Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
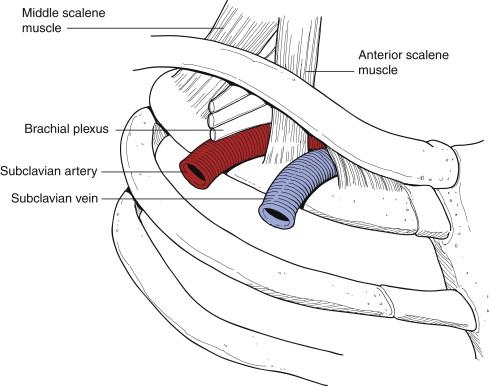
Subclavian-axillary vein thrombosis, also referred to as Paget-Schroetter syndrome or “effort thrombosis,” refers to primary thrombosis of the subclavian vein at the costoclavicular junction. Primary subclavian-axillary vein thrombosis is relatively rare, with a yearly incidence in the United States of 3000 to 6000 cases. A recent analysis suggests that less than 1000 first rib resections are performed for venous thoracic outlet syndrome yearly. This is a disorder of the anterior part of the thoracic outlet region, where the subclavian vein passes through the intersection of the clavicle and first rib ( Fig. 17-1 ), often seen in young, healthy patients who participate in vigorous activity that involves raising the arm above the head.
Paget was the first to describe “gouty phlebitis” of the upper extremity in 1875, which was a spontaneous thrombosis of the subclavian vein. von Schroetter postulated in 1884 that this entity resulted from a direct stretch injury to the vein caused by muscular strain. Hughes termed the condition Paget-von Schroetter syndrome in 1949.
Leaving this condition untreated results in residual upper extremity venous obstruction in up to 78% of cases and persistent symptoms and permanent disability in 41% to 91% and 39% to 68% of cases, respectively. Anticoagulation alone results in “excellent or good” long-term results in only 10 of 35 (29%) patients. Although significant differences exist, most recommend thrombolysis, followed by thoracic outlet decompression, most often by first rib resection. Decompression was initially thought best performed after an interval of a few months, but many now advocate immediate surgery to reduce the risk of rethrombosis. Secondary venous thrombosis is typically associated with a central catheter, with recommended treatment including anticoagulation and catheter removal.
True effort thrombosis almost always produces acute symptoms, and the patient usually presents to the clinic or emergency department with a swollen, blue, painful arm. Clinical clues include a history of vigorous activity, often with the affected arm overhead, and even if the onset of swelling is acute, a history of intermittent swelling, discoloration associated with activity, or both is common. Patients may have prominent chest wall or shoulder collaterals.
Duplex imaging should be performed to confirm the diagnosis.
If duplex is negative or equivocal, computed tomography or magnetic resonance venography can be considered. The patient with a duplex ultrasound venous thrombosis should be anticoagulated, with intravenous access established in the contralateral extremity.
Success of catheter-directed thrombolytic therapy rapidly decreases from onset of symptoms to intervention. Therefore, although not an emergency, treatment should be initiated within hours to a day or so after diagnosis unless contraindications exist. Although algorithms differ, pharmacologic or pharmacomechanical thrombolysis followed by transaxillary first rib resection during the same admission is an accepted approach. If thrombolysis is planned, pregnancy testing should be performed and renal function should be assessed.
Pulmonary embolism
Vessel perforation
Bleeding risk after thoracic outlet decompression is increased if surgery is performed within hours to days after thrombolysis.
Venous occlusion while awaiting thoracic outlet decompression may occur in 10% to 33% of patients if surgery is delayed for months, but is uncommon (5%) if surgery is performed within several days of thrombolysis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here