Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vidian neurectomy has been performed to relieve the symptoms of vasomotor rhinitis since the 1960s after being introduced by Golding-Wood as a transantral procedure.
Transnasal endoscopic vidian neurectomy was introduced by Kamel and Zaher and later refined by many, including El Shazly, El-Guindy, and Robinson and Wormald.
Better understanding of the anatomy with improving imaging modalities and better visualization of the operative field has led to decreasing complication rates and improving outcomes with endoscopic vidian neurectomies for vasomotor and allergic rhinitis.
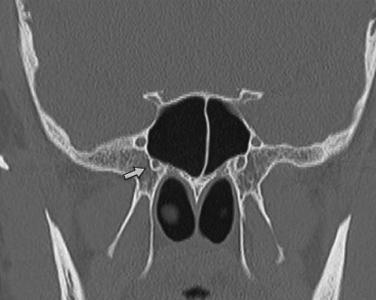
Understanding the anatomy of the vidian canal is a key element to the approach and thus the success of the procedure ( Fig. 23.1 ).
The vidian nerve is formed by the confluence of the greater superficial petrosal and deep petrosal nerves and travels in the pterygoid canal carrying the parasympathetic fibers, which synapse in the pterygopalatine ganglion, and the postganglionic fibers are distributed with the branches of the maxillary nerve.
Computed tomography (CT) scans allow for more precise appreciation of the location of the vidian nerve to the sphenoid sinus (type 1 and type 2 lying above or on the sphenoid sinus floor and type 3 canal being more embedded and deep).
The opening of the vidian canal into the pterygopalatine fossa is found at the junction of the medial pterygoid plate and the floor of the sphenoid sinus and is lateral to the smaller palatovaginal canal that houses the pharyngeal nerve, which runs in a medial to lateral direction.
Understanding the relationship of the vidian canal and the palatovaginal canal (lies inferomedial to the vidian canal transmitting the pharyngeal branches of the maxillary artery and pterygopalatine ganglion and is often mistaken for the vidian canal) is therefore vital for a successful outcome.
The main indication is for refractory vasomotor rhinitis in which topical measures have failed to give adequate relief for the patient or when the patient does not tolerate or is unwilling to continue with topical treatment, such as intranasal anticholinergic sprays.
Increasing evidence for the use of vidian neurectomy in both allergic and nonallergic rhinitis for control of watery rhinorrhea.
0-degree endoscope
Sickle knife or a scalpel with a No. 11 blade
Freer or Cottle dissector
Lusk 90-degree ball probe
2-mm upbiting Kerrison rongeur
Bipolar forceps
Bone wax (Ethicon, Somerville, New Jersey)
Surgicel (Ethicon, Somerville, New Jersey)
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here