Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Compartment syndrome occurs when pressure within a fibroosseous space increases beyond a level that is suitable for perfusion across tissues.
The most common cause of forearm compartment syndrome is fracture, especially distal radius fracture. Other causes of compartment syndrome include an injection injury, an extravasation injury, a penetrating trauma, circumferential burns, and snake or insect bites.
Injection injuries involving air, water, or other hydrophilic liquids can potentially be observed depending on the volume and clinical presentation.
Injection of paint or other oil-based liquid requires early decompression and additional debridement as needed. Although seemingly benign, these injection injuries tend to develop ischemia and deep space infections if left untreated.
Ischemia-reperfusion occurs after prolonged tourniquet time and with the use of compressive wraps and casts.
Crush injury with resultant edema leads to increased pressure in the closed muscle space and can also progress to compartment syndrome.
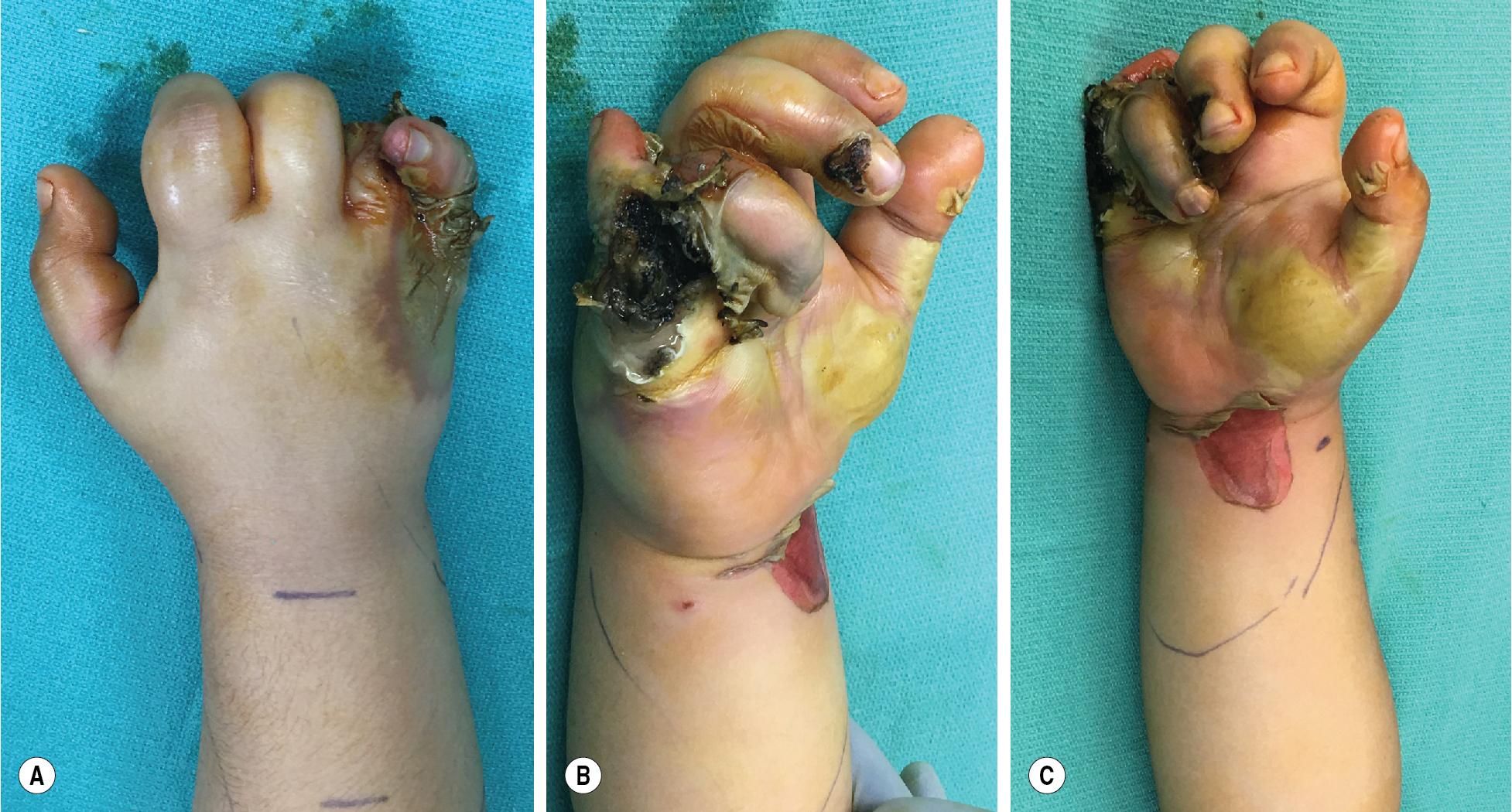
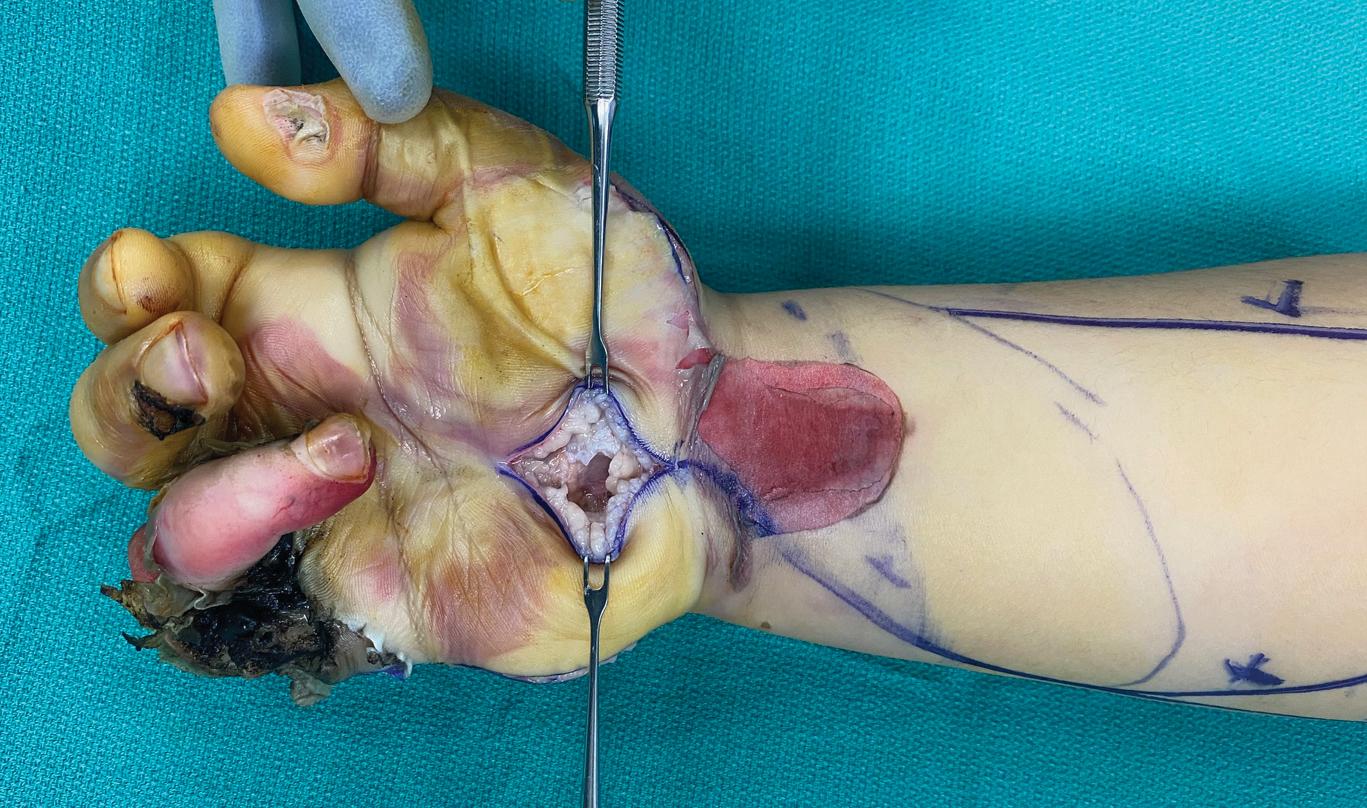
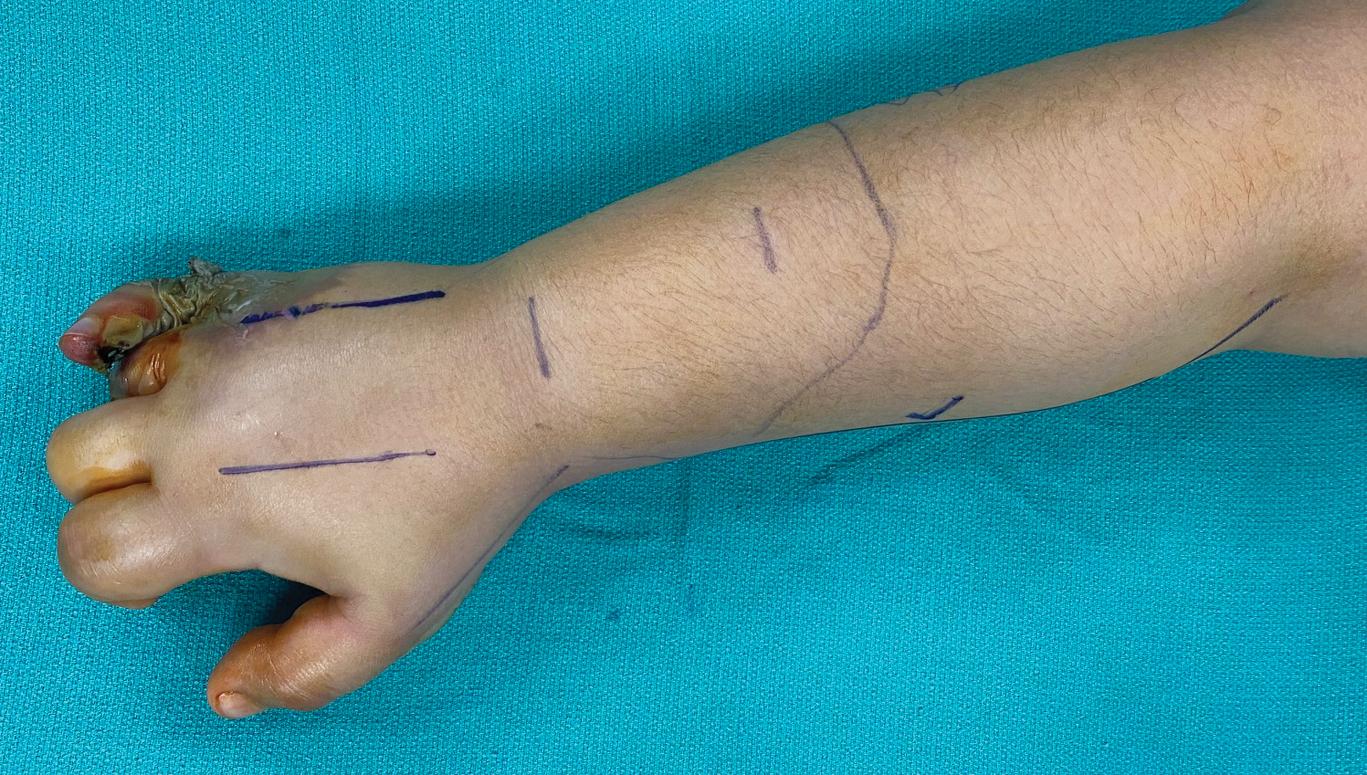
Electrical injury, a type of burn injury, can also cause compartment syndrome when the hands and upper limbs are damaged by a high-voltage current. Unlike thermal damage caused by eschar compression, which requires escharotomy, the deep tissue necrosis and swelling caused by electrical burns leads to increased compartment pressure. This can only be treated with fasciotomy.
In most cases, the upper extremities are the points of contact with the power source and are likely to require amputation. Although the timing of debridement does not reduce amputation rates, the boundary between healthy and damaged tissue is often unclear initially. Early debridement is important to reduce secondary necrosis from infection.
Multiple debridement procedures are often required to determine the extent of damage and the need for amputation. It is necessary to return to the operating room every 24 to 48 hours to reassess the viability of the tissue and repeat the debridement.
Immediate surgery is necessary if the patient has progressive neurologic dysfunction, vascular compromise, compartment syndrome, or systemic clinical deterioration from suspected ongoing myonecrosis.
The ischemia caused by compartment syndrome affects the nerves and muscles; irreversible damage can occur within 6 hours for muscle and in even less time for nerves.
The diagnosis of compartment syndrome is generally a clinical one, based on findings of nerve or muscle injury.
Pain (out of proportion to injury, especially on passive stretch), paresthesia, paralysis, pallor, pulselessness, and inability to regulate limb temperature (poikilothermia) are common manifestations.
Pain out of proportion to injury and paresthesias are the two earliest findings, whereas pulselessness and pallor are often seen later or may not occur at all.
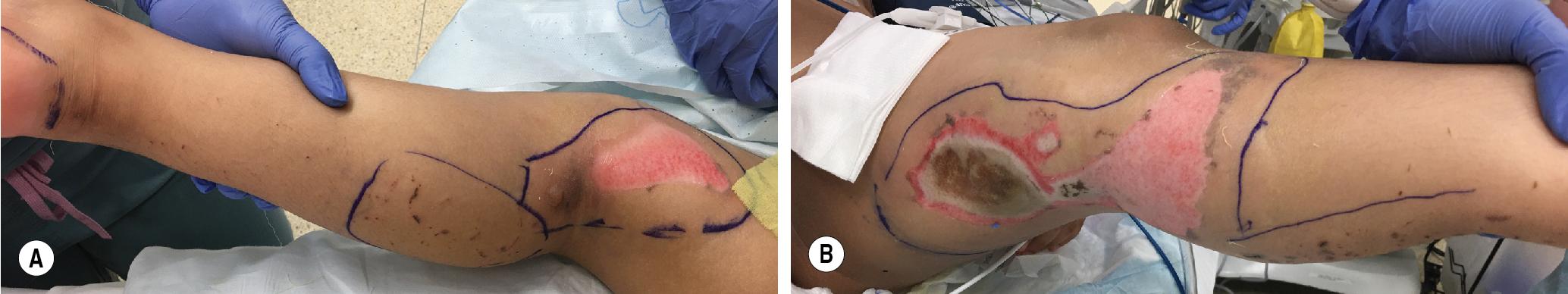
The compartments are often firm to palpation, and overlying skin may become shiny and even develop blisters ( Figs. 2.1 and 2.2 ).
For patients with electrical injuries, it is important to put forth the caveat of life before limb because the heart and kidneys may be affected by electric shocks. The patient’s general condition should be evaluated first, and limb salvage surgery should be performed once the patient is stable from a trauma standpoint.
Do not be deceived by the superficial appearance of skin burns after electrical injury because deep tissue damage is often serious and harder to evaluate on examination ( Fig. 2.3 ).
When an electric current passes through the body, the extent of damage to each tissue type depends on its inherent resistance. Bone is the most resistant to electric current, followed by fat, tendons, and skin. Muscles, blood vessels, and nerves are the least resistant.

Often, the diagnosis is clinically apparent, and therefore no additional imaging or other workup is needed.
Most commonly, the diagnosis in less clinically apparent cases is made by measuring the intramuscular pressure (IMP). Many techniques have been described, including arterial line transducer systems, slit catheters, and self-contained measuring systems.
Single pressure measurement does not reflect pressure changes over time and has limited significance for clinical diagnosis. Continuous pressure examination is the current gold standard for the diagnosis of acute compartment syndrome.
Normal tissue pressures range from 0 to 8 mm Hg. A compartment pressure measurement over 30 mm Hg is typically an indication for urgent fasciectomy; readings of 20 or more warrant very close monitoring and possibly surgical intervention under the right clinical circumstances. Additionally, some consider a difference of ≥20 mm Hg between diastolic pressure and compartment pressure as an indication for fasciotomy as well (hypotensive/septic patients).
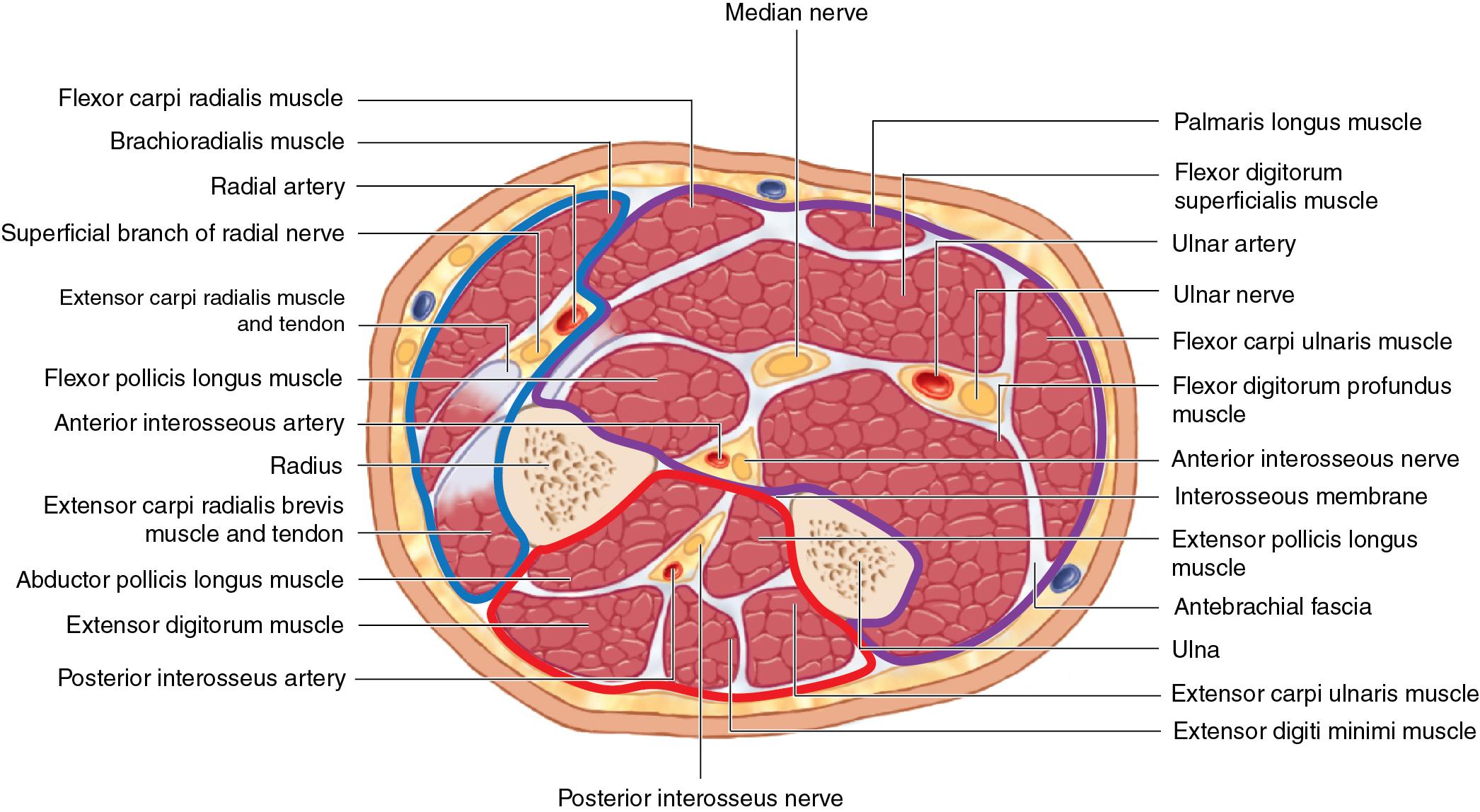
The forearm has four major compartments—superficial volar, deep volar, dorsal, and lateral (mobile wad) ( Fig. 2.4 and Table 2.1 ).
The interosseous membrane of the radius and ulna separates the forearm into volar and dorsal compartments. The deep volar compartment is most susceptible and most often affected by compartment syndrome, whereas the mobile wad (more superficial) is least commonly involved. Pronator quadratus belongs to the deep volar compartment, too. Some investigators consider it to be a separate subcompartment because it can be affected independently from other forearm muscles.
When compartment syndrome occurs in the volar compartment, it can be devastating to forearm function because the median nerve, anterior interosseous nerve (AIN), and the ulnar nerve run within it. The median nerve is the most common damaged nerve. AIN runs on the superficial side of the deep fascia and innervates the deep flexor muscle.
The dorsal compartment is not as frequently injured compared with the volar compartment.
| Compartment | Muscle | Artery | Nerve | |
|---|---|---|---|---|
| Arm | Anterior Posterior Deltoid |
Biceps, brachialis, coracobrachialis; Triceps Deltoid |
Brachial Profunda brachii — |
Musculocutaneous Radial Axillary |
| Forearm | Volar Superficial Deep Dorsal Superficial Deep Mobile wad |
Pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis, flexor carpi ulnaris; Flexor pollicis longus, flexor digitorum profundus, pronator quadratus; Extensor digitorum communis, extensor digiti minimi, extensor carpi ulnaris; Abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, extensor indicis proprius, supinator; Brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis; |
Radial and ulnar Pos. interosseous — |
Median, ulnar, and anterior interosseous Pos. interosseous Radial |
| Hand | Thenar Hypothenar Adductor Interosseous Carpal tunnel Digit |
Abductor pollicis brevis, opponens pollicis, flexor pollicis brevis; Abductor digiti minimi, opponens digiti minimi, flexor digiti minimi; Adductor pollicis; Four dorsal and three palmar interosseous muscles; Flexor digitorum profundus, flexor digitorum superficialis, flexor pollicis longus. |
Digital — — — — Digital |
Recurrent motor Ulnar Ulnar Ulnar Median Digital |
The carpal tunnel is susceptible to compressive pressures and is often released when other upper extremity fasciectomies are performed.
The compartments of the hand that have the most clinical significance and most often require release include the thenar, hypothenar, adductor pollicis, dorsal interosseous, and volar interosseous.
Digital compartments are bound by Cleland and Grayson ligaments, although the clinical significance of these compartments in the setting of compartment syndrome is debated.
For high-pressure injection injuries, the surgical approach may need to be adjusted to allow for adequate debridement of ischemic tissue in the area of injection.
Forearm
Volar release is traditionally done via a curvilinear incision from the medial epicondyle to the proximal wrist crease. This, however, places the distal flexor tendons and median nerve at risk for exposure and desiccation. Therefore we advocate for an alternative approach.
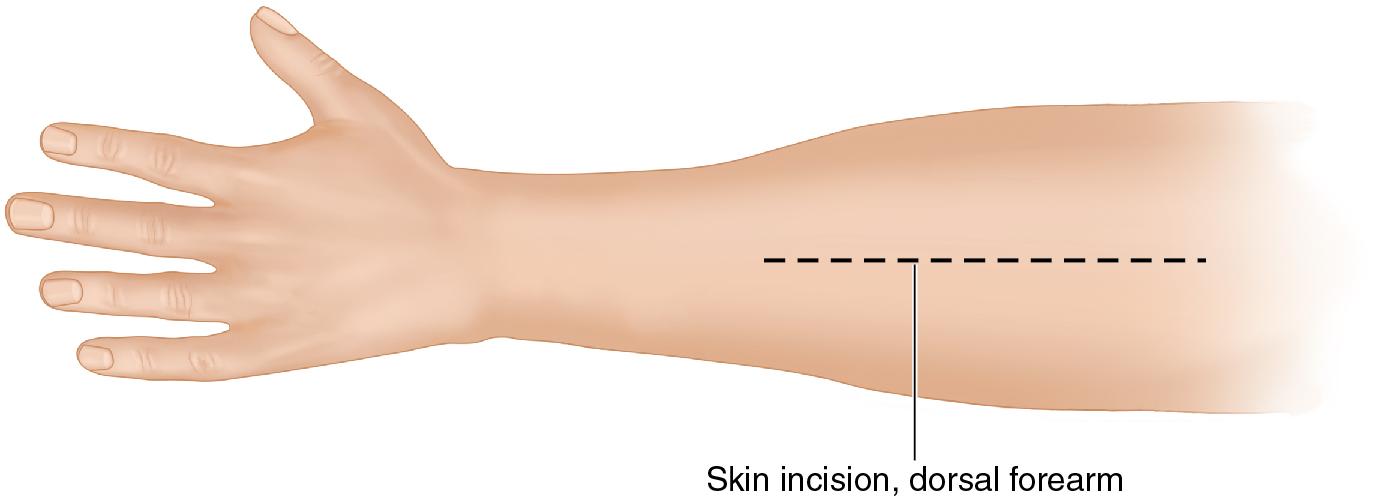
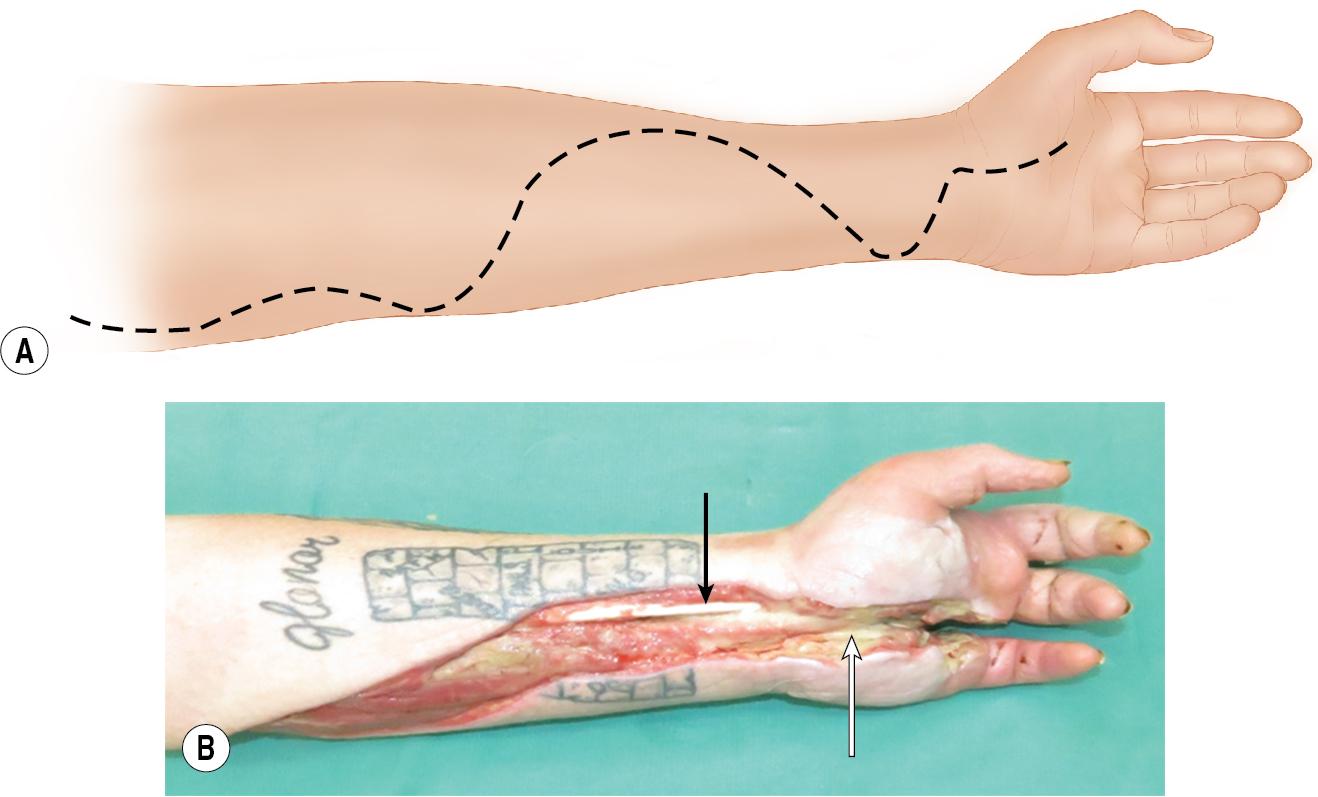
We recommend two longitudinal incisions—one over the volar radial aspect (over the flexor muscles) and the other over the dorsal ulnar aspect of the extensor muscles. This approach decompresses the volar and dorsal compartments without exposing the median nerve or distal forearm tendons ( Figs. 2.5 and 2.6A–B ).
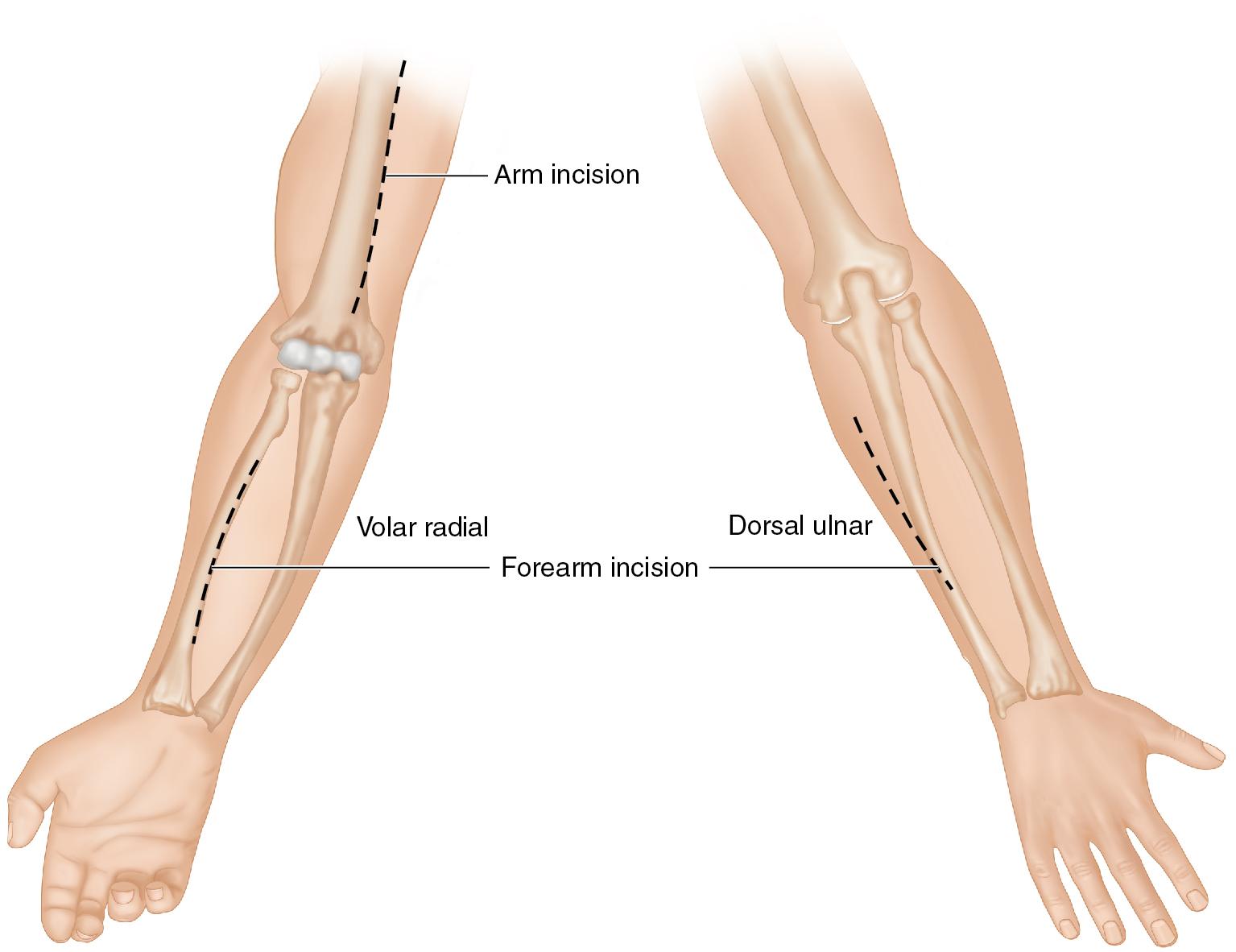
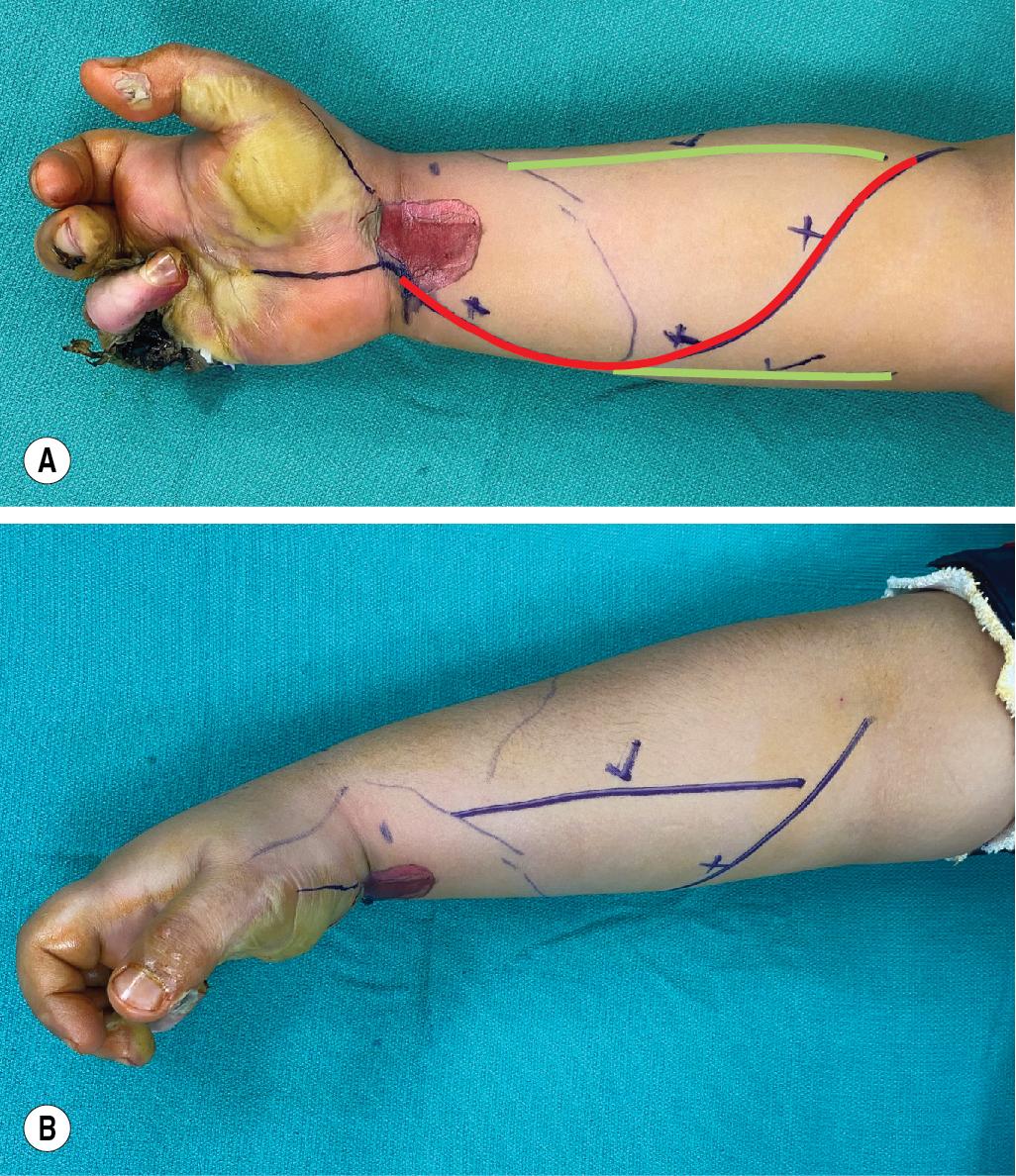
The more traditional dorsal release is performed via a single longitudinal incision along a line between Lister tubercle and an area 4 cm distal to the lateral epicondyle (incision is made in the space between extensor digitorum and extensor carpi radialis brevis; Fig. 2.7 ). This incision facilitates dorsal release; however, a more limited incision shown in Fig. 2.5 and Fig. 2.6A–B will provide adequate exposure and minimize wound morbidity.
Hand
The carpal tunnel is approached via a single incision between the thenar and hypothenar spaces, in line with the radial aspect of the ring finger ( Fig. 2.8 ).
The thenar compartment is approached via an incision along the radial side of the thenar eminence between glabrous and nonglabrous skin ( Fig. 2.9 ).

The hypothenar compartment is released via a longitudinal incision along the ulnar aspect of the palm ( Fig. 2.10 ).

Dorsal hand compartments are released by two longitudinal incisions parallel and radial to the index and ring finger metacarpals ( Fig. 2.11 ). This facilitates decompression of all four dorsal interosseus compartments ( Fig. 2.12 ).

Finger
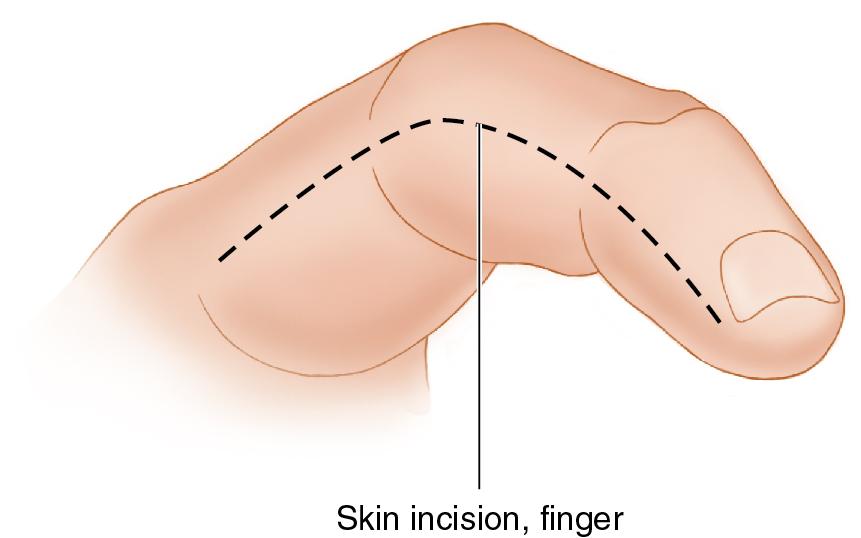
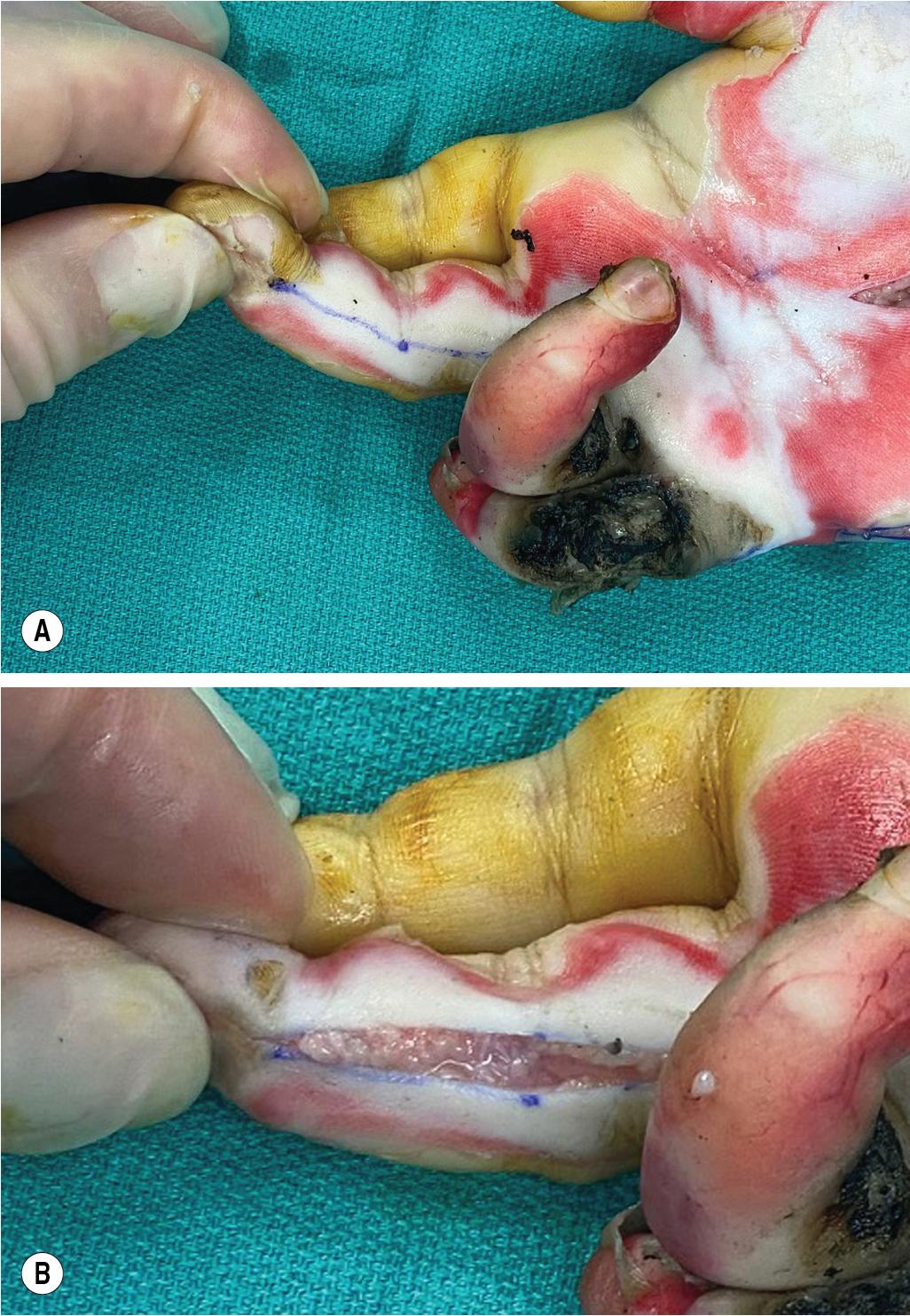
Decompression can be done with a midaxial incision along the noncontact (radial for index and thumb; ulnar for middle, ring, and small) side of the finger ( Figs. 2.13 and 2.14 ).
Hypothenar compartment release should not be done directly on the ulnar border, but instead should be slightly radial to the border, so that the scar is not on a direct pressure area of the hand.
When decompressing the median nerve at the carpal tunnel, avoid incising across the wrist because this can increase the risk for wound dehiscence, with swelling and subsequent exposure of the median nerve and flexor tendons.
It is not necessary to make release incisions distal in the midvolar forearm to expose the median nerve or distal flexor tendons because this could cause desiccation and necrosis of these vital structures. Avoid these exposure approaches whenever possible ( Fig. 2.15A–B ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here