Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Central venous access is required for temporary or permanent hemodialysis in many situations. It is estimated that several million central venous catheters (CVCs) are inserted annually in the United States. This widespread use has been accompanied by a concomitant abundance of catheter-related complications. With meticulous attention to proper techniques of insertion and maintenance, successful central venous access can be achieved while minimizing the incidence of complications.
Total parenteral nutrition (TPN) infusion is considered adjunctive therapy in patients suffering from short bowel syndrome, enterocutaneous fistulas, hepatic failure, acute kidney failure, and major thermal injury. In patients with contraindications to enteral nutrition, TPN is used solely as a means of providing nutritional support. Peripherally inserted central venous catheters (PICC lines) may also be used for TPN infusion and can prevent the severity of access site complications associated with puncture of larger, more central veins for access (e.g., internal jugular, subclavian, femoral). Catheter-related blood stream infections are not minimized compared with CVCs placed in more central veins.
In situations requiring intravenous (IV) chemotherapy, CVCs are considered when patients must receive multiple doses or have poor peripheral venous access. Like TPN, many chemotherapeutic agents can cause phlebitis when introduced into peripheral veins. Subcutaneously implanted ports have become a common form of central access for chemotherapy. These ports allow infusions of medication while minimizing the need for daily catheter care. Catheter-related thromboembolic complications have been reported at a rate of 12% to 64% of these patients.
To achieve long-term hemodialysis access, the recommended approach involves surgical construction of a primary arteriovenous fistula (AVF) or arteriovenous graft. However, in certain clinical situations, CVCs are required for temporary or permanent hemodialysis. Central venous catheterization is the preferred method for patients in whom kidney function is expected to return within a short time and is also used for emergent hemodialysis. In some patients, external angioaccess may be necessary if kidney failure sets in during the window period required for the AVF or prosthetic angioaccess graft to mature. Efforts should be made to remove the CVC once more permanent AV access is established. Long-term use of CVCs can result in central venous stenosis and thrombosis, which can compromise future peripheral AV access sites.
When patients are not candidates for AVFs or prosthetic angioaccess grafts, hemodialysis requires chronic central venous access. Children weighing less than 25 to 30 kg typically do not have upper extremity vessels suitable for AVF, with or without prosthetic graft material. In the setting of extensive arterial occlusive disease, AVFs or prosthetic angioaccess grafts can cause arterial steal syndromes by diverting blood from distal arteries to the venous limb of the fistula. Patients who have already had multiple failed AVFs or prosthetic angioaccess grafts might require external methods of hemodialysis. In these patients, the construction of multiple fistulas has often obliterated all anatomic locations for additional AVFs or grafts. Finally, patients with limited cardiac reserve may be unable to tolerate AVFs or synthetic angioaccess grafts because of the risk of high-output congestive heart failure.
In the acute setting, central venous access is achieved using percutaneous nontunneled catheters that are usually 7 to 8 Fr. These catheters are typically composed of stiff polyurethane. They are used for both IV infusion and hemodynamic monitoring of critically ill patients. The internal jugular vein is the most common site for insertion, but the femoral and subclavian veins may also be used. Acute-care devices are generally less comfortable for the patient and lack the durability needed for long-term use.
The Quinton–Mahurkar catheter is a device used to gain immediate vascular access for short-term hemodialysis. Composed of flexible polyurethane, this catheter consists of a dual lumen with two D -shaped channels. Each lumen is connected by a molded Y -piece to an external port. In addition to hemodialysis, the catheter structure allows other forms of IV therapy, as well as blood sampling and plasmapheresis.
Transition access devices are also percutaneous nontunneled catheters, but they are designed to facilitate extended IV therapy. The PICC line is most commonly used. PICC lines are inserted through an antecubital vein and advanced centrally into the superior vena cava or right atrium. The use of PICC lines for extended IV therapy reduces cost by allowing the procedure to be performed outside of an operating room. However, these devices are secured using only sutures, and they can become dislodged more than tunneled devices. Most nontunneled catheters also lack the subcutaneous cuff present on tunneled devices.
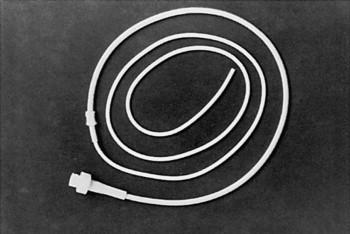
Tunneled catheters were developed to facilitate long-term administration of IV therapy. Two commonly used tunneled devices are the Broviac and Hickman catheters. The Broviac catheter ( Figure 1 ) was designed for prolonged infusion of TPN in children, and the Hickman catheter was developed to allow long-term central venous access in patients undergoing bone marrow transplantation. Both are now used for a variety of IV treatments, and they are also used in combination as a Hickman–Broviac double-lumen catheter. The catheters share many characteristics, including silicone elastic (Silastic) composition and a proximal cuff. The cuff anchors the catheter to surrounding soft tissues while also providing a mechanical barrier to infectious organisms. The main difference between these devices is catheter diameter. When using a Hickman–Broviac catheter, the smaller Broviac line is used for TPN or other forms of IV therapy. The larger Hickman line may serve as an additional line for IV therapy or as a source for blood withdrawal.
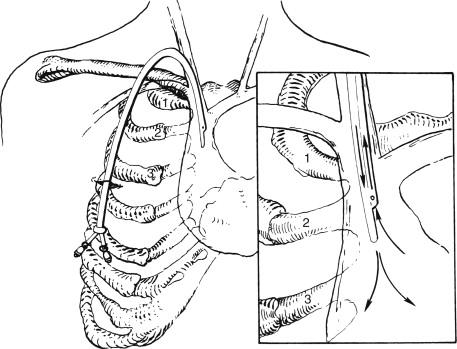
When using either CVC, access may be achieved using the subclavian, internal jugular, or femoral veins. Portable ultrasound and fluoroscopy should be used routinely when placing these lines. The distal end is advanced to a location just above the right atrium, and the proximal end exits the lower anterior chest wall ( Figure 2 ), anchored to the subcutaneous tissue by the cuff. Because of the silicone elastic composition, both catheters have low thrombogenicity but are susceptible to perforation or rupture. For this reason, guidewires should not be used to attempt clearance of obstructed catheters. Obstructed catheters should instead be irrigated using syringes no larger than 5 mL. Another recommended practice is to irrigate the lines with normal saline after any IV infusions to prevent occlusion or mixing of incompatible solutions. Hickman lines must be irrigated with heparinized saline after blood transfusions to prevent clot formation within the lumen.
The Groshong catheter is another silicone elastic tunneled device used for long-term IV therapy. The catheter has a relatively thin wall and small diameter, allowing bedside insertion using local anesthesia. This unique catheter is closed at its distal end but has a pressure-sensitive two-way valve near this tip. The valve prevents backflow after infusions but allows blood withdrawal with application of gradual negative pressure. This valve eliminates the need for heparin flushes, and catheter maintenance involves little more than weekly saline flushes. The manufacturer does recommend irrigation with normal saline after infusion of TPN or blood products.
Implanted ports are unique in that they reside completely beneath the skin and are accessed percutaneously. The device consists of a catheter attached to a titanium or plastic reservoir with a silicone access septum. Vascular access is accomplished by penetrating the self-sealing septum with noncoring needles that are specialized to minimize destruction of the septum. Implanted ports are ideal for patients receiving intermittent chemotherapy. The device requires minimal maintenance and can reduce the incidence of catheter-related infection.
The internal jugular vein is the preferred initial access site for central venous catheterization. The routine use of ultrasound guidance along with CVC placement has decreased complication rates and is recommended. Advantages of this approach include a more direct course to the right side of the heart and a lower risk of pneumothorax when compared with subclavian vein insertion. The right internal jugular is the site usually chosen because of its relatively straight course to the subclavian vein. The vessel lies deep to the sternocleidomastoid muscle in a position lateral and anterior to the common carotid artery. The main landmark used for placement is the division of the medial and lateral heads of the sternocleidomastoid muscle.
After the patient is placed in the Trendelenburg position, the head is rotated away from the side being catheterized, and the location of the vein is confirmed with ultrasound. After infiltrating this site with lidocaine, a 16-gauge needle is introduced and directed slightly inferiorly and toward the ipsilateral nipple. Care is taken to observe the needle puncture through the anterior vein wall with real-time ultrasound. Applying suction to the syringe, the appearance of venous blood indicates access of the internal jugular vein. A guidewire is then advanced through the needle 5 to 10 cm into the vein. If resistance is encountered while inserting the wire, the wire should be removed and blood should be reaspirated to reconfirm intravascular placement. A small skin incision is made, and a dilator is advanced over the wire to create a subcutaneous tract. The dilator is then removed, and the catheter is placed over the wire. The guidewire is withdrawn, and the catheter is sutured in place and covered with a sterile dressing. The use of tunneled devices and implanted ports requires an additional step of creating a subcutaneous tunnel from the venous insertion site to the catheter exit site or port reservoir.
The subclavian vein is an alternative location used for the placement of CVCs. Advantages of this approach include its easily identified landmarks and relative comfort for the patient undergoing long-term IV therapy.
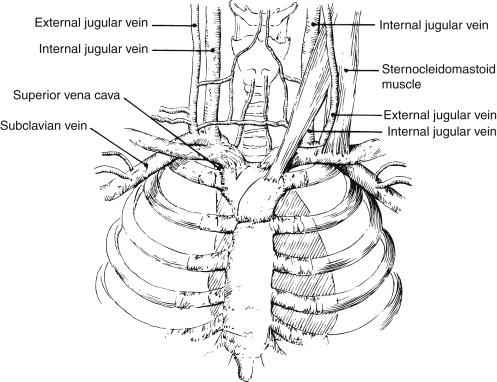
After placing the patient in the Trendelenburg position, the landmarks used for catheterization should be identified. An understanding of the anatomic relationships in this region is helpful ( Figure 3 ). The subclavian vein arches over the first rib and passes posterior to the clavicle and anterior to the insertion of the scalenus anterior muscle. The vein is most easily accessed as it passes over the first rib. Both the lateral head of the sternocleidomastoid muscle and the division of the medial and middle thirds of the clavicle can serve as landmarks for this optimal site of catheterization.
The skin and subcutaneous tissue at this site are anesthetized with lidocaine. A 16-gauge needle attached to a syringe is then advanced under the clavicle in a direction medial and cephalad toward a point 2 to 3 cm above the jugular notch. As the needle is directed behind the clavicle, care must be taken to advance the needle parallel to the ground because a more posterior direction can cause pneumothorax. If the initial attempt at cannulation is unsuccessful, a more cephalad approach may be attempted. When venous access is achieved, the needle is advanced 0.5 cm to ensure complete insertion of its beveled portion. At this time, catheterization can proceed using the same steps of the Seldinger technique employed in the internal jugular vein method.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here