Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
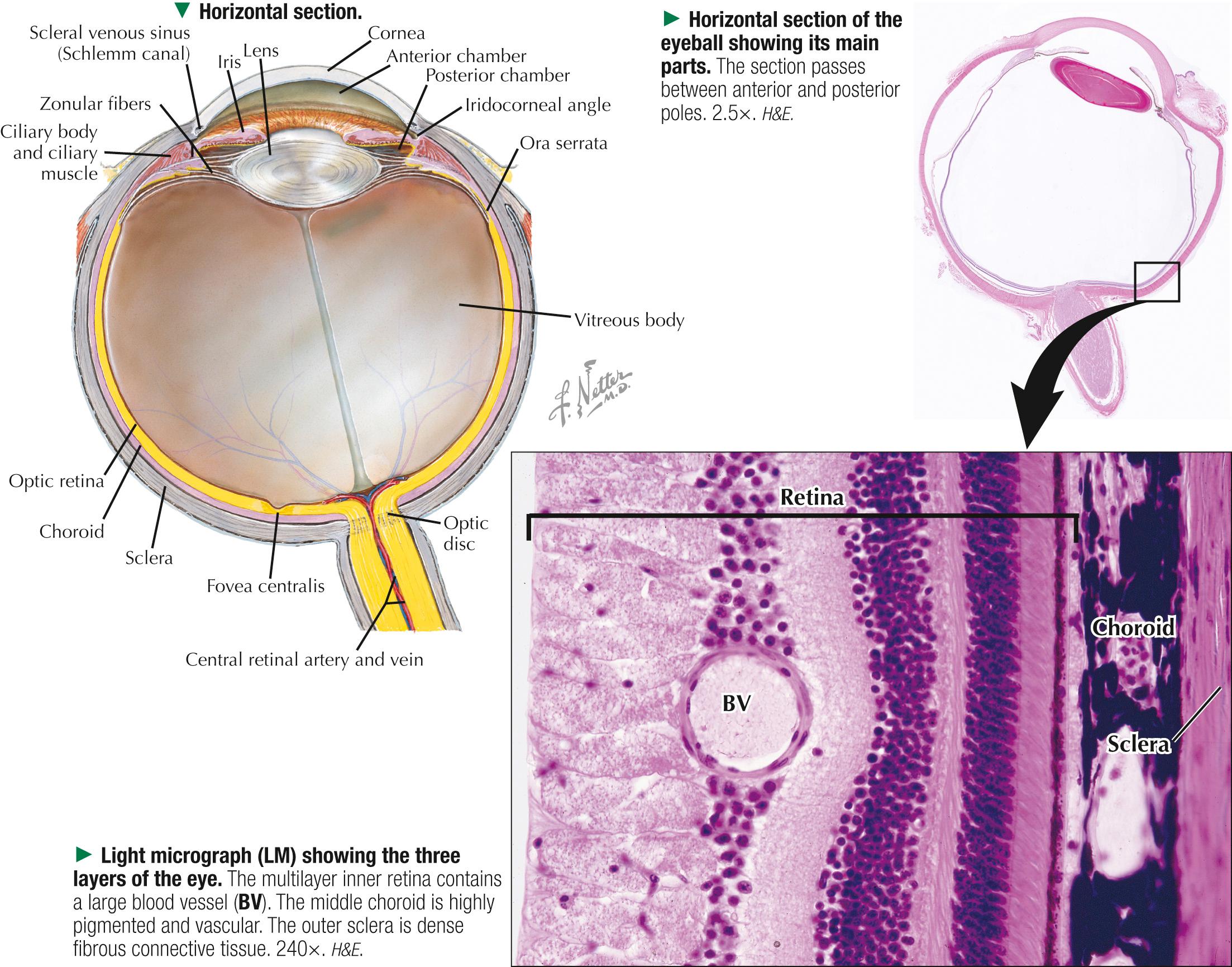
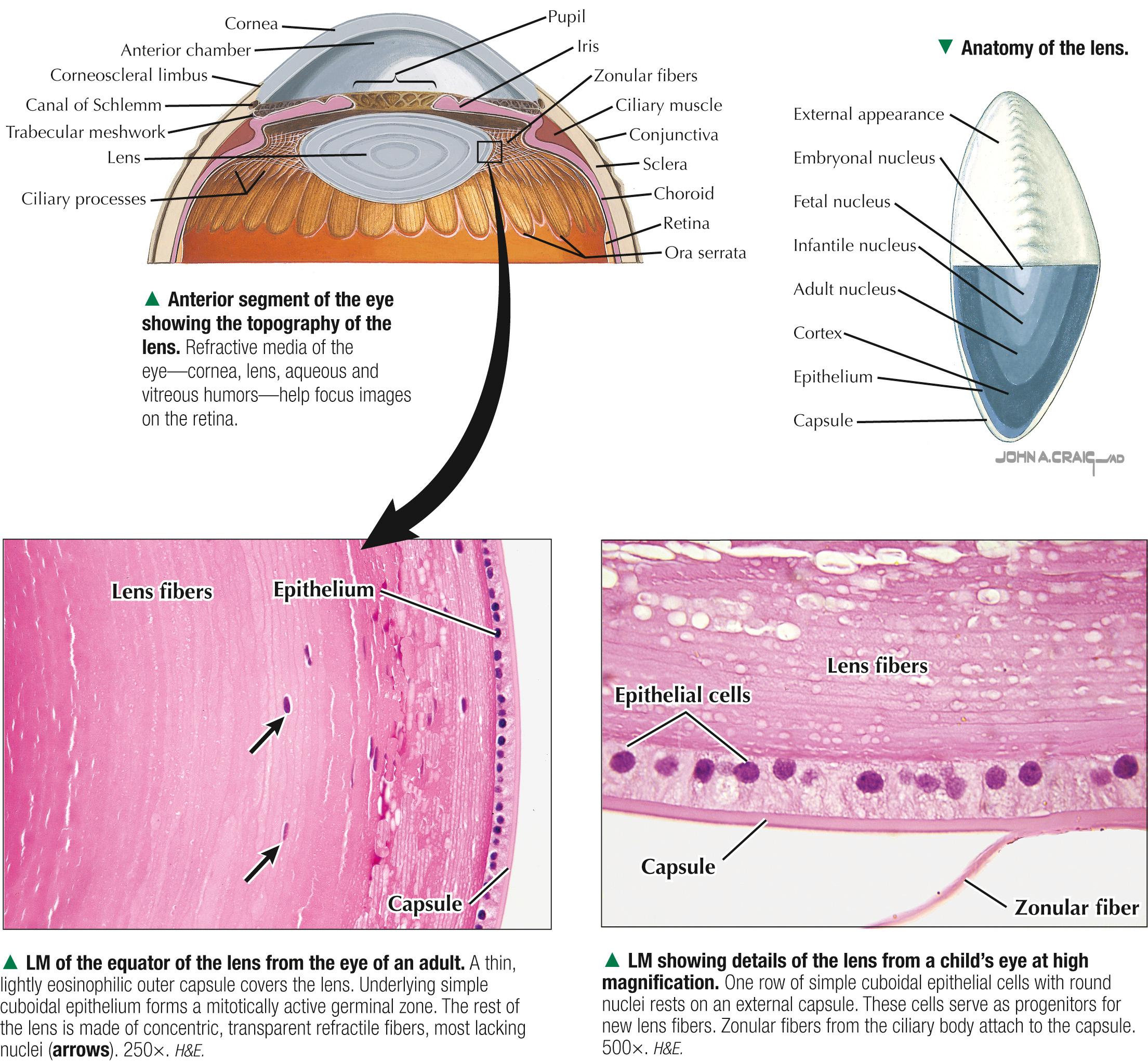
Eyes are complex, paired photoreceptor organs. Each is roughly spherical, about 2.5 cm in diameter. Eyes communicate with the brain via the optic (II) cranial nerve. They develop as an outgrowth of the brain, mostly from neuroectoderm, and from surface ectoderm and mesoderm, which give rise to adnexa. The wall has three concentric coats. The mainly protective outer fibrous layer consists of an opaque sclera posteriorly and a transparent cornea anteriorly. The middle vascular coat, or uvea, comprises choroid, ciliary body, and iris. The inner layer, the retina, consists of a small nonneural region, anteriorly. At the ora serrata, it becomes the neural retina, posteriorly. The multilayer neural retina contains specialized photoreceptors and other retinal cells. Optic nerve fibers from the retina exit posteriorly at the optic disc ( blind spot ). Three interior ocular chambers are the small anterior and posterior chambers, containing transparent fluid— aqueous humor —and the main chamber, the vitreous body. It is behind the lens and ciliary body and holds a transparent, semisolid gel rich in hyaluronic acid, which cushions the retina against shock and vibration. Descriptive terms for the eye can be confusing. Outer (or external) means the eye's exterior; inner (or internal) applies to more central areas in the bulb. The anatomic (optical) axis refers to a line between anterior and posterior poles, through the center of the cornea. The visual axis joins the center of the pupil through the posterior part of the lens and the fovea centralis, the site of sharpest visual acuity in the retina. The eyeball sits in the bony orbital socket, which contains adipose tissue, nerves, blood vessels, and three sets of skeletal (extraocular) muscles.
Myopia ( nearsightedness )—the most common refractive (eye focusing) condition in which close objects are seen clearly, but objects farther away appear blurred—occurs if the eyeball is too long or the cornea has too much curvature. As a result, light entering the eye is not focused correctly, and distant objects appear blurred. It affects 30% of people in North America and is classified as either simple juvenile onset, adult onset, or degenerative . For an accurate diagnosis, a standard ophthalmologic examination may include tonometry , slit lamp examination of the anterior segment of the eye, and retinography . Patients with myopia are at risk of developing a detached retina . Treatment options include corrective lenses (e.g., eyeglasses, contact lenses), orthokeratology , or laser and other refractive surgical procedures that reshape the cornea.
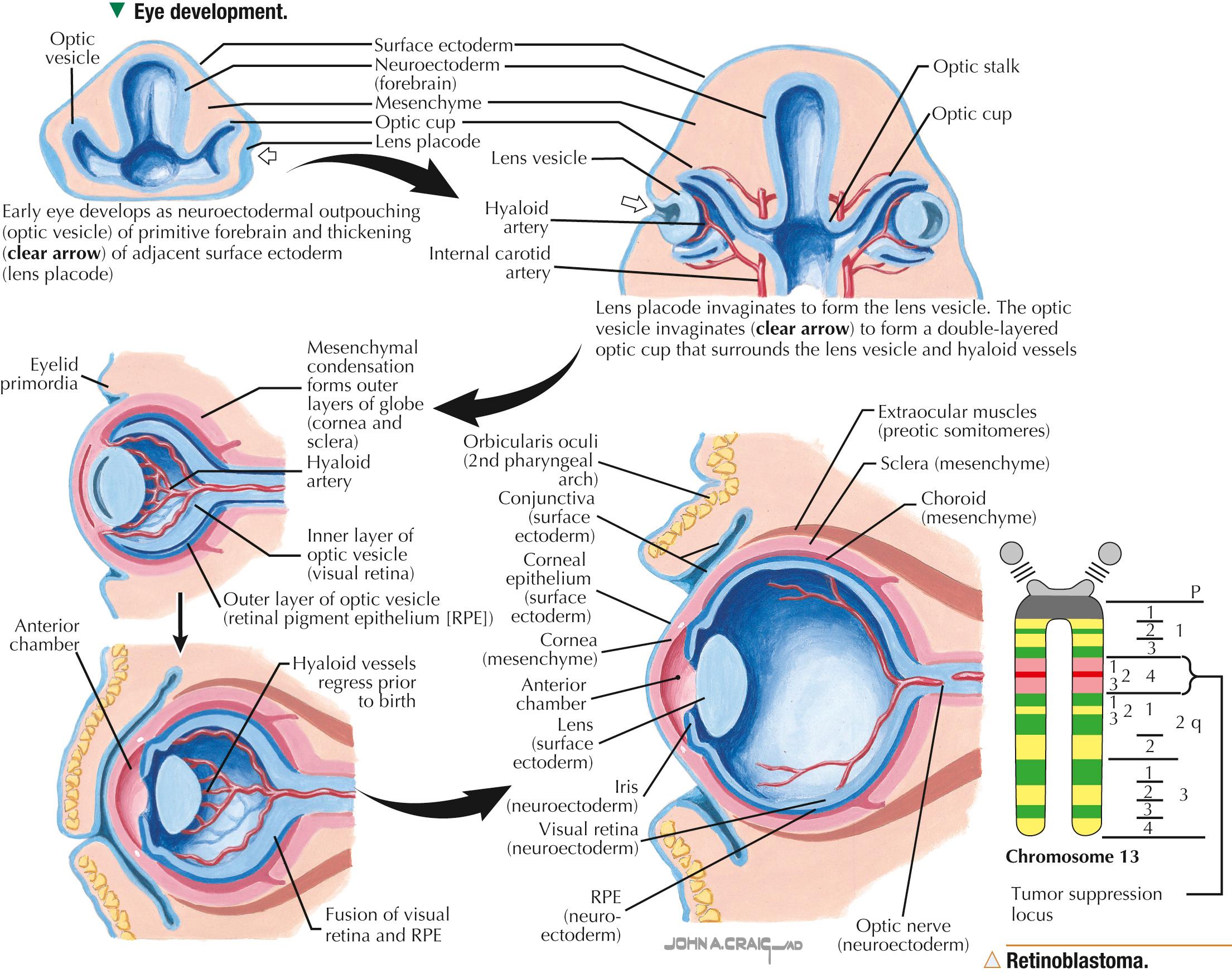
In the 4-week embryo, bilateral projections of neuroectoderm from the developing forebrain (diencephalon) become the optic vesicles. An optic stalk attaches each vesicle to the wall of the primitive brain. Optic vesicles induce overlying surface ectoderm to thicken and become the lens placode. A condensation of mesenchyme is interposed between the optic vesicle and lens placode. The hollow optic vesicle then invaginates onto itself, as if the side of a balloon is compressed, and becomes cup shaped with two layers. The inner layer of this optic cup, destined to be the neural retina, undergoes proliferation and stratification. The outer layer remains as simple epithelium and gives rise to retinal pigment epithelium (RPE). The potential space, or cleft, between the two layers may be the site of retinal detachment. Mesenchyme inside the optic cup invagination gives rise to the vitreous body. The inferior surface of the optic vesicle has a fissure that encloses hyaloid vessels and nerve fibers that will form the optic nerve. Proximal parts of hyaloid vessels become the retina's central vessels; distal parts supply the lens before they regress. A condensation of head mesenchyme around the optic cup gives rise to the middle vascular layer ( uvea ) and outer supportive layer ( sclera ) . The sclera (dense connective tissue) is continuous with dura mater around the developing brain. The lens placode bulges inward to become the lens vesicle, which then separates from corneal epithelium to become the biconvex lens. The inner substance of the cornea also arises from mesenchyme, but the anterior surface is epithelium derived from ectoderm. The anterior chamber develops as a space in the mesenchyme. Ciliary body and iris also develop from mesenchyme. Extraocular muscles arise from mesoderm of preoptic somites.
Retinoblastoma, the most common intraocular malignancy in infants and children, is so named because most cells in the tumor resemble undifferentiated embryonic retinal cells called retinoblasts. It is caused by a mutation in the long arm of chromosome 13 (13q14), which leads to an abnormal or absent tumor suppressor gene. The normal function of this retinoblastoma gene (RB1), the first human cancer suppressor gene to be completely characterized, is to suppress cell growth. Surgical removal of the tumor and enucleation (removal of the eye) are common treatments, but new chemotherapy agents that can cross the blood-ocular barrier, combined with laser and cryotherapy, provide favorable results.
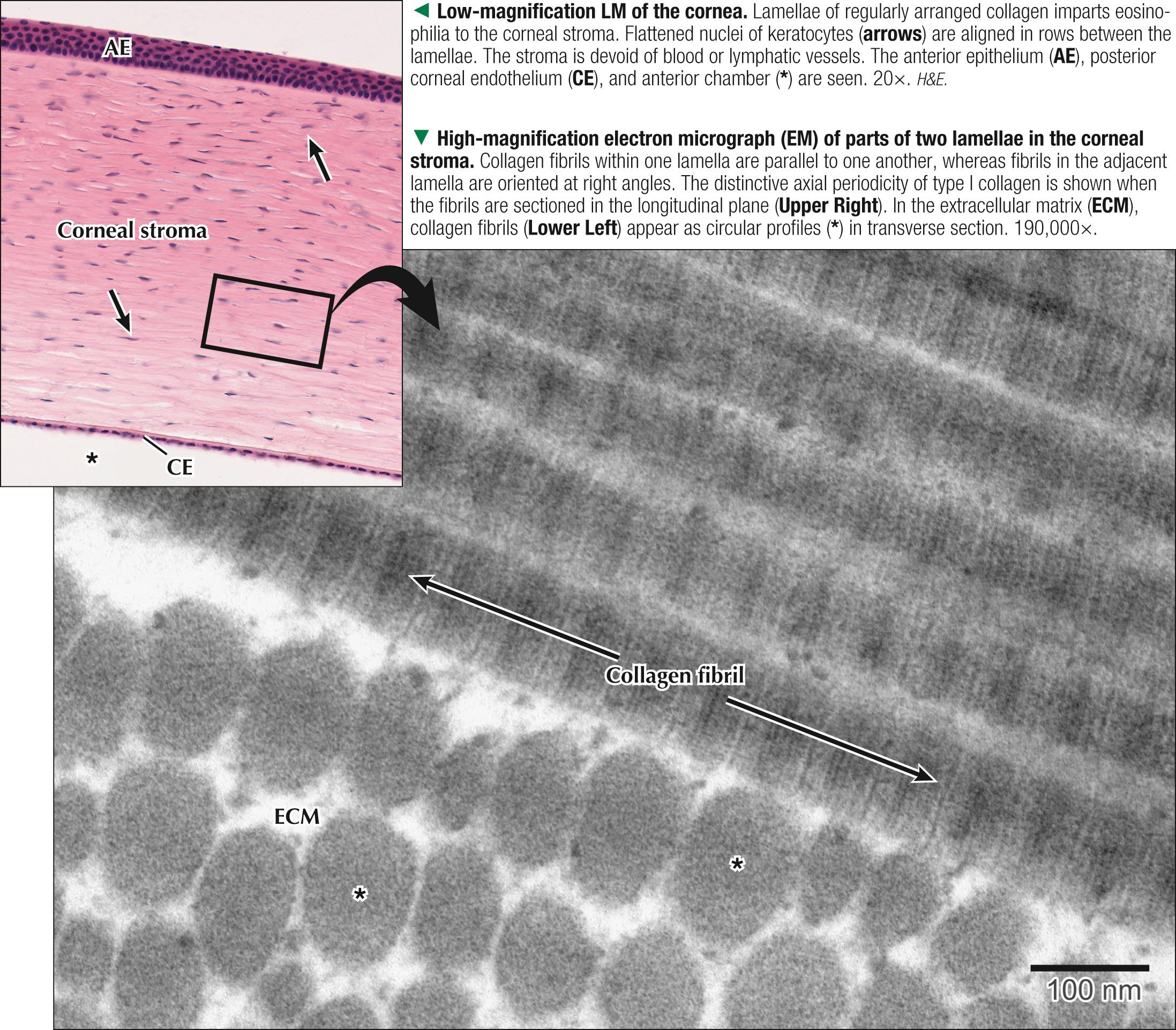
The cornea—dense connective tissue with a layer of epithelium on both sides—is about 0.5 mm thick, 11.5 mm in diameter, transparent, and resistant to deformation. It occupies one fifth of the ocular surface, with its radius of curvature less than that of the rest of the eyeball. Its anterior surface is nonkeratinized stratified squamous epithelium, about 50 µm thick and consisting of 3-6 layers of cells, except near the periphery, where it is 8-10 layers. Basal cells are polygonal, but the most superficial cells, which retain nuclei, are flattened. The epithelium continuously replicates, and it regenerates in response to wear and tear. Its rich sensory nerve supply (from the ophthalmic branch of cranial nerve V) is sensitive to touch and pain. A layer of tears lubricates the anterior surface. Deep to the epithelium is Bowman membrane —a prominent basement membrane, 8-15 µm thick—that binds epithelium to underlying connective tissue. The thick central region, the corneal stroma (or substantia propria ), contains 200-250 layers of type I collagen fibers, which are uniform in diameter and embedded in a proteoglycan-rich extracellular matrix. A unique pattern of collagen fibers—regularly arranged, parallel in each layer and at right angles in successive layers—contributes to transparency of the cornea. Simple cuboidal epithelium —misnamed corneal endothelium —lines the posterior surface. Its basement membrane (10-12 µm thick) is Descemet membrane. Its free (apical) surface is directly exposed to aqueous humor in the anterior chamber. Being avascular, the cornea is immunologically privileged and a good candidate for transplants. Most of it relies on diffusion of oxygen and nutrients from aqueous humor. The boundary between cornea and sclera (white of the eye) is an abrupt transitional zone, the limbus, where mucous membranes covering the sclera ( bulbar conjunctiva ) and underside of the eyelid ( palpebral conjunctiva ) join the anterior corneal epithelium. The sclera, about 0.5 mm thick and four fifths of the surface area, consists of dense fibrous connective tissue.
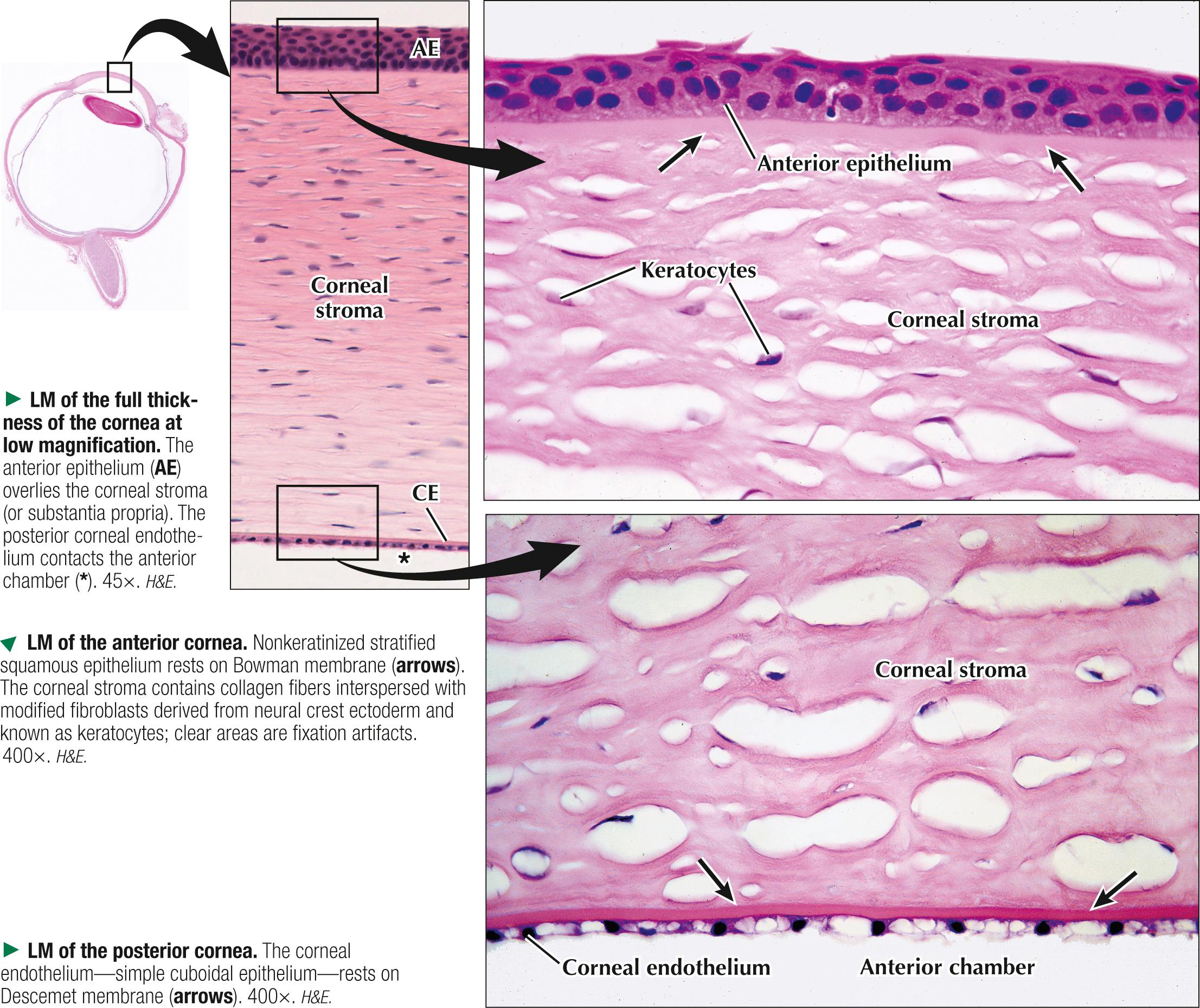
The stroma, which accounts for 85%-90% of the bulk of the cornea, is composed of 200-250 distinct lamellae of parallel, tightly packed, and evenly distributed type I collagen fibrils that are in a heterodimeric complex with type V collagen, which regulates their uniform and narrow diameter. Fibrils in each lamella are arranged at roughly right angles relative to fibrils in adjacent lamellae. The refractive index of the fibrils, which are about 28 nm on average in diameter, is similar to that of the intervening extracellular matrix (ECM)—a property that is essential to corneal transparency. Modified fibroblasts derived from the neural crest, called keratocytes, are stellate-shaped cells with numerous dendritic processes that form a syncytium via gap junctions. They synthesize collagen molecules, sulfated glycosaminoglycans, and proteoglycan core proteins (mainly lumican, keratocan, and decorin ) in the ECM. Their cytoplasm also houses corneal crystallins that help reduce backscatter of light, also contributing to corneal transparency.
Laser-assisted in situ keratomileusis ( LASIK ) is an outpatient surgical procedure used to treat certain refractive disorders (e.g., myopia [nearsightedness], hyperopia [farsightedness], astigmatism ) by reshaping the corneal curvature, thereby improving visual acuity. A precision surgical instrument, known as a microkeratome, first creates a thin (80-200 µm) circular flap of corneal tissue consisting of outer epithelial and stromal layers. A computer-controlled excimer laser then reshapes the cornea by vaporizing small amounts of stroma in a finely controlled manner. For patients, LASIK provides more rapid visual recovery and less pain than the original photorefractive keratectomy (PRK) procedure.
The iris—a circular diaphragm, 10-12 mm in diameter—is the most anterior part of the uvea and separates anterior and posterior chambers. Its free end is suspended in aqueous humor between the cornea and lens; its root is continuous with the ciliary body. Its central adjustable aperture is the pupil, whose opening and thus the amount of light reaching the retina, it regulates. Its anterior surface, which contacts the anterior chamber, has, instead of epithelium, a discontinuous layer of stromal cells: a mixture of fibroblasts and pigment-containing melanocytes. Spaces between the cells allow fluid from aqueous humor to percolate into the stroma. The stroma is richly vascularized, and most vessels have a corkscrew shape to adjust for length changes in the iris. The number of melanocytes in the stroma and the amount of melanin in their cytoplasm mostly determine eye color. A double layer of pigmented cuboidal epithelium, continuous with that of the ciliary body, covers the posterior surface. The superficial layer of these cells is in contact with aqueous humor in the posterior chamber. The inner layer is made of myoepithelial cells, which form the dilator pupillae muscle. Basal processes of these cells have abundant contractile filaments. Postganglionic nerve fibers of the sympathetic nervous system stimulate the cells to contract, which causes pupil dilation. In the stroma, near the pupillary margin, lies the involuntary constrictor pupillae muscle, a flat ring of circumferential smooth muscle, about 0.75 mm in diameter, that reduces pupillary diameter by contraction. Postganglionic nerve fibers of the parasympathetic nervous system innervate it. Both dilator and constrictor muscles derive from neuroectoderm.

The lens is an elastic, biconvex avascular structure between the iris and vitreous body. It is about 10 mm in diameter and 3.5-5 mm wide. It is held in a fairly fixed position by zonular fibers (from the ciliary body) and the vitreous body behind it. Tensile forces in the lens cause its roughly globular shape. Its elasticity diminishes with age, which restricts its limit of focus. Lens fibers, the main cells of the lens, are elongated columnar epithelial cells with distinctive cytoplasmic proteins ( crystallins ) , filensin intermediate filaments, and a degenerated nucleus. Enveloping the lens is a homogeneous capsule that corresponds to a thick basement membrane containing a network of collagen fibrils. Underneath it, the anterior half of the lens has a simple cuboidal (lens) epithelium, the germinal zone. The lens epithelial cells in the equator undergo mitosis and differentiation throughout life. They elongate, accumulate protein, and lose nuclei. The posterior half of the lens lacks an epithelium. Like the cornea, the lens depends on diffusion of aqueous humor for nutrition.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here