Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Anticoagulation has long been considered the gold standard for treatment of lower extremity deep vein thrombosis (DVT). This therapy is effective at preventing DVT extension, pulmonary embolism, and DVT-related death. However, because anticoagulation does not dissolve thrombus, clot resolution is slow, relying on the intrinsic thrombolytic pathways. Although this is sufficient for isolated calf DVT, prolonged venous obstruction can lead to pronounced long-term morbidity in those with more proximal iliofemoral DVT. Five-year follow-up of patients with iliofemoral DVT treated with anticoagulation alone demonstrates that up to 95% develop venous hypertension, 90% display venous reflux, 15% exhibit venous claudication, and another 15% develop venous ulceration. Poor quality of life has been substantiated by further study.
Early clot removal with surgical venous thrombectomy for iliofemoral DVT was first reported by Fogarty and colleagues in 1966. Venous thrombectomy was demonstrated to improve long-term patency and substantially reduced the occurrence of postthrombotic symptoms and morbidity. Nonetheless, this technique was highly invasive, which prevented widespread acceptance and implementation.
Systemic thrombolysis was assessed as an alternative to venous thrombectomy, with improvement in patient outcomes and venous patency correlating directly with the degree of lysis. Complete lysis, however, was only achievable in up to 50% of patients with nonocclusive thrombus and 10% of patients with occlusive thrombus. Clinical applicability of this strategy was further limited by unacceptably high rates of bleeding complications. Thus for nearly a decade, strategies of early thrombus removal were abandoned, because the immediate risks of the procedure outweighed the significant long-term morbidity of iliofemoral DVT.
In 1994 Semba and Dake were the first to demonstrate the effectiveness of catheter-directed thrombolysis using urokinase in the treatment of 21 patients with ileofemoral DVT. Complete lysis was achieved in 18 patients (72%) and partial lysis in 5 patients (20%). There were no major complications or clinically detectable PE. At 3 months, 12 limbs were studied with Doppler ultrasonography and veins were patent in 92%. Subsequent advancements in endovascular techniques have demonstrated the ability to achieve more effective clot removal while limiting systemic thrombolytic drug exposure and bleeding risks. In 2001 Kasirajan and colleagues demonstrated the potential value of percutaneous mechanical thrombectomy to achieve symptomatic relief and clot removal in ileofemoral DVT using a rheolytic AngioJet catheter (Medrad, Inc., Warrendale, Pa.). In 2006 Lin demonstrated that additional infusion of a thrombolytic agent via the AngioJet catheter increased the effectiveness of percutaneous mechanical thrombectomy in a technique referred to as power pulse spray mode. With limited risk and significant improvements in long-term clinical outcomes and venous patency, endovascular interventions should be considered for all healthy patients with proximal lower extremity DVT, good functional status, and reasonable life expectancy.
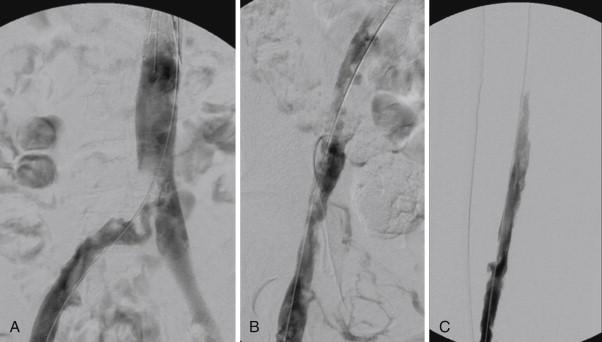
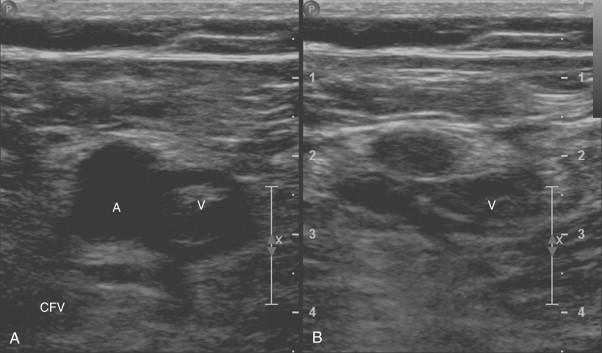
Preoperative imaging. Because isolated calf DVT is best managed with anticoagulation, thrombus within the iliofemoral system should be documented before the decision to intervene. Although venography remains the gold standard for both the diagnosis and the assessment of DVT, this test is invasive and is reserved as a confirmatory study during intervention ( Fig. 58-1 ). Alternatively, preoperative imaging with lower extremity duplex ultrasonography is noninvasive, convenient, and cost effective for the diagnosis of DVT ( Fig. 58-2 ). Duplex imaging has a sensitivity and a specificity of 95% and 97%, respectively, for diagnosing proximal lower extremity DVT. Ultrasonographic evidence of DVT includes noncompressible or partially compressible venous segments with continuous venous flow patterns that lack normally phasic flow variation.
Thrombophilia evaluation. Evaluation for inherited thrombophilia is indicated for patients who present under 50 years of age with an unprovoked DVT, a family history of thromboembolism, unusual thrombus location, or with a recurrent DVT. Screening should include evaluation for protein C or S deficiency, antithrombin deficiency, factor V Leiden, protein C resistance, prothombin gene mutation 20210A, hyperhomocysteinemia, and antiphospholipid antibody syndrome. Diagnosis of a thrombophilic disorder should prompt referral to a hematologist for long-term anticoagulation. A history of oral contraceptive use and malignancy should be sought, and evaluation for occult cancer should be considered.
Anticoagulation. Therapeutic anticoagulation with unfractionated heparin or low-molecular-weight heparin should be administered preoperatively once the diagnosis is established and blood is drawn for evaluation of an inherited thrombophilia. Full anticoagulation should continue throughout the procedure and for at least 6 months thereafter. Longer periods of anticoagulation may be necessary for treatment of an underlying thrombophilia.
Hemorrhagic complications. Bleeding complications have been substantially reduced with the introduction of catheter-directed endovascular therapy for thrombolysis. The use of thrombolytics enhances the success of intervention, but if the risk is deemed too high, percutaneous mechanical thrombolysis (PMT) may be performed with saline infusate alone.
Recurrent DVT. Treatment of recalcitrant thrombus and stenting of underlying lesions may reduce the risk of recurrent DVT.
Endovascular thrombolysis and thrombectomy procedures are ideally suited for early intervention. Patients can expect complete or near-complete clot and symptom resolution and preservation of venous valvular function if treated when symptoms have been present for less than 14 days.
Efficacy of DVT intervention decreases significantly as time from initial presentation increases. Several difficulties are encountered when attempting to treat chronic DVT. First, organized thrombus is often difficult to lyse even with aggressive treatment. Patients with chronic DVT and postthrombotic symptoms have also often developed venosclerosis, or diffuse venous scarring. In addition, damage to venous valves is likely irreversible after 14 to 30 days.
Nonetheless, venous recanalization and subsequent clinical improvement have been documented in patients with subacute and chronic DVT. In a series of 287 patients from the North American Venous Registry, complete lysis was achieved with catheter-directed thrombolysis (CDT) in 34% and 19% of patients with acute and chronic DVT, respectively. Significant partial lysis of greater than 50% was achievable in 64% and 47% of acute and chronic DVT patients, respectively. Better results have been obtained with the use of PMT alone or in combination with overnight CDT. Rao and associates reported that 17 patients (89%) with more than 14 days of symptoms underwent successful lysis and clinical symptom resolution. The two failures were in patients who were not considered candidates for adjunctive CDT after PMT. Ultrasound-accelerated thrombolysis led to partial lysis in 96% of acute DVT (<14 days), 100% of subacute DVT (15-28 days), and 78% of chronic (>28 days) and acute-on-chronic DVT cases.
Patients with subacute and chronic DVT may be candidates for treatment with pharmacomechanical thrombectomy and catheter directed thrombolysis if debilitating symptoms are present in otherwise healthy, functional patients, who have a reasonable life expectancy.
Access is achieved in the vein distal to the occluded segment. An ipsilateral femoral puncture may be sufficient for isolated iliac and femoral DVT. More extensive DVT, particularly involving the femoral-popliteal segments, is best accessed from the ipsilateral popliteal vein. It is essential to use ultrasound guidance to confirm venous entry, because blood return may not be obtained upon venous puncture secondary to occlusion of venous flow. Use of a micropuncture technique is recommended to minimize bleeding complications in an anticoagulated patient who will be further exposed to a thrombolytic agent. A venogram should be obtained and the lesion crossed with a 0.035-inch guidewire before any intervention is initiated.
Retrievable filters may be considered to prevent pulmonary embolization as the clot is disrupted ( Fig. 58-3 ). Approximately 30% to 40% of patients have thrombus in filters retrieved after intervention. The true incidence of symptomatic emboli is unknown but appears to be low.
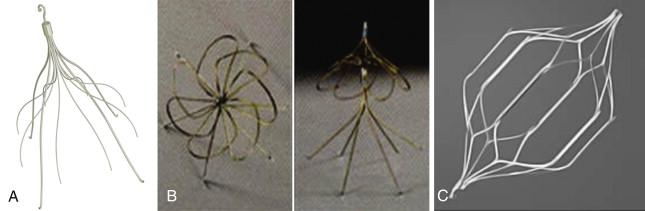
If a filter is used, it should be placed prior to intervention below the renal veins via a delivery route that is free of thrombus; most often from the contralateral femoral vein or right internal jugular vein. The filter can be retrieved at the end of the procedure or later if thrombus remains or a contraindication to anticoagulation exists.
A small multisidehole infusion catheter, such as a 4 or 5 Fr Uni-Fuse catheter (Angiodynamics, Latham, N.Y.) is advanced directly into the venous thrombus and secured at the most distal end of the thrombus load. The 4 Fr Uni-Fuse catheter is available in 90 and 135 cm lengths with infusion slit patterns of 5, 10, and 20 cm. The 5 Fr Uni-Fuse catheter is available in 45, 90, and 135 cm lengths with infusion slit patterns between 5 and 50 cm. Both catheters are compatible with a 0.035-inch guidewire. A thrombolytic agent is slowly administered while the patient is monitored in the intensive care unit (ICU). Blood sampling should be performed at 6-hour intervals to monitor hematocrit, platelet count, fibrinogen levels, and aPTT. Although debated, halting thrombolysis should be considered if fibrinogen levels fall below 150 mg/dL. The external portion of the catheter should be rolled into a coil that is secured under a transparent barrier film that should be monitored for hematoma formation. Repeat venography and assessment of clot lysis is performed at least once every 24 hours until complete lysis is achieved.
Tissue plasminogen activator (tPA, Activase, Genentech, South San Francisco) or recombinant tissue plasminogen activator (r-tPA, Retavase, PDL BioPharma, Fremont, Calif.), or tenecteplase (TNK, Genentech) are commonly used thrombolytic agents and no significant differences have been observed with regard to success rate or major complications. Recommended doses for continuous catheter-directed thrombolytic infusion include tPA 0.5 to 1.0 mg/hour, r-tPA 0.25 to 0.75 U/hour, and TNK 0.25 to 0.5 mg/hour. Concomitant heparin is delivered at 500 U/hour.
Successful clot lysis has been reported in 60% to 90% in patients with proximal DVT. Improvements in long-term venous patency and prevention of postthrombotic syndrome correlate with the degree of thrombolysis.
CDT allows lytic infusion at the location of venous thrombosis, thus maximizing effect and limiting overall drug dosages and systemic lytic exposure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here