Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() For video accompanying this chapter see ExpertConsult.com . See inside cover for access details.
For video accompanying this chapter see ExpertConsult.com . See inside cover for access details.
Our face is our most inextricable sense of self. A person’s self-image and self-esteem are powerfully influenced by their appearance. People requesting a facelift are aware of loss of confidence as a result of their altered “look.” The way people are “judged” and treated by others, whether supportive or discriminatory, is largely determined by others’ perception of their character and personality, so often fallaciously based on first impressions from their facial appearance. This aspect places a significant responsibility for the facelift patient’s future psychological wellbeing in the hands of the surgeon, an added dimension, for which trainees are usually not prepared, but which they must quickly appreciate.
The myriad of possible facelift surgery techniques reflects two separate considerations in the evolution of the field. First, the unique subjective, esthetic, and artistic elements that distinguish surgery of the face from more objective measures-riven fields, such as microsurgical patency. Second, and more importantly, the lagging understanding of the anatomical basis of facelift technique. By contrast, the anatomy of the hand, recognized by plastic surgeons as being complex, is more overtly functional and most of the detail was defined during the classical era of anatomy. In facelift surgery the empirical techniques preceded, what is only now becoming, an almost complete and nuanced understanding of the functional anatomy, as well as the anatomicopathological basis of the aging face. Skoog’s insightful advance into anatomically-based rejuvenation along with the description of the superficial musculoaponeurotic system (SMAS) were the start of this journey. , The work on the functional, as well as anatomical, basis of the more recently defined sub-SMAS spaces of the face and role of the facial ligaments as well as aging of its skeletal foundations has created a detailed surgical roadmap to safe, natural, and lasting facelift surgery outcomes. This is the holy grail of facial rejuvenation and this clarification in thinking around the anatomical basis of facelift surgery is being reflected in the availability of cadaver dissection courses and the training of the younger generation of plastic surgeons.
Considerations of esthetics in appearance are paramount. While facelift surgery is inherently a technical exercise, the importance of the surgeon’s esthetic eye cannot be overlooked as it is a critical, although intangible, factor in the outcome ( Fig. 66.1 ). Facelift patients in general have a more advanced visual esthetic than the young technical surgeon, who does not intuitively have, or yet developed, this level of esthetic appreciation. Just as a young musician learns by listening to music, the young plastic surgeon must cultivate the habit of analysing faces. Without nuanced understanding of what looks attractive and why, the practitioner of esthetic surgery does not have an appreciation of the specific outcome to be aimed for.

This chapter will give the reader an overview of the subject. Overlapping aspects are covered in the relevant preceding chapters on facial aging and lower eyelid rejuvenation. The senior author’s evolved approach to facelift surgery is laid out.
The face is a complex three-dimensional structure based on a solid skeleton containing three large apertures (the orbits and the extensive oral cavity). The openings of these cavities are closed by the dynamic sphincter muscles of the eyelids and lips, whose effect is modified by ancillary levator muscles of the lids and brows, and by the levator and depressor lip muscles. Supporting soft tissue volumes are held together by visible and invisible ligamentous extensions upon which our interaction in life, emotions, and expressions is played out. Genetics and time take their toll on our appearance modified by environment, lifestyle, and ultimately, gravity. A tired look with wrinkles, a changed shape of the face with sagging into jowls, and a loose hanging neck are the exacting toll of life’s vectors on the face. The logical way to start thinking about the face is that its aging is related to its function based around the skeletal apertures, located on the front of the face. The same muscles are used for communication by voice or facial expression. The lateral part of the face by contrast, being remote from the cavities, is more a platform for the structures of mastication, and has less aging as it is relatively fixed, requiring less mobility.
The original surgical techniques, from the early 1900s, were limited to the skin envelope. The improvements in a person’s aging look seemed remarkable because such a change had not been possible before this time. To be tackling facial appearance was bold surgery, even if addressing laxity of the facial skin was not. With success, the procedures evolved over the years with progressively more undermining and redraping of the facial skin. The risks were few, mainly to do with bleeding, skin circulation, and visible scars.
Deeper contouring surgery commenced only in the 1960s, with direct submental lipectomy introduced by Millard. Profound results were obtained in this era preceding liposuction. The modern facelift era commenced in the mid 1970s with Skoog’s revolutionary “anatomical” approach in which the flap is in a deeper plane. Then, Mitz and Peyronie’s seminal 1976 paper on the anatomical details of the superficial fascia introduced the important concept of the superficial musculoaponeurotic system (SMAS). Skoog’s was the first sub-SMAS dissection plane facelift. It took over a full decade after the SMAS description before the potential benefit of the SMAS was to be realized by mobilizing the SMAS of the anterior face. This required the release of the strong attachment of the SMAS to the zygoma. Furnas later described these attachments as part of a system of named retaining ligaments, that attach the facial soft tissues to the skeleton in between areas of mobility. Even now, 30 years on, understanding how to use the SMAS and retaining ligaments to best advantage is ongoing. ,
The soft tissue volume changes reflect the atrophy of normal aging, possibly accelerated by weight loss as well as “shrinkage” of skeletal projection, particularly of the perioral “dental” bones and dentition. The recent advent of soft tissue fillers and lipofilling has turned attention towards the role of correcting soft tissue atrophy of both subcutaneous fat compartments, and deeper sub-SMAS spaces, as an alternative to surgical lifting. The recent history of adding volume mirrors the earlier era of subcutaneous hydrocarbon (paraffin) injections, from the early 1900s, whose popularity well exceeded surgical correction for a time. Volume addition can achieve tissue tightening according to the location on the face, e.g., directly on the skeleton, and in proportion to the volume placed. To lift sagging tissue by this form of tightening is a greater challenge, although in the midcheek it may compete with surgical lifting. The appropriate method of correcting a person’s aging tissue laxity, must be individualized.
The earliest facial rejuvenation surgery, at the beginning of the 20th century, consisted of the simple excision of carefully-located and shaped ellipses or half-moons of skin at the back of the face (hairline, pretragal). These were performed under local anesthesia without undermining and direct closure was performed with controlled skin tension. Multiple sessions were often involved. By the late 1920s the additional benefit of undermining the skin for a short distance was appreciated. Interestingly, even then with this small advance in technique a pattern was emerging, acknowledging the advance as being “too much for the would-be surgeon.” Similarly, poor facelift results were being seen, with an unnatural appearance resulting from tightly stretched skin.
Modern subcutaneous lifting commenced in the 1930s as a result of linking the multiple skin excisions with a continuous incision, along with the release of subcutaneous attachments. These tentative first steps in facelifting progressed with surgical experience. Increased demand resulted from the increased social affluence of the post-World War Two years and general medical progress, with the advent of antibiotics and improved anesthesia. A rather standard technique evolved consisting of the dissection of large, random pattern skin flaps of the cheek and jowls with redraping in a superolateral suspension vector and resection of excess skin. To improve the cheek correction, the extent of skin flap dissection was progressively extended towards the nasolabial fold, usually, but not always, stopping a few centimeters short of this landmark. The extension of undermining over the lower zygoma has been more of a challenge, due to the difficulty of subcutaneous dissection in this area along with more bleeding. The reason was subsequently found to be due to the fibrous extensions of the zygomaticocutaneous ligament, the strongest of the osteocutaneous ligaments, which continue through the SMAS and divide in the subcutaneous layer as they extend to the dermal attachments. Below the mandible the extent of undermining has continued into the neck towards the midline to a variable extent without this ligamentous difficulty.
Following satisfactory hemostasis, with appropriate tension applied to the skin flaps, the excess skin is marked and key sutures placed before trimming the redundant skin and closure of the incisions, with or without drains. A thin face with modest skin laxity and/or excess, and indeed revision facelifts, may be appropriate cases where a subcutaneous technique can still be considered.
There are innumerable variations in the extent of subcutaneous undermining. The dermal attachments are not uniform across the face as first assumed, but reflect the underlying pattern of facial ligamentous attachment. This is the rational basis for deciding the extent of surgical release. The depth level of dissection within the subcutaneous layer is also varied according to the surgical objective. A superficial subcutaneous dissection has the advantage of being the most remote from the facial nerve branches, hence minimizing the risk of facial nerve damage. This can be important where the subcutaneous layer is thin, as over the temple, particularly in the elderly, where there may be less than usual protection of the underlying temporal branches of the facial nerve. The nerves are at greater risk in secondary facelifts, due to their fixation by fibrosis from previous surgical intervention, and especially when this is more than usual, for example, as a result of previous hematoma.
When a separate SMAS flap is planned, it is beneficial to leave most of the retinacula cutis (in the subcutaneous layer) attached to the SMAS, as this fibrous component reinforces the strength of the SMAS flap. A meticulous dissection technique is required with superficial subcutaneous dissection to avoid visible irregularities and damage to the dermal circulation.
Otherwise, a deep level of subcutaneous dissection is preferred, especially when the surface of the SMAS is to be exposed preliminary to superficial SMAS, platysma manipulation techniques. It is considerably easier to perform the dissection at the deep subcutaneous level and with less bleeding, although the plane is closer to the nerves. This level of dissection has been named the superficial musculoaponeurotic plane (SMAP). When this plane of dissection is continued in front of the zygoma, directly on the surface of orbicularis oculi, direct access is provided to the malar fat pad. The malar fat pad is the discrete mass of thicker subcutaneous fat of the anterior cheek, whose inferior descent forms the volume of the nasolabial fold. Specific suture suspension of the malar fat pad provides a controlled correction of the medial cheek/nasolabial fold contour, but at the expense of prolonged postoperative edema.
The skin flap technique remains popular with some surgeons owing to its surgical “simplicity,” and safety, being remote from the structure of the face. The benefits are touted as short operative time with relatively speedy recovery, and relatively satisfactory early postoperative results. There are inherent long-term shortcomings with the technique as a consequence of the viscoelastic properties of skin, making it less than ideal for taking tension. As a consequence, facial shape cannot be maintained by tightening the skin envelope alone. Additional manipulation of the underlying parenchyma is required, as in other plastic surgery procedures, most notably breast reductions. Other inherent limitations when depending on direct skin tightening include a propensity to skin flap necrosis, traction effect on the pinna, and scar widening.
Originating with Skoog’s technique and the subsequent anatomical description of the SMAS by Mitz and Peyronie, it became evident that utilization of the underlying SMAS was the key to controlling the tension on the skin closure. This was the first accepted benefit of SMAS surgery. It took many years, with further anatomical studies and improved understanding of the potential of the SMAS, along with multiple evolutions of the technique of SMAS correction, for it to be appreciated as the tool for reshaping the face as well as for providing more lasting outcomes. , ,
The original version of this technique was to first perform a standard, skin-only facelift dissection and then perform a SMAS incision located directly beneath the facelift incision to mobilize the SMAS, as a completely separate layer. However, dissection of the thin SMAS flap in the preauricular area is inherently difficult due to the absence of a natural cleavage plane as the SMAS has a strong adherence to the parotid capsule ( fixed SMAS ), which Furnas named the platysma auricular fascia. The early SMAS mobilizations were limited in extent to the anterior border of the parotid, as advised by Mitz and Peyronie, the focus being on avoiding the risk of damage to the facial nerve branches as they emerge from the parotid. It became appreciated that to satisfactorily tighten the medial cheek and jowl it is necessary to extend the SMAS release into the mobile SMAS forward of the parotid capsule and release the SMAS from the restraining effect of the vertical line of masseteric cutaneous ligaments ( Fig. 66.2 ).
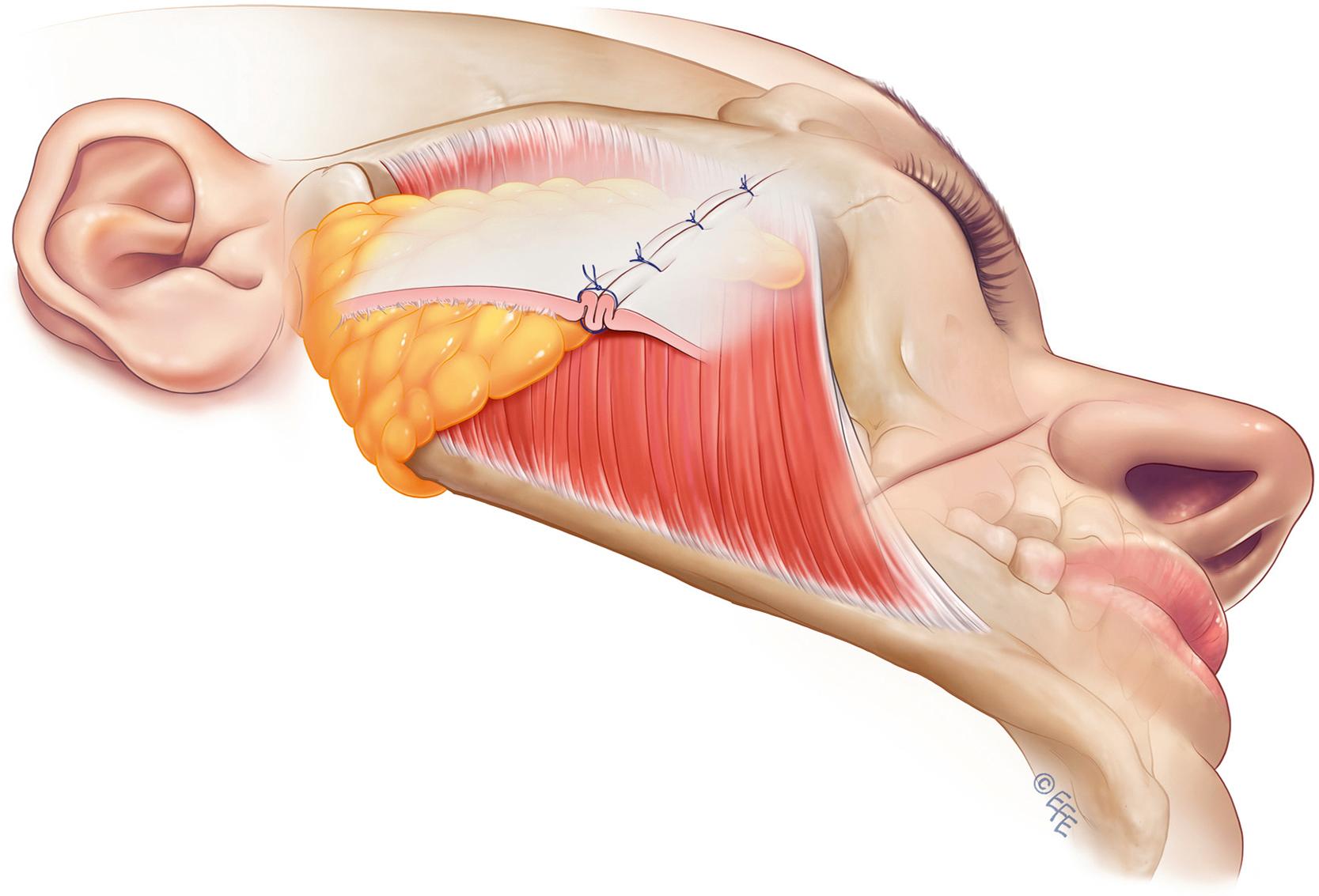
On completion of the SMAS dissection, the subsequent handling of the SMAS is varied according to the individual facial morphology, specifically the SMAS thickness. The options include plication (simple infolding of the lax SMAS) and imbrication (undermining of the SMAS and subsequent overlapping). Tightening is performed perpendicular to the nasolabial fold using buried sutures to reduce laxity and fullness. Thereafter, the redundant pre- and post- auricular skin is managed as in a standard skin facelift.
Variations of this technique continue to have wide popularity. The advantages include relative safety in relation to the sub-SMAS facial nerve branches, while providing a degree of effective manipulation of the mobile SMAS, combined with a reasonably fast postoperative recovery, yielding a more lasting improvement than skin-only rhytidectomies. Superolateral traction on the SMAS without release of its more anterior retaining ligaments (masseteric cutaneous) is a limitation as this restricts the tightening of the more anterior laxity towards the nasolabial fold and oral commissure, which explains why correction of the anterior midface had traditionally been limited.
The role of the SMAS was the major topic of discussion in facelifts through the late 1980s and 1990s. In this context the newly introduced deep plane and then composite facelift techniques, introduced by Hamra, became hot topics. , These were an evolution of the original Skoog operation. Skoog did not describe his operation as being sub-SMAS as it preceded the introduction of the term. Skoog described the plane of dissection used in his revolutionary facelift, in correct anatomical terms, as being under the superficial fascia. For surgeons of the time, for whom considerations of anatomy were not usual in the context of facelifts, this concept was not readily accepted until the surgical term the “deep plane” was later introduced. Hamra’s deep plane concept, being clearly descriptive of the dissection plane, was less anatomically confusing and the term became widely adopted and remains in use to this day, although Hamra’s surgical plane of dissection transitioned from being sub-SMAS to become more superficial, as the dissection continued medially over zygomaticus major.
Some clarification regarding use of the term “composite” is required, as two different, yet similar, meanings are attributed to it. In the context of flaps, a composite flap is one in which the several concentric tissue layers in a compound flap remain in their natural fused anatomical relationship. A scalp flap is the archetypal composite flap, consisting of the outer three tissue layers, skin (layer 1), subcutaneous layer (layer 2), and galea aponeurotica (layer 3), that form a vertical composite. Elevation of a scalp flap involves dissection through the subgaleal areolar tissue glide plane (layer 4) beneath the composite flap, allowing it to be separated from the underlying fixed deep fascia, the periosteum. (layer 5).
In Hamra’s composite facelift, described in 1990, the term composite was used to denote the surgical extension medially of the same SMAS layer to incorporate the orbicularis oculi within the flap. According to Hamra’s description, it is the inclusion of the lower lid orbicularis in the flap (elevation and repositioning) and its (horizontal) continuity with the sub-SMAS cheek flap that determines Hamra’s composite. Otherwise, a deep plane facelift does not impact the lower eyelid in spite of obtaining vertical cheek movement. Hamra’s composite concept evolved to include a package of procedures: elevation of the lower lid deep to the orbicularis in layer 4, i.e., an extended submuscular flap, using a “zygorbicular” dissection and redraping the lid cheek in a superomedial vector after performing a septal reset procedure. This results in a powerful correction of the lid and upper cheek, as well as direct benefit to the midcheek and nasolabial fold.
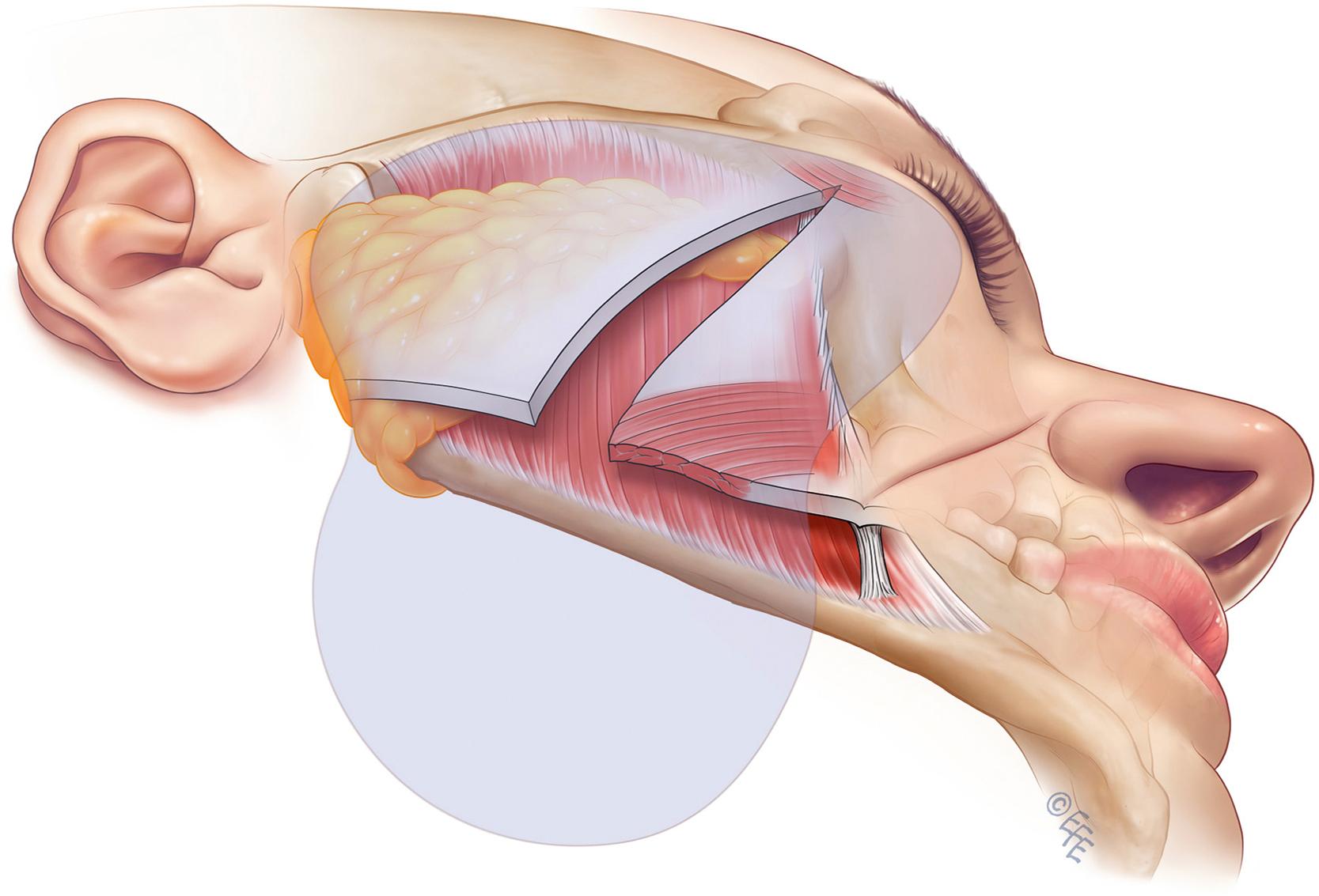
A standard facelift incision is used, with 2–3 cm subcutaneous skin flap dissection. The fixed SMAS is incised over the parotid and the sub-SMAS dissection continued superiorly to the malar eminence, dividing the zygomaticocutaneous and relevant masseteric ligaments. Dissection is continued medially over the surface of zygomaticus major muscle towards the nasolabial fold, while the remaining zygomaticocutaneous ligaments are divided to provide access to the malar fat pad. The musculocutaneous flap, once developed, is advanced and rotated superiorly. For the neck, the anterior neck is opened and the medial upper platysma edges approximated following excision of redundant medial platysma in the lower neck. This communicates with a superficial, preplatysmal dissection plane from the lateral approach with dissection carried 8–10 cm below the mandibular angle, with defatting of the flap where indicated. This leaves separate dissection pockets in the face and the neck, which do not communicate anatomically. Closure is performed with tension on the SMAS applied in the temporal fixation.
Hamra addressed a limitation of previous facelifts, being the failure to correct the upper cheek. He appreciated the importance of correcting aging changes of the lid–cheek junction (the lowering of the position of the upper cheek with lengthening of the lower lid) for complete facial rejuvenation. He further observed the benefit of correcting orbicularis oculi laxity in the roof of the prezygomatic space, which contributes to the appearance of malar mounds (crescent, bags) and modified his facelift to address this. To correct laxity of the orbicularis oculi of the upper cheek required an inferior extension of the submuscular lower lid blepharoplasty dissection, with communication through into the pocket of the, previously dissected, deep plane facelift. It was necessary to release the restraining effect of the ligamentous attachments along the orbital rim (later recognized to be the orbicularis retaining ligament) for this to occur. In contrast to the superolateral vector usually used in redraping a lower lid blepharoplasty flap, a superomedial vector is used to oppose the inferolateral vectors of upper cheek aging. The tightening is achieved at the completion of the facelift by suspension of the orbicularis flap to the lateral orbital rim. ,
Hamra’s composite facelift clinical series demonstrated impressive results as a result of the anatomically composite musculocutanenous flap that provides robust vascularity with reduced tension on the skin closure. In addition, the surgically composite access to the malar fat pad and superomedial cheeklift vector corrects the lid cheek area more effectively than do the extended and high SMAS counterparts. Similar to these techniques, potential damage to facial nerve branches in the dissection field and higher operative technical requirements with longer postoperative recovery are disadvantages that have limited usage of this specific technique ( Fig. 66.3 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here