Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The treatment of anterior skull base neoplasms has successfully evolved over the past few decades. Conventional approaches often employ open techniques involving transfacial dissection with or without frontal, bifrontal, pterional, or orbitozygomatic craniotomies. This may allow for en bloc resection of tumors at the expense of large cranial and possible dural defects necessitating reconstruction with regional tissue such as the pericranial or temporoparietal fascial (TPF) flaps. Although these approaches remain a viable option for large tumors, endoscopic endonasal approaches have become increasingly successful at treating the vast majority of patients with anterior skull base tumors, benign or malignant. Endoscopic resection of tumors has been shown to be safe and effective with oncologic outcomes similar to those of open approaches. Furthermore, the endoscopic endonasal approach has been shown to reduce postoperative hospital length of stay and improve recovery time with similar rates of survival, local recurrence, and complications. Despite these benefits, this approach can produce reconstructive challenges, especially in the setting of recurrent tumors and complex skull base defects as there is frequently no easy access to either the TPF or pericranial flap.
The underlying principle of reconstruction is to separate the cranial and sinonasal cavities to prevent cross-contamination, intracranial infections, and pneumocephalus. Early endoscopic reconstruction often used a dural substitute, either synthetic or autologous, in the reconstruction of the dural defect. Initial attempts at closure of these large defects often resulted in an unacceptably high postoperative cerebrospinal fluid (CSF) leak rate of upward of 30%. It was not until the use of vascularized sinonasal tissue that the postoperative CSF leak decreased to 5% or less. , Even with this improved outcome, challenges of endoscopic repair persist. The lack of supporting structures and effects of gravity on the reconstruction pose the greatest barriers for a robust repair. Numerous methods have been described to overcome this challenge, including balloon stabilization, peripheral buttressing techniques, gasket closure, and a bilayered button graft, with good reported outcomes. Regardless of the specific reconstructive method, success rates are similar and are based on surgeon experience and sound technique. The choice of repair technique is largely influenced by the size of the defect and the presence of a high-flow CSF leak. Postextirpation cranial base defects larger than 2 cm in diameter and those communicating with the ventricles or cisterns are considered high flow and generally require the use of vascularized tissue for coverage, such as a nasoseptal flap (NSF), since reconstruction with nonvascularized tissue has unacceptably high failure rates.
There are practically as many reconstructive techniques as there are institutions performing them. A common underlying theme is a primary dural repair with one of several techniques of stabilization, ideally covered by a pedicled vascularized mucosal graft. The choice of the approach is influenced by patient factors such as body mass index, comorbidities, tumor biology dictating the need for radiation or other adjuvant treatments, extent of resection, size of cranial base defect, communication with cisterns and ventricles, and surgeon experience with particular repair techniques. Outcomes depend on meticulous surgical technique with watertight closure of the dural defect and fixation of the grafts to prevent migration once placed. Endoscopic endonasal approach reconstruction techniques require thoughtful preoperative consideration of the expected cranial base defects and availability of postextirpation tissue to provide the best overall outcome.
Successful endoscopic repair of CSF leaks after resection of skull base tumors requires careful planning and consideration of the anticipated defect. Postextirpation cranial base defects can range in size and rate of CSF flow requiring variable reconstructive approaches. Regional vascularized tissue may be compromised in the setting of malignancy and prior surgery, necessitating the use of alternative sources of tissue for closure. Considering this, it is imperative to understand the biology of the underlying tumor and the extent of invasion of surrounding structures. This begins with careful evaluation of computed tomography and magnetic resonance imaging to assess the sinonasal anatomy and involvement of mucosa, including the nasal septum and turbinates. Assessment of the skull base anatomy is also important to anticipate the size and location of potential bony defects. However, even with careful planning, the final extent of the resection dictates the repair and can require intraoperative modification of the repair technique. Thus, it is important for the surgeon to be malleable and have a broad repertoire of repair options.
Anterior cranial fossa defects after endonasal tumor surgery commonly occur from resection of sellar or suprasellar pathology, including pituitary adenomas and craniopharyngiomas, anterior cranial base meningiomas, and sinonasal malignancies. In the case of primary intradural pathology, including craniopharyngiomas, giant pituitary adenomas, and tuberculum sellae or planum sphenoidale meningiomas, planned resection of the anterior cranial fossa bone and dura allows for a predictable defect requiring skull base reconstruction. In contrast, sinonasal malignancies pose a particular challenge because the neoplasm may involve the nasal septum or mucosa, resulting in a larger defect without viable local tissue for reconstruction. As many of these patients may have undergone previous endonasal surgery, review of prior operative notes and direct nasal endoscopy is essential to assess viability of autologous sinonasal tissue for repair techniques. Viable tissue for repair can also be limited in patients who have undergone prior irradiation, requiring the need for more complex reconstruction with more distant tissue, such as pericranium and TPF flaps, or vascularized free tissue transfer. The subsequent sections of this chapter address reconstruction considerations for specific pathologies.
Planning of the reconstruction is dependent on the expected extent and location of the cranial base defect and the characteristics of the CSF leak. CSF leaks can be classified based on size, pressure, and rate of flow. Typically a small defect is less than 1 cm in greatest diameter, a medium defect is 1 to 2 cm, and large defects are 2 cm or larger in greatest diameter. Whereas high-flow leaks are not consistently defined in the literature but can be considered to occur if the cranial base defect directly communicates with a ventricle or cistern, low-flow leaks do not involve these structures nor are they driven by elevated intracranial pressure (ICP). Patients with elevated ICP are also often referred to as having high-pressure leaks regardless of the size or communication with a ventricle or cistern highlighting the lack of consensus on the definition of high pressure versus high flow. A large cranial base defect with normal pressure but high CSF flow is frequently encountered after endoscopic resection of anterior cranial base tumors.
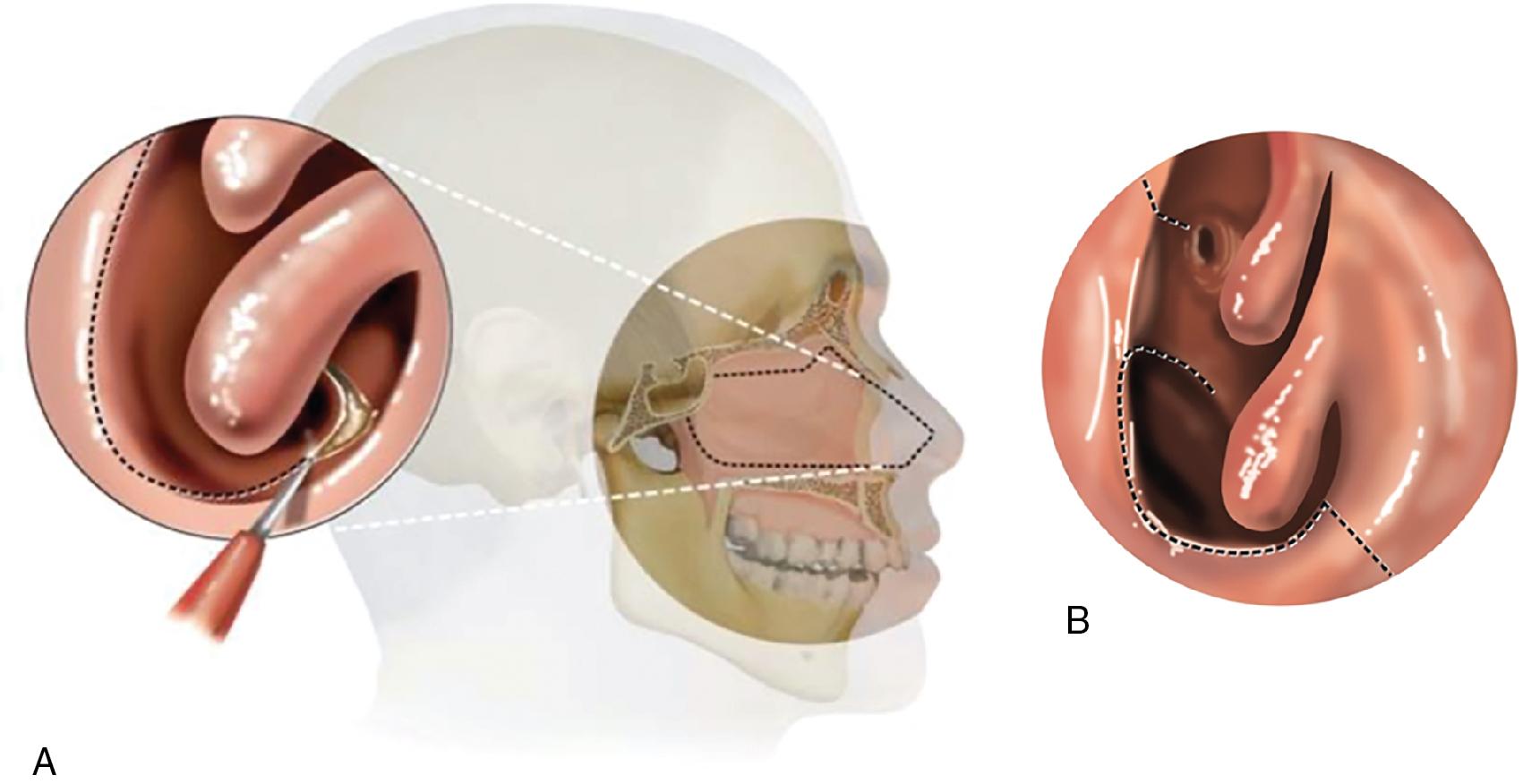
After standard preparation for endoscopic endonasal surgery, the nasal cavities can be decongested using oxymetazoline or epinephrine-soaked cottonoids. Local infiltration of mucosa using lidocaine with epinephrine provides hemostasis. Endoscopic evaluation of both nasal cavities and paranasal sinuses is performed to evaluate the extent of the tumor and availability for tissue for reconstruction. Depending on the planned size of the cranial base defect, a NSF can be raised, and tucked into the nasopharynx or maxillary sinus for protection ( Fig. 33.1 ). Further details regarding the use of a pedicled NSF are discussed in Chapter 29 . Surgical extirpation should then proceed with care to avoid undue tissue trauma, as well as careful preservation of the pedicle and blood supply to the NSF. Depending on the size of the anticipated defect, the NSF can be extended to include mucosa from the floor of the nose and the lateral nasal wall to increase width.
After resection of the tumor, careful evaluation of the defect should include inspection for the presence of a CSF leak and measurement of the defect. In cases in which the dura was not transgressed for tumor resection or removed as a margin, a leak may be occult. In this situation, a Valsalva maneuver or intrathecal fluorescein via lumbar drain can be used to identify any occult leak, though this is rarely necessary. Preparation of the cranial base is a key component to successful reconstruction. Depending on the site of the leak, a complete or limited sphenoethmoidectomy with or without maxillary antrostomy may be required to facilitate flap placement. Leaks involving the posterior table of the frontal sinus may require a Draf III frontal sinusotomy to provide access for reconstruction and to maintain frontal sinus outflow. After an adequate dissection is performed, the mucosa around the leak should be elevated to expose the surrounding bone and prevent entrapment of mucosa within the cranial cavity, which can lead to delayed formation of a mucocele.
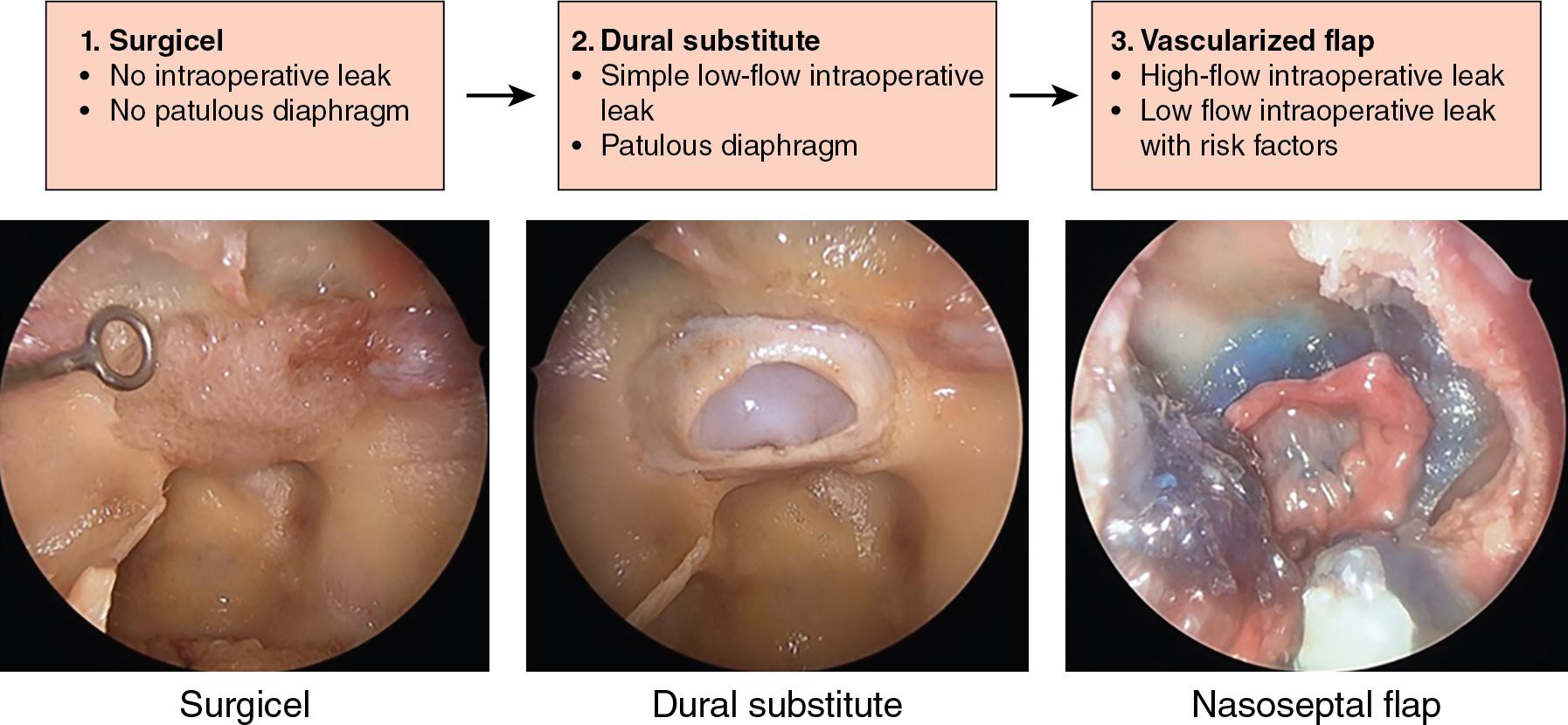
The occurrence of CSF leaks after endoscopic endonasal tumor resection varies from small leaks through the diaphragma sellae from resection of a pituitary macroadenoma to large anterior skull base defects resulting from tumors involving the anterior cranial base. Small defects with low CSF flow can typically be reconstructed in a minimalistic fashion. Leaks of this type are frequently encountered during endonasal pituitary surgery and can also occur from endonasal sinus surgery after iatrogenic injury. The authors manage reconstruction after removal of pituitary tumors using a three-tiered algorithm based on the presence or absence of intraoperative CSF egress, the status of the diaphragm sella, and the flow rates of the leak if present ( Fig. 33.2 ). For cases in which there is no intraoperative leak and the decompressed diaphragm is not displaced down to or through the dural opening, a simple reconstruction with an onlay of Surgicel (oxidized regenerated cellulose, Johnson & Johnson, New Brunswick, NJ) is used. If a low-flow CSF leak is encountered through the diaphragm or there is a patulous decompressed diaphragm displacing down to or through the dural opening, reconstruction is performed using an inlay dural substitute with biological glue. In the setting of a large defect with high-flow CSF leak, a more robust reconstruction is favored using an inlay dural substitute and vascularized flap, such as the NSF. A similar approach may be applied to leaks elsewhere along the anterior cranial base.
Many alternative dural reconstructive grafts are described in the literature. There are a range of synthetic, autologous, and nonautologous grafts that can be used as onlay grafts including collagen grafts, cadaveric dermis, and fascia lata. For small anterior skull base defects, autologous fat grafts have been used with success in the form of a “bath plug.” Additionally, free mucosal grafts can be harvested from the middle turbinate or nasal septum, or the nasal floor to be used as an onlay. , Onlay grafting typically requires some form of fibrin sealant or a bolster to prevent displacement of the graft into the nasal cavity. To prevent displacement, grafts may also be anchored between the dura and the skull base.
Large anterior cranial base defects can be encountered with endonasal resection of tumors and present a reconstructive challenge. Regardless of the rate of flow of the leak, a multilayered closure is necessary for adequate repair. The general principle for management of these defects involves dural reconstruction followed by a vascularized onlay flap. The authors favor the use of a bilayer button graft for primary dural reconstruction, designed from autologous fascia lata with the two layers sutured together and placed as an inlay–onlay repair ( Fig. 33.3 ). This graft has the advantage of being harvested from an autologous source, has minimal risk of migration, and can be used effectively for defects with multiple planes (e.g., defects transitioning between the tuberculum sella and planum sphenoidale). Importantly, the button graft doubles the surface area for healing, and it can safely be used around critical neurovascular structures without the requirement of a rigid buttress.
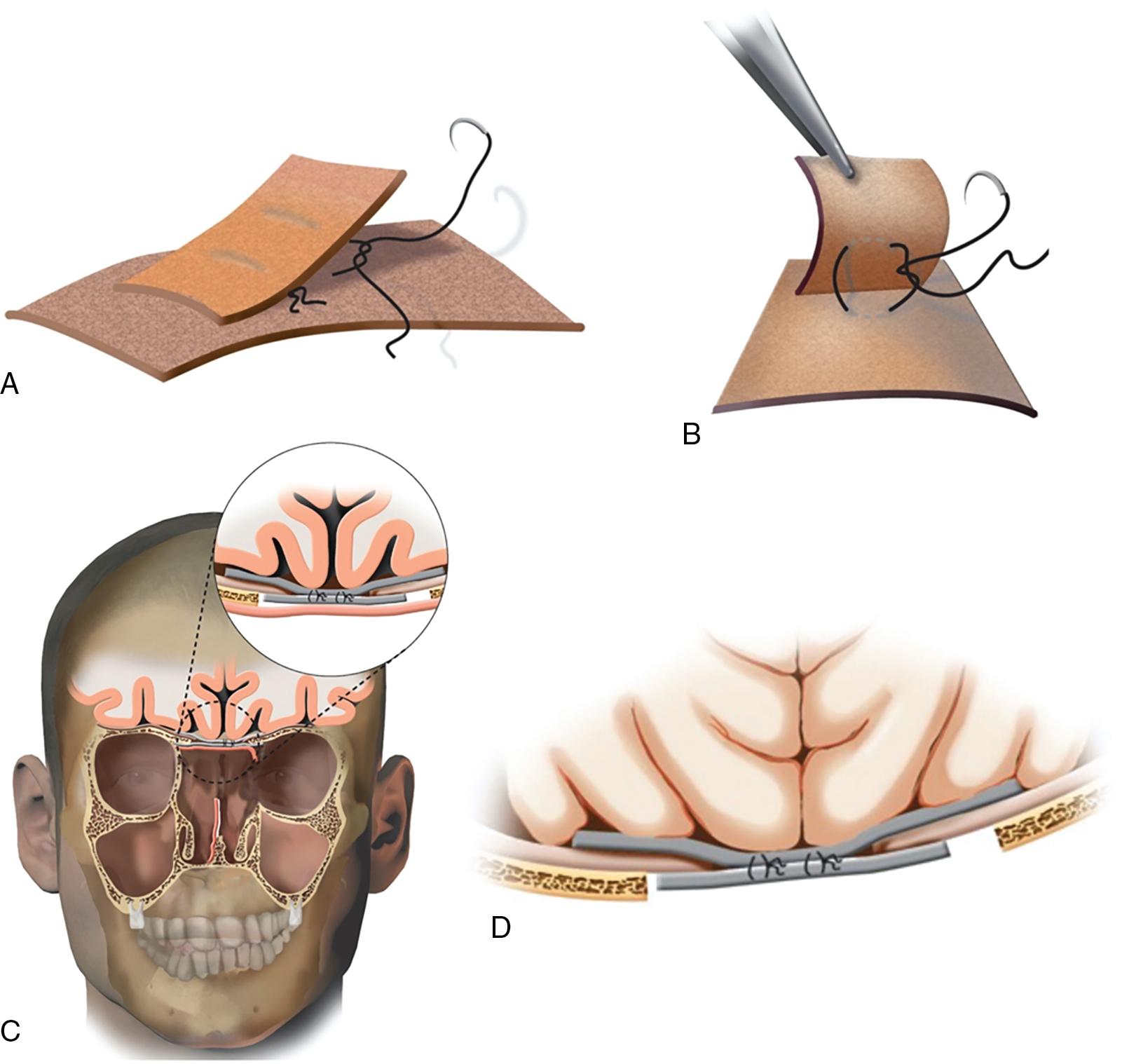
After a tumor is resected, the skull base must be prepared for reconstruction. The mucosa is dissected sufficiently around the bony defect so as to avoid trapping beneath the repair to prevent delayed mucocele formation. Of note, mucosa removal must also be considered for the recipient site and pathway of other repair layers, such as a NSF. The size of the bony defect is measured, and an appropriate size fascia lata graft is harvested such that the inlay portion of the button graft is designed to be 25% to 30% larger than the dural defect, and the onlay portion is designed to be only slightly larger than the dural defect. The two grafts are then are sutured together using four 4-0 Nurolon (Ethicon, Raritan, NJ) nylon sutures (see Fig. 33.3 ). This bilayered graft can then be tucked into the defect, with the larger portion lying flat in the subdural space along the anterior cranial fossa and the smaller portion covering the defect externally as an onlay. After the fascia lata graft has been appropriately placed, the graft will pulse like the surrounding dura, and there will be no evidence of CSF leakage around the graft. A vascularized flap, such as a NSF or superiorly based septal flap, is then harvested and placed on top of the button graft to assist with repair and mucosalization. The button graft doubles the surface area of dural healing and does not require packing to bolster the reconstruction. The authors place a layer of dural sealant (DuraSeal, Integra LifeSciences, Princeton, NJ) along the edges of the NSF to prevent any motion of the flap until it scars down to the surrounding tissue. If needed, a piece of NasoPore® (Stryker, Kalamazoo, MI) can be placed centrally to reinforce the NSF, but this is not critical.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here