Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Fetal platelet disorder is a potentially life-threatening condition.
Fetal thrombocytopenia may lead to fetal bleeding. complications, such as an intracranial haemorrhage.
Idiopathic thrombocytopenic purpura.
Has an incidence of 1 to 2 in 1000 pregnancies.
Causes severe fetal thrombocytopenia in 5% to 20% of the cases.
Rarely leads to bleeding problems in fetuses or neonates.
Is treated primarily with corticosteroids.
Fetal and neonatal alloimmune thrombocytopenia.
Occurs in 1 in 1000 pregnancies.
Is mainly caused by human platelet antigens 1a (80%) and 5b (10%) in Caucasians.
Causes severe bleeding complications in 10% of cases of severe thrombocytopenia.
Treatment should be noninvasive with intravenous immunoglobulins.
Population-based screening would mean a major improvement in the prevention of bleeding complications.
Fetal platelet disorders, causing fetal thrombocytopenia, are relatively rare but potentially life-threatening conditions. During normal fetal life, the platelet count progressively increases, and reaches a level of approximately 150 × 10 9 /L by the end of the first trimester. The normal range for platelet counts in healthy fetuses and neonates is equal to that of adults (150–450 × 10 9 /L). Therefore fetal and neonatal thrombocytopenia is defined as a platelet count less than 150 × 10 9 /L regardless of gestational age, which corresponds with values below the fifth percentile, calculated in adults. The degree of the thrombocytopenia can be further classified to mild (100–150 × 10 9 /L), moderate (50–100 × 10 9 /L) or severe (<50 × 10 9 /L). In contrast to neonatal thrombocytopenia, the exact frequency of fetal thrombocytopenia is unknown. Of all newborns, 1% to 2% have a platelet count below 150 × 10 9 /L and 1 to 2 of 1000 newborns have a severe thrombocytopenia.
The risk for fetal thrombocytopenia is the development of bleeding complications, varying from harmless skin bleeds to internal organ haemorrhage, intracranial haemorrhage (ICH) or even perinatal demise. These complications mostly present after birth, and a diagnosis of a fetal platelet disorder occurs postnatally in the vast majority of cases. Therefore preventive measures can only be taken in subsequent pregnancies ( Table 41.1 ).
| Increased destruction |
|---|
| Immune thrombocytopenia |
|
|
|
|
| Peripheral consumption |
|
|
|
|
| Decreased production |
|---|
| Genetic disorders (TAR syndrome, trisomy 13,18,21, triploidy, Turner syndrome, amegakaryocytosis, Wiskott-Aldrich syndrome, May-Hegglin syndrome, Bernard-Soulier syndrome, Alport syndrome) |
| Bacterial infection (GBS, E scherichia c oli , Listeria spp., syphilis) |
| Viral infection (CMV, parvovirus, rubella, HIV, HSV) |
| Parasite infection (toxoplasmosis) |
| Asphyxia |
| Placental insufficiency (preeclampsia, IUGR, diabetes, premature birth) |
Nonimmune conditions that are associated with fetal and neonatal thrombocytopenia act through increased destruction of platelets as well as a decreased production. Non–immune-mediated increased destruction or consumption can be caused by disseminated intravascular coagulation (DIC), thrombosis, Kasabach-Merritt Syndrome or hypersplenism. Through increased destruction, placental insufficiency (premature birth, preeclampsia, intrauterine growth restriction, diabetes), several genetic abnormalities, infection and asphyxia can lead to fetal and neonatal thrombocytopenia.
Because immune-mediated fetal platelet disorders are the most important cause of severe fetal thrombocytopenia, responsible for one third of all neonatal thrombocytopenia cases, this chapter focuses on idiopathic thrombocytopenic purpura (ITP) and fetal and neonatal alloimmune thrombocytopenia (FNAIT). Also, through an unknown mechanism, a small proportion of cases with severe fetal anaemia caused by red blood cell (RBC) alloimmunisation is associated with fetal thrombocytopenia.
Maternal thrombocytopenia is encountered regularly, complicating 1 in 12 pregnancies. The most common cause of maternal thrombocytopenia is a benign transient condition called gestational thrombocytopenia, accounting for approximately two thirds of all cases of maternal thrombocytopenia; ITP accounts for 3%. Other causes of maternal thrombocytopenia are preeclampsia, HIV, systemic lupus erythaematosus and thyroid dysfunction.
There are two different types of ITP: the acute form and the chronic form. Acute ITP is predominantly a condition of childhood that seldom occurs in pregnancy. It is mostly preceded by a viral infection and is caused by cross-reactivity between viral antigens and platelet antigens. This form usually resolves within weeks or months. ITP in pregnancy is therefore almost always chronic ITP, with an incidence of 1 to 2 in 1000 pregnant women.
Chronic ITP is an autoimmune disorder caused by the maternal production of antibodies against glycoproteins present on the membranes of maternal platelets. The majority of these autoantibodies are of the immunoglobulin (Ig) G class and are thus able to cross the placental barrier, bind to fetal platelets and cause fetal thrombocytopenia. The reported incidence of severe neonatal thrombocytopenia in ITP varies between the 5% and 20%. Although these numbers vary widely among studies, none of them reported any significant bleeding problems in neonates as a result of the ITP. No cases of severe in utero bleeding have been documented, and the reported incidence of ICH is low and varies between 0% and 1.2%. The lowest platelet count in the affected newborns mostly occurs within 7 days after birth.
In pregnancy, maternal platelet counts are usually lower than before. Maternal symptoms can vary from none to severe haemorrhaging but are usually mild, and pregnant women seem to have a greater tolerance to ITP compared with nonpregnant women because of the procoagulant state in pregnancy.
Unfortunately, no reliable pregnancy-specific parameters exist to predict the severity of fetal thrombocytopenia in ITP. The maternal platelet count, nor IgG level seems to correlate with the fetal platelet count. The strongest correlation found so far is the lowest platelet count in older siblings. The only maternal factor identified to predict a low platelet count in affected neonates is a history of splenectomy.
The diagnosis of ITP is one of exclusion, other causes of thrombocytopenia during pregnancy (e.g., preeclampsia, gestational thrombocytopenia, HELLP (haemolysis, elevated liver enzymes, low platelet count) syndrome, DIC, massive obstetric haemorrhage or acute fatty liver syndrome) need to be ruled out first. The distinction between gestational thrombocytopenia and the first presentation of ITP may be particularly difficult. Differences are the gestational age at detection and platelet count. ITP is usually detected in early pregnancy because the condition is present before conception, and it usually has a lower platelet count than gestational thrombocytopenia. In addition, an elevated mean platelet volume, implicating increased platelet production, can support the diagnosis. Bone marrow examination is not performed during pregnancy but would reveal normal or elevated megakaryocytic numbers. Thrombopoietin (Tpo) level can be used to distinguish platelet production disorders from platelet destruction disorders. In ITP, Tpo levels are normal or slightly elevated in contrast to significant elevation of Tpo levels in patients with platelet production disorders.
Autoantibodies can be identified using a platelet immunofluorescence test (PIFT), which is based on the detection of platelet-bound antibodies. Unfortunately, it has a relatively low sensitivity of 70% in patients with ITP. Positive reactions can be identified in case of greater than 1000 molecules of IgG bound to a platelet; 450 molecules can already cause platelet destruction. Also, in some patients with ITP, destruction of platelet can be T cell mediated, so platelet-bound antibodies will not be measurable.
Idiopathic thrombocytopenic purpura is not a reason to discourage pregnancy; however, women with severe thrombocytopenia despite a splenectomy and high doses of corticosteroids are at high risk for complications and should have extensive preconception counselling about possible risks. When planning pregnancy, it is wise to optimise treatment before conception, mainly to assess the need for splenectomy before pregnancy.
Management of IPT during pregnancy requires a multidisciplinary approach, with a team including a haematologist, paediatrician (neonatologist), obstetrician and anaesthetist. A complete overview is displayed in Fig. 41.1 .
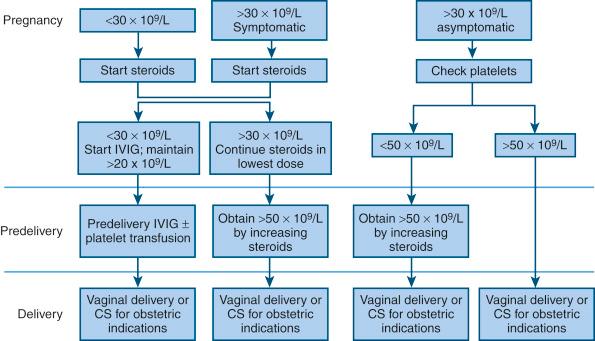
During pregnancy, there are three indications for starting treatment: symptomatic women, a platelet count below 30 × 10 9 /L or the need for a higher platelet count before a procedure (e.g., caesarean section).
When platelet counts are higher than 30 × 10 9 /L, no treatment is necessary, and monitoring of maternal platelet counts needs to be performed every 2 weeks and more closely as delivery approaches.
First choice of treatment during pregnancy is similar to the approach in nonpregnant women, prednisone started at a dosage of 1 to 2 mg/kg/day and then tapered to find the minimal effective dose. If the thrombocytopenia shows to be resistant to corticosteroid treatment with prednisone or in case of serious side effects, intravenous infusion of immunoglobulins (IVIG) is next in line. Other treatments with limited evidence for their efficiency in ITP during pregnancy are intravenous anti-D infusion, splenectomy and azathioprine. Rituximab, danazol, Tpo receptor agonists and most other immunosuppressive drugs should not be administered during pregnancy because of possible teratogenicity. Platelet transfusions are only to be administered in very severe thrombocytopenia (platelet counts <20 × 10 9 /L) and at times when there is a high risk for bleeding.
Maternal platelet counts above 50 × 10 9 /L are considered to be safe for vaginal as well as caesarean delivery. Therefore, if predelivery platelet counts are below 50 × 10 9 /L, IVIG treatment should be administered at a dose of 0.8 kg/day. Although guidelines can differ among countries and centres, a platelet count above 80 × 10 9 /L is considered safe for epidural analgesia. Treatment during pregnancy does not seem to have any effect on fetal platelet counts or the occurrence of neonatal bleeding problems; it should be administered for maternal indications only.
Initially, the management of labour and delivery in ITP patients was based on the concerns of ICH in the thrombocytopenic neonate, secondary to vaginal birth trauma. Therefore fetal scalp blood sampling or cordocentesis was performed, and caesarean delivery was preferred when fetal platelet count was below 50 × 10 9 /L. Fetal scalp blood sampling appeared to yield falsely low counts, and predelivery cordocentesis, although producing reliable fetal platelet counts, has a significant risk for fetal loss and severe morbidity. In combination with the low incidence of perinatal bleeding, these should not be performed as routine procedures in patients with ITP. The route of delivery (vaginal or caesarean section) does not seem to affect the incidence of ICH; therefore, caesarean section in patients with ITP should only be performed for obstetric indications. Interventions such as fetal scalp blood sampling and vacuum extraction should be avoided during delivery.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here