Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Atherosclerotic peripheral artery disease (PAD) involving one or more major vessels of the lower limb is common. The global spread of abdominal adiposity, its associated metabolic disorders and smoking has led to a significant increase in PAD, particularly in lower- and middle-income countries (LMIC). Current estimates suggest that over 200 million people globally are affected by PAD, with a marked increase in those affected over the last decade (LMIC 29% increase, high income countries (HIC) 13% increase). PAD tends to affect older patients and likely occurs because of both genetic and environmental interactions that result in the development of atherosclerotic disease. The natural history of the lower limb in patients with symptomatic PAD (intermittent claudication) is somewhat benign, with up to 75% of patients noticing stabilisation or some improvement of their symptoms. Patients with PAD, however, are at significant risk of major adverse cardiovascular events (MACE), noticeably because of concomitant atherosclerotic disease within the coronary, carotid and cerebral circulation. Disability and mortality associated with PAD have increased over the last 20 years, and this increase in burden has been greater among women.
There are a number of studies that highlight this link between PAD and MACE, predominantly using the ankle–brachial pressure index (ABPI) as a marker of disease severity. Data from the Ankle Brachial Index Collaboration group showed that a low ABPI (<0.9) was associated with an increased risk of subsequent all-cause mortality (pooled relative risk [RR] 1.60; 95% confidence interval [CI], 1.32–1.95), cardiovascular (CV) mortality (pooled RR 1.96; 95% CI, 1.46–2.64), coronary heart disease (pooled RR 1.45; 95% CI, 1.08–1.93) and stroke (pooled RR 1.35; 95% CI, 1.10–1.65) after adjustment for age, sex, conventional CV risk factors and prevalent CV disease.
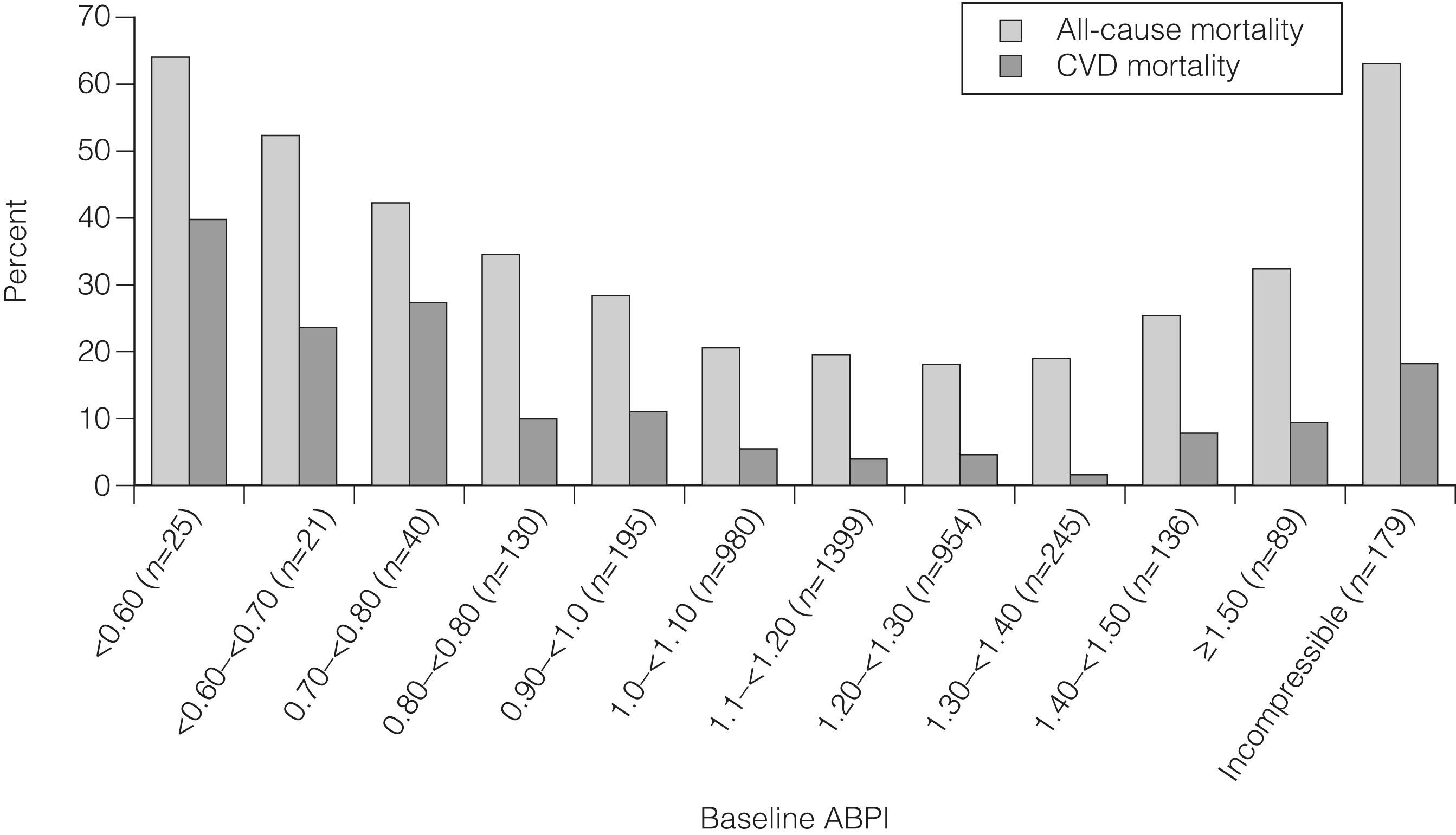
Medial artery calcification, associated with diabetes and renal disease leads to an inability to compress the arteries during ABPI measurement. An elevated ABPI (defined as >1.40) has also been identified with an increased risk of all-cause and CV disease mortality (adjusted risk estimates 1.77 all-cause mortality / 2.09 CV mortality). This U-shaped relationship between ABPI and outcome is now well recognised ( Fig. 1.1 ).
The aims of this chapter are to describe the epidemiology of lower limb PAD and analyse the role of reversible and irreversible risk factors on both disease progression and the incidence of MACE.
Compared to coronary artery disease (CAD), there are few data available on the epidemiology of PAD. The incidence of PAD is defined as the rate of new (or newly diagnosed) cases of the disease (generally reported as the number of new cases occurring within a period of time). Prevalence is defined as the actual number of cases alive with the disease either during a period of time (period prevalence) or at a particular date in time (point prevalence). The true incidence and prevalence of PAD is difficult to determine accurately, in part because of methodological issues related to the diagnosis of PAD but also because of continuing changes in CV risk factor prevalence and management. Differences are also encountered depending on sampling criteria and whether the diagnosis of PAD is based purely on symptomatic patients (intermittent claudication/chronic limb threatening ischaemia [CLTI]) or whether one includes asymptomatic individuals.
The population may be screened using a questionnaire-based approach (Rose questionnaire/Edinburgh Artery Questionnaire). These questionnaires tend to underestimate the diagnosis of claudication and a more objective analysis of limb perfusion (ABPI/reactive hyperaemia) may be more appropriate. The ABPI has become an increasingly used diagnostic tool for PAD, with a value ≤0.9 signifying PAD. It is both a reproducible and reliable test although there are circumstances where a false-negative reading may be obtained, which includes patients with medial artery calcification where arterial compression is difficult, the presence of mild arterial lesions (often seen in the iliac artery) and where significant collateralisation has occurred. In such circumstances, pre- and post-exercise ABPI measurement can help, but these are impractical to perform in population-based studies. A number of the initial validation studies of ABPI were performed before the advent of arterial duplex. As such, intra-arterial lower limb angiography was used as the gold standard against which the ABPI was compared. As this is an invasive test, carrying some risk, ABPI was only determined in selected patients with significant symptoms who were more likely to have severe arterial disease, and this was compared against younger ‘normal’ controls. As such, the observed sensitivity and specificity values obtained were between 97% and 100%. , In a more representative sample of patients seen in daily practice, the specificity of ABPI measurement is maintained at approximately 97%, the sensitivity falls to nearer 80%. There can be confusion in such epidemiological studies when determining whether solely symptomatic PAD or PAD as a whole (symptomatic and asymptomatic) are included. This gains some importance when discussing the merits of screening for PAD.
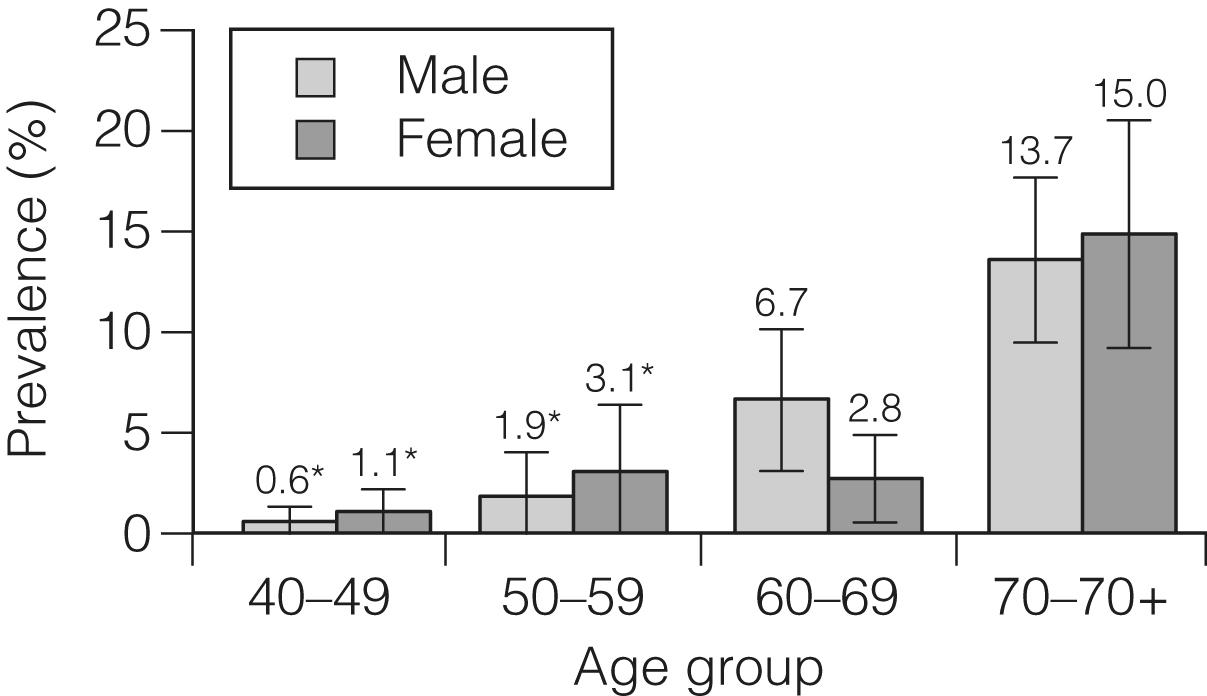
In population studies using ABPI for the diagnosis of PAD, studies suggest a prevalence of PAD of approximately 3–10% in the population as a whole, with this increasing to between 15 and 20% when focusing on older patients (>70 years of age). More recent studies include the PAD Awareness, Risk, and Treatment: New Resources for Survival (PARTNERS )study, the National Health and Nutritional Examination Survey (NHANES) and the REGICOR study ( Fig. 1.2 ). The PARTNERS study screened 6979 subjects for PAD using ABPI (included were people over 70 years OR age 50–69 years and at least one CV risk factor). PAD was detected in 29% of the population. The NHANES recruited an unselected cohort of subjects over 40 years of age and found a prevalence of PAD of 2.5% in those aged 50–59 years, rising to 14.5% in those aged >70 years. The REGICOR study, studying a purely Mediterranean population, found the prevalence of PAD to be 4.5% (5.2% in men and 3.9% in women). Other studies report prevalence of PAD from 3–20%, with variation depending upon methodology and the population examined. Interestingly, there appears to be little difference in prevalence between men and women, with ratios ranging from 0.8 to 1.2. The issue with regard to the method of assessment of PAD is borne out by the data from the British Regional Heart Study, where direct assessment of the femoral artery performed using ultrasound suggested that 64% of people aged 56–77 years have significant femoral atherosclerosis, of whom fewer than one-fifth were symptomatic.
Data on the incidence of PAD are more limited. The Limburg study, involving a cohort of 2327 patients selected from 18 primary care facilities in the Netherlands, found that after a follow-up period of 7.2 years the overall incidence rate for asymptomatic PAD was 9.9 (95% CI, 7.3–18.8) per 1000 person-years at risk. The rate was 7.8 (95% CI, 4.9–20.3) for men and 12.4 (95% CI, 7.7–24.8) for women and more marked in those patients over the age of 65 years. The REGICOR study collected data on 5434 individuals aged between 35 and 79 years. In total, 118 new cases of confirmed PAD were identified, resulting in a cumulative population incidence rate of 377 cases per 100 000 person years, lower than that seen in other areas.
Intermittent claudication is a symptom of muscular lower limb pain brought on by exertion and relieved by rest, with CLTI being at the more severe end of the symptom spectrum (night pain/rest pain/tissue loss). The prevalence of intermittent claudication varies, up to 3% at the age of 40 years and rising to 6% at 60 years. While some of the data are historic, the largest studies performed over 3 decades ago are probably still the most reliable. These include the Edinburgh Artery Study, which screened large random samples of the general population using age/sex registers from general practices. This study used both the World Health Organisation (WHO) questionnaire and the ABPI to determine the prevalence of both symptomatic and asymptomatic lower limb PAD in a sample of 1592 participants (men and women) aged between 55 and 74 years. They found that the prevalence of intermittent claudication was 4.5% (95% CI, 3.5–5.5) with major asymptomatic disease seen in 8.0% (95% CI, 6.6–9.4).
The incidence of claudication also varies, in part depending on geography, with values as low as 0.2% in Iceland, 1.0% in Israel and 1.6% from the Edinburgh Artery Study. , , More detailed data come from the Framingham dataset that showed an overall incidence of 7.1 per 1000 years in men and 3.6 per 1000 years in women, although the gender differences were not seen between the ages of 65 and 75 years. Data from the REGICOR dataset suggest an incidence for symptomatic PAD of 102 per 100 000 person years. This suggests that the incidence of PAD is lower in the Mediterranean area than reported from other areas and warrants more in-depth analysis.
The incidence of CLTI has been estimated to be around 400 cases per million population per year, which equates to a prevalence of 1 in 2500 of the population annually. For every 100 patients with intermittent claudication, approximately one new patient per year will develop critical ischaemia.
What is clear is that the incidence of symptomatic PAD (intermittent claudication and CLTI) increases steeply with age. , When considering the effect of ethnicity, the most comprehensive data come from a study by Allison et al., who combined data from seven community-based studies within the USA. The study showed that PAD was uncommon before the age of 50 years but was present in up to 20% of subjects over the age of 80 years. The rate of PAD in Black Americans was double that seen in non-Hispanic Whites (NHW), with the rates for Hispanics, Asian Americans and Native Americans similar to those in NHW.
There are a number of important methodological issues in determining the natural history of lower limb PAD. This relates to a higher chance that significant disease progression may result in either revascularisation or limb loss, or if associated with more aggressive atherosclerotic progression in other arterial beds, then a higher mortality risk. When considering symptom progression, then this is in part related to the degree of collateralisation, muscle adaptation, allied physical function/ability and adaptability so that there may be marked differences seen between pathological disease progress and symptom progression. There is, however, a reasonable quantity of data on PAD progression using predominantly ABPI measurements as a marker of PAD.
The Cardiovascular Health Study, analysing a cohort of 5000 patients with normal ABPI, reported a 9.5% incidence of PAD over a 6-year follow-up period. The Edinburgh Artery Study found between 7% and 15% of patients with initially asymptomatic PAD developed intermittent claudication over a 5-year follow-up period. Nicoloff et al. reported a 37% deterioration in ABPI over a 5-year follow-up, which equated to clinical progression (defined as symptom change or need for revascularisation) in 22%. , A smaller study from Germany suggested lower limb PAD progression occurred in 18.6% over a 5-year follow-up period and 30% in a study from San Diego in a similar time period, using a six-category scale of disease severity. ,
Large population studies from Edinburgh and Basle in people with claudication suggest that only a quarter of patients will have significant deterioration in symptoms, with this being most frequent within the first year after diagnosis (7–9%) and after this occurring in only 2–3%. Specifically, the risk of amputation is rare, occurring in only 1–3% of patients with intermittent claudication at 5 years.
Atherosclerotic disease can be manifest in a number of arterial beds and as such PAD is associated with other vascular-related conditions, specifically within the coronary and cerebral circulations.
In a screening programme consisting of ultrasound screening of 3.6 million people in USA, the proportion of subjects with two or more affected arterial beds increased with age from 0.04% (40–50 yeas of age) to 3.6% (81–90 years of age). In patients with a diagnosis of PAD (defined as an ABPI <0.9) between 25–70% of patients will have CAD, 14–19% of patients will have a carotid stenosis >70% and between 10–23% of patients will have a renal artery stenosis of >75%.
These findings are supported by the Atherosclerosis Risk in Communities study, a study of 15000 middle-aged subjects. A diagnosis of PAD (ABPI <0.9) was associated with a twofold increase in CAD. The association is starker in older patients. A study of 1800 older patients (mean age 80 years) from New York showed that a diagnosis of PAD was associated with coronary disease in 68% of patients and with a history of ischaemic stroke in 42%.
Further corroboration comes from the Reduction of Atherothrombosis for Continued Health (REACH) registry, a large multinational registry collating observational data about the spectrum of disease progression, CV outcomes and patterns of treatment in patients with atherosclerotic disease. The registry encompasses a total of 67 888 patients, aged 45 years or more, from 44 countries with an inclusion criterion of either established CV disease or, if they were asymptomatic, with more than three risk CV risk factors (n = 12 389). Among the symptomatic group, patients were enrolled on the basis of CAD (n = 40 248), cerebrovascular disease (CVD; n = 18 843) or PAD (n = 8273), with 16% of this group having polyvascular disease.
Between 7–16% of patient with a diagnosis of CAD will also have concomitant lower limb PAD. The PAD is commonly asymptomatic because of exercise limitations seen in patients with CAD, namely anginal and dyspnoea symptoms. Of note, patients with PAD in the coronary population exhibit more extensive, heavily calcified and progressive coronary atherosclerosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here