thorough systems review, the clinician should assess the probability of a subacute or chronic underlying infectious, inflammatory, or malignant disease by inquiring about anorexia, nausea, vomiting, weight loss or failure to thrive, night sweats, fatigue, cough, and exercise intolerance. The clinician should seek symptoms suggesting multisystem disease, such as myalgias, arthralgias, headache, precordial pain or pain with inspiration, abdominal pain, jaundice, skin photosensitivity, peripheral edema, alopecia, Raynaud phenomenon, and hematuria. In patients with symptoms that indicate the presence of multisystem disease, a thorough survey of the functional status of the central, peripheral, and autonomic nervous systems is clinically relevant. Specific inquiries into visual disturbances, photophobia, disordered mentation, neck stiffness, paresthesia, weakness, or seizure activity are essential and may reveal potentially life-threatening infection within the central nervous system or a systemic vasculitis involving the nervous system, such as systemic lupus erythematosus (SLE) or polyarteritis nodosa.
The physical examination is used to refine the probability of underlying serious illness, to identify rashes typical of a specific diagnosis, to look for noncutaneous disease manifestations, and to identify if further testing or treatment is indicated ( Tables 53.2 and 53.3 ; also see Chapter 52, Chapter 61 ).
| Degree of Toxicity |
| Vital Signs |
|
|
|
|
| Characteristics of Rash |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Distribution and Localization of Rash |
|
|
|
| Associated Enanthem |
|
|
|
|
| Associated Findings (Isolated or in Clusters) |
|
|
|
|
|
|
|
|
|
| Bacterial |
|
| Viral |
|
| Infestation |
|
| Immunologic |
|
|
|
A critical first step is an assessment of the patient’s vital signs and degree of toxicity. Lethargy, irritability, altered mental status, decreased activity, poor perfusion, pallor, mottled skin, decreased pulses, or cyanosis indicates serious illness; resuscitation and treatment directed at the most likely diagnoses should be initiated without delay. The importance of the height of fever in predicting the risk of serious illness is unclear. Underlying chronic illness and degree of toxicity are more useful for risk assessment than fever height. The presence of tachycardia and tachypnea in any patient with fever and rash suggests the possibility of sepsis. Tachycardia may also be seen in endocarditis or in myocarditis secondary to certain viruses, Kawasaki disease (KD), multisystem inflammatory syndrome children (MIS-C), or acute rheumatic fever. Evidence of alteration in mental status suggests either sepsis associated with decreased organ perfusion or primary meningoencephalitis. The presence of hypotension usually indicates septic shock, but other disorders such as toxic shock syndrome (TSS), dengue hemorrhagic shock syndrome, KD shock syndrome, MIS-C, hemorrhagic fever with renal syndrome caused by hantavirus, and lupus myocarditis must also be considered in this context. Hypertension may be noted in association with vasculitic disorders involving small- to medium-sized arteries, such as polyarteritis and SLE.
The clinical characteristics of the rash are often helpful in establishing an etiologic diagnosis. A morphologic nomenclature of cutaneous manifestations helps the clinician with differential diagnosis, documentation, and communication (see Chapter 61 ). An exanthem is defined as a skin eruption occurring as a sign of a generalized disease. An enanthem is an eruption on the mucous membranes that occurs in the context of generalized disease. Exanthems and enanthems may be macular, maculopapular, vesicular, urticarial, petechial, or diffusely erythematous. Rashes are usually classified according to their most typical lesion morphology. However, morphology may vary as rashes evolve; the rash of Rocky Mountain spotted fever is classically described as petechial, but it may initially be maculopapular. In addition, the rash of chickenpox begins as a papule that progresses to vesicular that then forms crusted lesions; all stages are present at the same time. Because a wide variety of infectious agents, including viruses and a broad range of bacteria (including rickettsiae), as well as drugs and inflammatory conditions can cause exanthems and enanthems, few of these eruptions are pathognomonic ( Tables 53.4, 53.5, and 53.6 ).
| Lesion | Pathogen or Associated Factor |
|---|---|
| Maculopapular or Macular Rash | Viruses |
Bacteria
|
|
Rickettsiae
|
|
Other
|
|
| Diffuse Erythroderma | Bacteria |
Fungi
|
|
| Urticarial Rash | Viruses
|
Bacteria
|
|
Other
|
|
| Vesicular, Bullous, Pustular | Viruses |
Bacteria
|
|
Other
|
|
| Petechial-Purpuric | Viruses
|
| Bacteria | |
Rickettsiae
|
|
Other
|
|
| Erythema Nodosum | Viruses
|
Bacteria
|
|
Fungi
|
|
Other
|
|
| Distinctive Rashes | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Disease | Cause | Age | Season | Transmission | Incubation (Days) | Prodrome | Features and Rash Structure | Enanthem | Complications | Prevention/Treatment | Comments |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Scarlet fever | Group A streptococcus | School age | Fall, winter, spring | Direct contact, droplets | 1–4 | Sore throat, headache, abdominal pain, cervical lymphadenopathy, fever, 0–2 days, acute onset | Diffuse erythema with “sandpaper” feel; accentuation of erythema in flexural creases (Pastia lines); circumoral pallor, lasts 2–7 days; may exfoliate | Palatal petechiae, strawberry tongue | Peritonsillar abscess, rheumatic fever, glomerulonephritis | Prevent rheumatic fever with penicillin within 10 days of onset of pharyngitis, treat with penicillin | Similar syndrome may be noted with Arcanobacterium haemolyticum in adolescents; group A streptococci may also produce toxic shock or true bacteremic shock syndromes in addition to cellulitis, lymphangitis, and erysipelas; Staphylococcus aureus may produce a scarlatiniform rash |
| Staphylococcal scalded skin syndrome (SSSS) | S. aureus –producing exfoliative toxin | Neonates, infants, young children | Any | Colonization, contact | Unknown | None | Sudden onset, tender erythroderma progressing to diffuse flaccid bullae; significant perioral, perinasal peeling; eventual diffuse exfoliation (positive Nikolsky sign), possibly conjunctivitis, purulent rhinorrhea | Unusual | Shock | Treat with intravenous antibacterial active against S. aureus | — |
| Toxic shock syndrome (TSS) | S. aureus –producing toxic shock syndrome toxin-1 (TSST-1) and staphylococcal enterotoxins (SEs) Group A streptococcus–producing Streptococcus pyogenes exotoxins (SPEs) |
Adolescent females if menstrual; others variable | Any | Colonization, contact | Variable, often 1–5 | Myalgias, fevers, and gastrointestinal symptoms May be secondary to wound infection, trivial mucosal or respiratory infection, or necrotizing fasciitis or myositis |
Diffuse sunburn-like erythroderma; hypotension, diarrhea, emesis, mental status changes; late desquamation | Conjunctivitis | Shock, multisystem organ dysfunction/failure | Treat with intravenous antibacterial active against S. aureus ; penicillin if group A streptococcus suspected; clindamycin; possible intravenous immune globulin; prevent menstrual-associated TSS by frequent changes of tampon | — |
| Meningococcemia | Neisseria meningitidis | Any (<5 yr and adolescents) | Winter, spring, follows influenza epidemics | Close, prolonged contact | 5–15 | Fever, malaise, myalgia, 1–10 days | Erythematous, nonconfluent, discrete papules (early); petechiae, purpura present on trunk, extremities, palms, soles | Petechiae | Shock, meningitis, pericarditis, arthritis, endophthalmitis, gangrene, disseminated intravascular coagulation | Contacts: rifampin; general: vaccine; treat with ceftriaxone, penicillin (if sensitive) | Neisseria gonorrhoeae , pneumococcus, Haemophilus influenza type b, group A streptococcus may produce similar clinical manifestations |
| Rocky Mountain spotted fever (RMSF) | Rickettsia rickettsii | Any (>5 yr), male > female | Summer | Carrier ticks | 3–12 | Fever, myalgia, headache, malaise, ill appearance, 2–4 days | Early maculopapular, then petechial or, rarely, purpuric; present on extremities, then trunk, palms, and soles | Petechiae variable | Shock, myocarditis, encephalitis, pneumonia | Remove ticks as soon as possible; use tick repellants; treat with doxycycline | Ehrlichia chaffeensis and other rickettsiae may produce similar illnesses with or without a rash |
| Rickettsialpox | Rickettsia akari | Any | Any | Mouse mite | 7–14 | Fever, chills, headache, malaise, 4–7 days | At primary bite site, eschar; secondary papulovesicles in same stage throughout illness; fewer vesicles than in chickenpox (5–30); present on trunk and proximal extremities | Occasional, transient lesions in the oral cavity similar to that seen on the body | Usually none | Treat with doxycycline | Often confused with chickenpox; may be more common than expected, especially in crowded urban settings with poor housing |
| Disease | Cause | Age | Season | Transmission | Incubation (Days) | Prodrome | Features and Rash Structure | Enanthem | Complications | Prevention/Treatment | Comments |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measles (rubeola) | Measles virus | Any | Winter, spring | Respiratory droplet | 10–12 | High fever, cough, coryza, conjunctivitis, 2–4 days | Maculopapular (confluent), begins on face, spreads to trunk; lasts 3–6 days Brown color develops; fine desquamation; toxic, uncomfortable appearance, photophobia; rash may be absent in HIV infection |
Koplik spots on buccal mucosa before rash | Febrile seizures, otitis, pneumonia, encephalitis, laryngotracheitis, thrombocytopenia; delayed subacute sclerosing panencephalitis | General: measles vaccine at 12–15 mo and again at 4–6 yr Exposure: measles vaccine if within 72 hr; immune globulin if within 6 days of exposure (must then wait 6–8 mo to vaccinate) World Health Organization recommends treatment with vitamin A in all patients with measles |
Reportable to public health department; epidemics reported, contagious 3 days before symptoms until 4 days after rash Increasing incidence as vaccination rates are decreasing |
| Rubella (German measles) | Rubella virus | Infants, young adults | Winter, spring | Respiratory droplet | 14–21 | Malaise, fever <101°F, posterior auricular, cervical, occipital adenopathy, 0–4 days | Discrete, nonconfluent, rose-colored macules and papules, begins on face and spreads downward; lasts 1–3 days | Variable erythematous macules on soft palate | Arthritis, thrombocytopenia, encephalopathy; fetal embryopathy | General: rubella vaccine at 12–15 mo and again at 4–6 yr; exposure: possibly immune serum globulin | Reportable to public health department; epidemics reported, contagious 2 days before symptoms and 5–7 days after rash |
| Roseola (exanthem subitum) | Human herpesvirus type 6 (HHV-6), human herpesvirus type 7 (HHV-7) | Infants/toddlers (6 mo–2 yr) for HHV-6, can be older children for HHV-7 | Any | Secretions of asymptomatic close contacts | 9–10 (HHV-6); unknown (HHV-7) | Irritability, high fever 3–7 days, cervical, occipital adenopathy | Discrete macules on trunk, neck; sudden-onset rash with defervescence; lasts 0.5–2 days; some patients have no rash | Variable erythematous macules on soft palate | Single or recurrent febrile seizures; encephalopathy; dissemination (e.g., liver, CNS, lung) in immunosuppressed patients | None | No epidemics |
| Fifth disease (erythema infectiosum) | Parvovirus B19 | Prepubertal children, schoolteachers | Winter, spring | Respiratory droplets; blood transfusion, placenta | 5–15 | Headache, malaise, myalgia; often afebrile | Local erythema of cheeks (slapped cheek appearance); lacy pink-red erythema of trunk and extremities, ± pruritus; rash may lag prodrome by 3–7 days; lasts 2–4 days, may recur 2–3 wk later | Rare, ill-described, on buccal mucosa | Arthritis, aplastic crisis in patients with chronic hemolytic anemia (e.g., sickle cell), fetal anemic hydrops, vasculitis, Wegner granulomatosis | Isolation of patients with aplastic crisis but not normal host with fifth disease | Epidemics reported; once rash is present, the normal host is not contagious; patients with aplastic crisis often have no rash |
| Chickenpox (varicella) | Varicella-zoster virus | 1–14 yr (most) but can vary | Late fall, winter, early spring | Respiratory droplet | 10–21 | Fever | Pruritic papules, vesicles in various stages, 2–4 crops and then crusts; distributed on trunk and then face, extremities; lasts 7–10 days; recurs years later in dermatomal distribution (zoster, shingles) | Oral mucosa, tongue | Staphylococcal or streptococcal skin infection, arthritis, cerebellar ataxia, encephalitis, thrombocytopenia, Reye syndrome (with aspirin), myocarditis, nephritis, hepatitis, pneumonia; dissemination in immunocompromised | VZIG for exposed immunosuppressed patients, susceptible pregnant women, preterm neonates, and infants at birth whose mother developed varicella 5 days before and 2 days after birth; active immunization with live attenuated vaccine at 12 mo | Acyclovir therapy for immunosuppressed and possibly normal patients (controversial); contagious 1–2 days before rash until all lesions are crusted |
| Enteroviruses | Coxsackievirus, echovirus, and others | Often infants and young children but varies | Summer, fall | Fecal-oral, respiratory, vertical, and possibly fomites | 4–6 | Variable: irritable, fever, sore throat, myalgias, headache | Hand-foot-and-mouth: vesicles in those locations; others: nonspecific, usually fine nonconfluent, macular or maculopapular rash, rarely petechial, urticarial, or vesicular; lasts 3–7 days | Yes | Aseptic meningitis, hepatitis, myocarditis, paralysis: usually in younger patients | None | Rash may appear with fever or after defervescence; rash may be present in <50% of enteroviral illnesses; epidemics possible, contagious up to 2 wks |
| Mononucleosis | Epstein-Barr virus | Children, adolescents | Any | Close contact, saliva, blood transfusion | 28–49 | Fever, adenopathy, eyelid edema, sore throat, hepatosplenomegaly, malaise; atypical lymphocytosis | Maculopapular or morbilliform on trunk, extremities; may be confluent; often elicited by simultaneous administration of ampicillin or allopurinol; rash in 15% and in 50% with drug-induced form, lasts 2–7 days | Variable | Anemia, thrombocytopenia, aplastic anemia, hepatitis, encephalitis; rarely hemophagocytic lymphohistiocytosis, lymphoproliferative syndrome | None | Cytomegalovirus and toxoplasmosis also produce mononucleosis-like illness; monospot or heterophile tests negative |
| Gianotti-Crosti syndrome (papular acrodermatitis of childhood) | EBV, hepatitis B virus (uncommon where vaccination rates are high), coxsackieviruses, others | 1–6 yr (primarily) | Any | Variable; fecal, sexual, blood products for hepatitis B | Unknown; 50–180 days for hepatitis B | Usually none except for specific viral disease; arthritis-arthralgia for hepatitis B | Papules, papulovesicles, discrete or confluent; face, arms, extremities, often spares trunk; lasts 4–10 days | Variable | As per specific disease | Hepatitis B: HBIG plus vaccine | — |
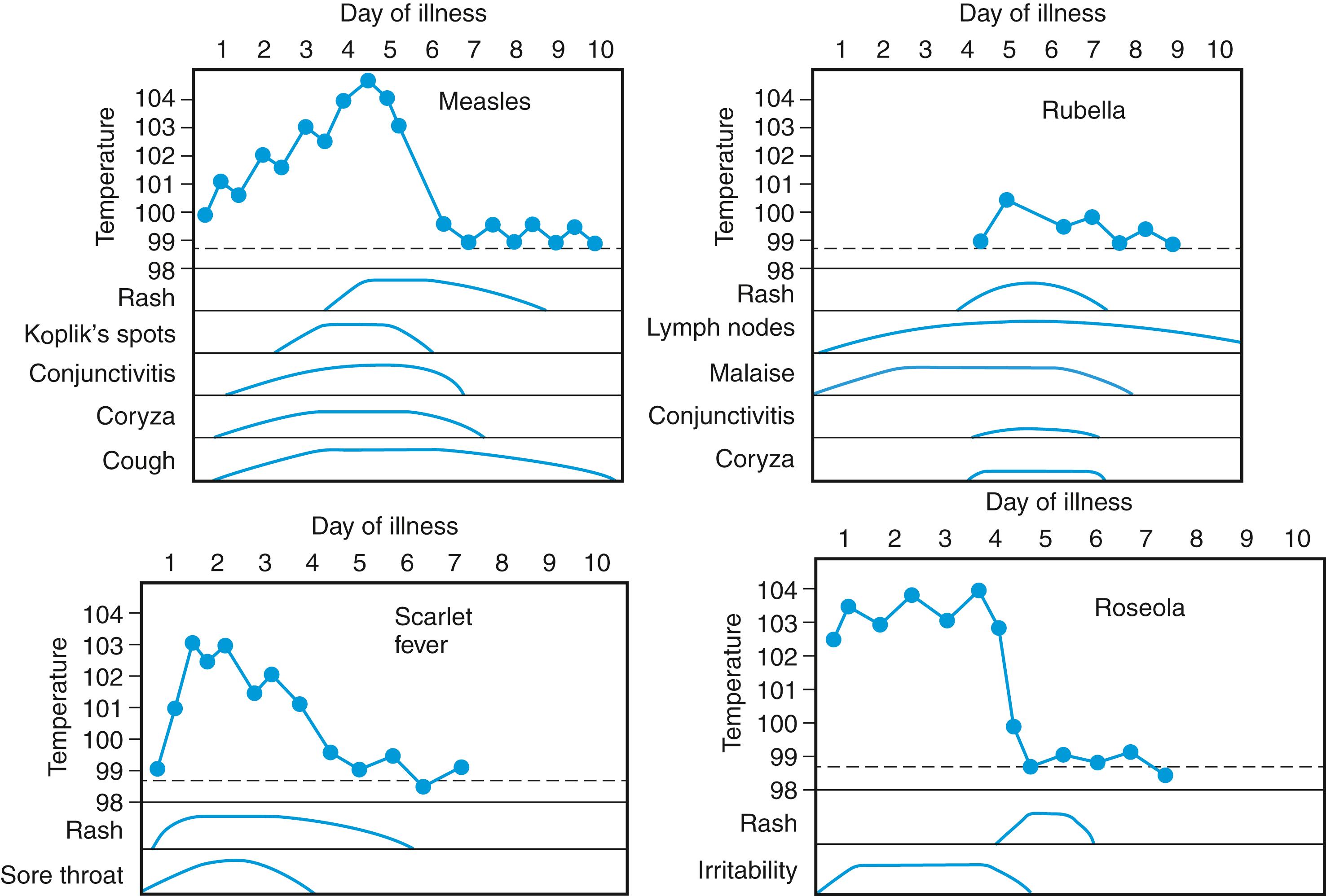
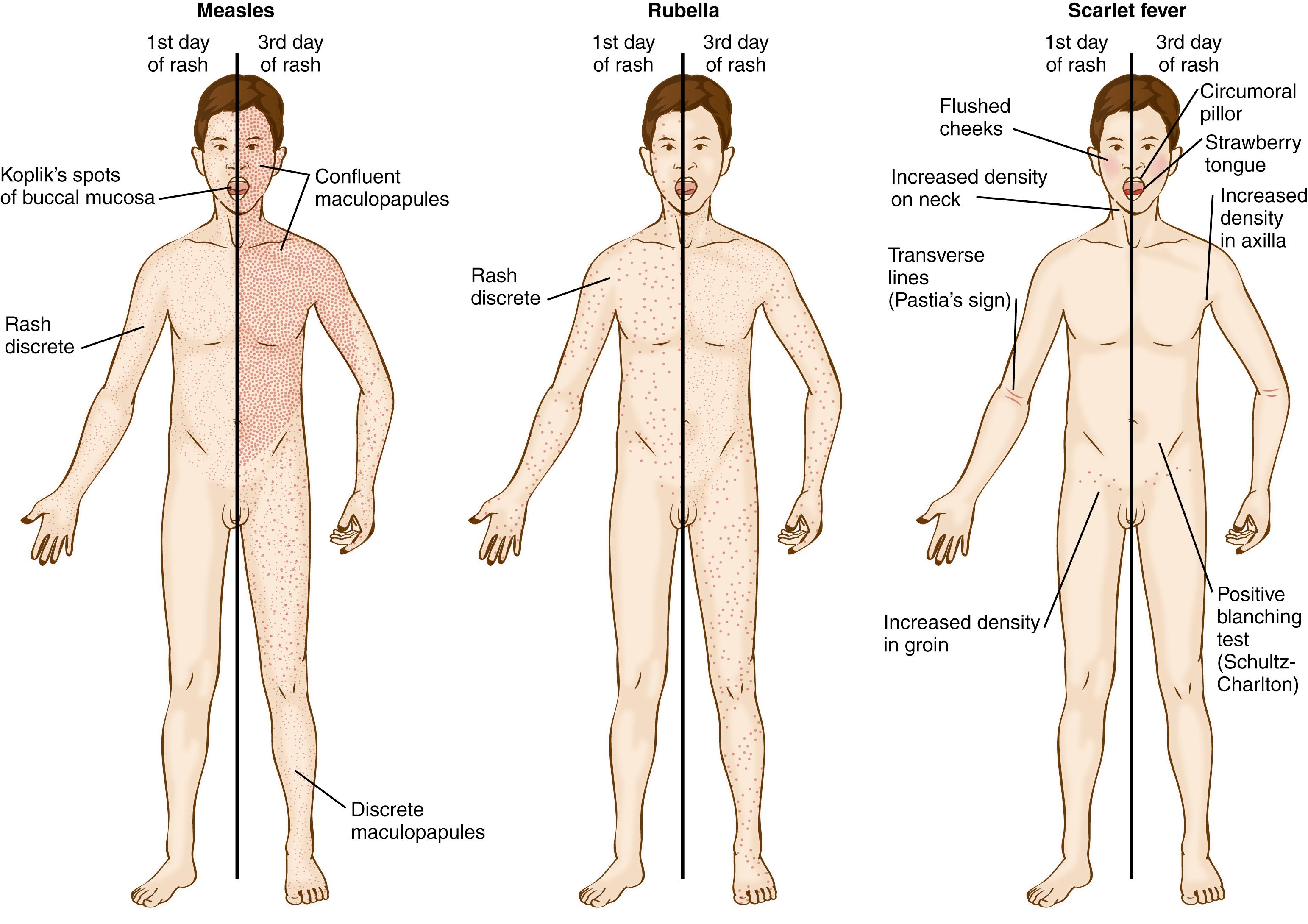
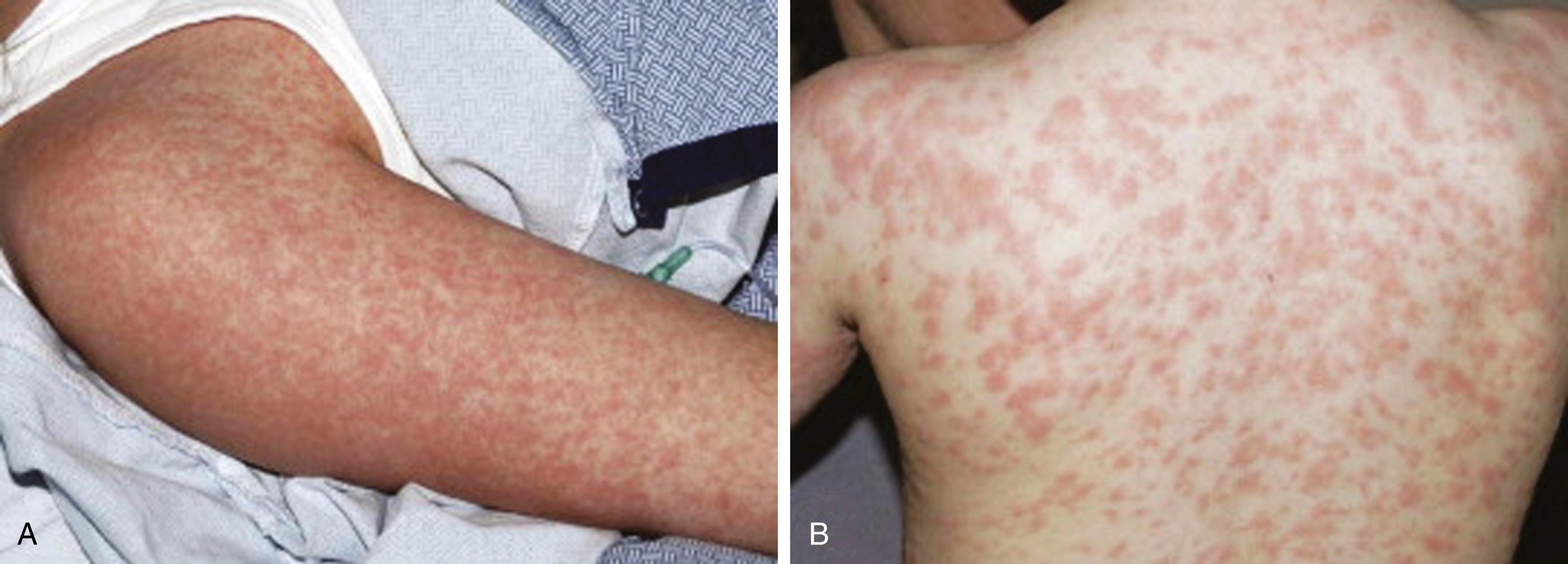
Macules are flat, nonpalpable circumscribed lesions, while papules are <1 cm, circumscribed palpable lesions. Maculopapular lesions may coalesce into a more confluent morbilliform (measles-like) eruption. A rash with multiple small papules that feels like sandpaper is described as scarlatiniform . Maculopapular rashes are usually seen in viral illnesses, drug eruptions, and immune complex–mediated disorders. The classic childhood exanthems such as measles, rubella, erythema infectiosum (fifth disease, caused by parvovirus B19), and roseola (exanthem subitum, caused by human herpesvirus types 6 and 7) produce a maculopapular rash and are usually clinically recognizable ( Figs. 53.1 and 53.2 ; see Table 53.6 ). Other organisms that commonly cause a maculopapular rash include enteroviruses, Epstein-Barr virus (EBV), cytomegalovirus, adenovirus, acute HIV, and hepatitis B virus. Erythema migrans, the distinctive rash of Lyme disease (caused by the tick-borne spirochete Borrelia burgdorferi ), begins as a papule at the site of a recent tick bite and slowly expands over days to weeks to form an erythematous, annular lesion, sometimes with partial central clearing ( Fig. 53.3 ). The rash of southern tick-associated rash illness (STARI) appears similarly. Erythema marginatum, a rare but major manifestation of acute rheumatic fever, is also distinctive ( Fig. 53.4 ).


Morbilliform drug eruptions are often indistinguishable from viral exanthems and typically present 7–14 days after exposure to a drug ( Fig. 53.5 ). As with most viral exanthems, the rash starts on the trunk and spreads to the extremities. Examples of causative agents include aminopenicillins, cephalosporins, antiepileptics, and sulfonamides. Morbilliform drug eruptions usually resolve spontaneously after discontinuation of the culprit drug, but sometimes they are the first sign of the potentially life-threatening syndrome drug rash with eosinophilia and systemic symptoms ( DRESS , also known as drug-induced hypersensitivity syndrome, formerly anticonvulsant hypersensitivity syndrome).
Inflammatory diseases can also present with fever and maculopapular rash. Systemic juvenile idiopathic arthritis (SJIA, Still disease) classically presents with an evanescent, salmon-colored macular rash on the trunk and proximal extremities that coincide with fever spikes (see Chapter 44 ). Many of the hereditary periodic fever syndromes manifest with macular, maculopapular, or urticarial rashes associated with fever (see Chapter 54 ).
Extravasation of red blood cells from the vasculature into the skin produces petechiae and purpura. These lesions do not blanch with applied pressure. Petechiae are pinpoint lesions (<3 mm). Purpura are larger lesions and can be either palpable or nonpalpable. While the majority of patients with fever and petechiae have a benign illness, their presence, especially in a child younger than 24 months, is of particular concern. Between 2% and 20% of affected patients have an underlying bacterial infection, and depending on the clinical setting, 0.5–10% have sepsis caused by Neisseria meningitidis . Other potentially serious infections signaled by a petechial rash and fever include bacterial endocarditis and Rocky Mountain spotted fever. Group A streptococcal (GAS) pharyngitis is the most common bacterial cause of fever and petechiae, with up to 20% of patients with fever and petechiae being diagnosed with GAS pharyngitis in some studies. Common viral causes include enterovirus and adenovirus. Febrile children may develop petechiae after coughing or vomiting; petechiae in this setting are almost always located in the superior vena cava distribution above the nipple line. Further, petechiae confined solely to the area above the nipple line is rarely associated with invasive bacterial disease. Noninfectious causes of fever and petechiae include drug eruptions and acute leukemia. Not all children with fever and petechiae have thrombocytopenia.
Diffuse purpuric lesions may be noted in a wide variety of disorders. These include infectious diseases associated with organisms with a predilection for vascular endothelium, such as N. meningitidis ( Fig. 53.6 ) and rickettsiae ( Fig. 53.7 ), uncommon bacterial diseases such as rat-bite fever ( Fig. 53.8 ) and Vibrio vulnificus or Brazilian purpuric fever caused by Haemophilus aegyptius , and a number of viral hemorrhagic fever diseases. Purpura is also associated with disseminated intravascular coagulation (DIC) and profound thrombocytopenia, such as in idiopathic thrombocytopenic purpura (see Chapter 51 ). Purpura followed by subsequent necrosis of skin is referred to as purpura fulminans , a severe, life-threatening condition that has been reported after relatively benign infections such as varicella or with more serious disorders (meningococcemia) ( Fig. 53.9 ). Purpura can also occur in the noninfectious vasculitides, such as Henoch-Schönlein purpura (HSP) and granulomatosis with polyangiitis. Discrete, raised purpuric lesions (palpable purpura) distributed predominantly over the buttocks and lower extremities are typical for this disorder. While bacteremia must be considered for all febrile patients presenting with diffuse or discrete purpuric lesions (see Figs. 53.6, 53.7, 53.8, and 53.9 ), patients with HSP are generally well-appearing but may have significant discomfort from arthritis or abdominal pain.




Vesicular rashes (sharply demarcated, raised lesions containing clear fluid), bullae (vesicles exceeding 1 cm in diameter), or pustules (raised lesions containing cloudy fluid composed of serum and inflammatory cells) may be suggestive of focal or disseminated infection with various pathogens or signal a serious drug reaction. Localized vesicles may suggest infection with herpes simplex virus (HSV) type 1 or 2 (especially if the vesicles are grouped on an erythematous base), varicella-zoster virus (especially if grouped vesicles are distributed in a dermatomal pattern) ( Fig. 53.10 ), or infection with nonviral pathogens, such as Rickettsia akari (the cause of rickettsialpox , a mouse mite–borne rickettsiosis found worldwide but common in New York City). Localized pustules and bullae are usually suggestive of pyodermas caused by Staphylococcus aureus , but pustular lesions distributed on the palms and soles in the context of fever may represent infective emboli with microabscess formation (Janeway lesions), which are often caused by S. aureus endocarditis.

Vesicles distributed in a more generalized pattern , especially with a concentration of lesions over the head and trunk in various stages of evolution, are suggestive of primary varicella-zoster virus infection ( chickenpox ). A more generalized pattern with a concentration over the extremities is suggestive of enteroviral infection, especially with coxsackievirus A16 ( hand-foot-and-mouth disease ), or A6 in even more severe presentations. Orthopoxviruses such as monkeypox, like smallpox, cause a systemic febrile rash illness with lesions that progress from papules to vesicles to pustules concentrated on the face and extremities. Acute generalized exanthematous pustulosis (AGEP) is a rare cutaneous hypersensitivity reaction characterized by numerous sterile pustules beginning on the face and spreading to the trunk and limbs. It typically presents within 24 hours after exposure to an offending drug, usually a β-lactam or macrolide antibiotic. The clinician evaluating the sexually active patient presenting with asymmetric generalized pustules or vesicopustular lesions should also consider disseminated infection with Neisseria gonorrhoeae . Diffuse vesiculobullae may be noted in Stevens-Johnson syndrome (SJS) or in toxic epidermal necrolysis (TEN), life-threatening mucocutaneous hypersensitivity diseases usually related to drugs.
Nodules (discrete, raised, firm, well-demarcated lesions without fixation to the overlying skin) may be associated with a number of underlying infectious or inflammatory disorders, such as polyarteritis nodosa and Sweet syndrome (acute febrile neutrophilic dermatosis). Red, pink, or plum-colored nodules distributed in a seemingly random manner over the skin surface may represent leukemic infiltrates. The subcutaneous nodules of acute rheumatic fever are usually located over bony extensor surfaces near tendons and are found in <5% of patients with acute rheumatic fever. They may also be found in patients with polyarticular JIA and dermatomyositis.
Erythema nodosum (erythematous and painful nodules usually distributed over the extremities) may be associated with viral infections including hepatitis B and C; bacterial infectious agents including group A β-hemolytic streptococcus (most common), chlamydia, Brucella species, and Yersinia species; mycobacterial infections; fungal infections, particularly Coccidioides immitis and less often Histoplasma capsulatum , Blastomyces dermatitidis, or Cryptococcus neoformans ; or drug reactions, especially in response to oral contraceptives and sulfonamides. Other noninfectious causes include SLE, sarcoidosis, and inflammatory bowel disease.
Ulcers are depressed lesions in which the epidermis and some or all of the dermis has been destroyed. In immunocompromised hosts, infection with HSV may manifest with shallow erosive or ulcerative lesions. In immunocompetent hosts, cutaneous ulcerations may be noted in noninfectious disorders associated with vasculitis, such as SLE, polyarteritis nodosa, and HSP.
Pyoderma gangrenosum and ecthyma gangrenosum are painful cutaneous ulcerative lesions with an erythematous, raised edge. The lesions usually begin as a papule and break down rapidly with central necrosis. It may be seen in immunocompromised patients, typically in the setting of neutropenia, often with systemic infections with bacterial pathogens (typically gram-negative), such as Pseudomonas aeruginosa or Stenotrophomonas maltophilia (ecthyma). In immunocompetent patients, the lesion may manifest in the context of inflammatory bowel disease (pyoderma gangrenosum), PAPA (pyogenic arthritis, pyoderma gangrenosum, acne), or rheumatoid arthritis. Digital ulcerations may be noted in patients with small-vessel vasculitis, such as SLE. Oral ulcerations may be noted in those with herpes simplex or coxsackievirus (hand-foot-and-mouth disease) or as a manifestation of Behçet disease, SLE, PFAPA (periodic fever, aphthous stomatitis, pharyngitis, adenitis), cyclic neutropenia, or inflammatory bowel disease.
Diffuse erythema ( erythroderma ) is associated with toxin-mediated disorders characterized by superantigen production. Bacterial superantigens cause nonspecific T-cell stimulation resulting in several acute rash-fever disorders, such as staphylococcal scalded skin syndrome (SSSS; Fig. 53.11 ), streptococcal scarlet fever, staphylococcal or streptococcal TSS, and possibly KD.

Localized erythema in the context of acute fever is strongly suggestive of cellulitis, erysipelas, or abscess. The presence of warmth, tenderness, and associated lymphangitis is highly indicative. Organisms causing cellulitis or abscess formation are usually inoculated directly into the skin as a result of trauma. However, bacteremic localization is well described among young children with preseptal or facial cellulitis associated with Haemophilus influenzae type b (pre– H. influenzae type b vaccine) or Streptococcus pneumoniae .
Patients with SLE or dermatomyositis may present with an isolated erythematous malar rash (butterfly rash), which is exacerbated by exposure to sunlight. The acute onset of intense “slapped-cheek” erythema of the face suggests erythema infectiosum, a recognizable exanthem caused by parvovirus B19, and should be differentiated easily from the malar rash of SLE, which usually manifests other characteristics, such as chronicity as well as hyperkeratosis and follicular plugging. In addition, patients with erythema infectiosum tend to have a maculopapular, lacelike rash over the arms, which may spread to the buttocks and thighs ( Fig. 53.12 ; see Table 53.6 ).

Patients with dermatomyositis may have localized lilac-colored lesions over the eyelids (heliotrope rash), which may be associated with periorbital edema. Such patients characteristically, but not invariably, have an erythematous, scaly eruption on the face, neck, knees, elbows, and phalanges. When the rash is localized over the knuckles, it resembles dripped wax and has been referred to as Gottron papules. Patients with autoinflammatory disorders (periodic fever syndromes) may present with localized erythema or fasciitis (see Chapter 54 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here