Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Elbow arthroplasty was first developed for patients with end-stage articular destruction secondary to inflammatory arthropathy, mostly rheumatoid arthritis (RA). In fact, the long-term performance of elbow arthroplasty has mostly been tested in inflammatory conditions. However, the pharmacologic treatment of RA has improved substantially over the last two decades. As a result, the number of patients with inflammatory conditions that eventually require an elbow arthroplasty seems to be decreasing. On the other hand, as detailed later, treatment with modern disease-modifying antirheumatic agents may increase the risk of infection with any surgical procedure. Finally, contemporary rheumatoid patients subject their implants to higher mechanical demands, partly because of societal changes and partly because of being much more active than the classic rheumatoid patient with polyarticular destruction.
Chapters 77 and 78 provide a great overview of inflammatory elbow conditions, their evaluation and overall management. This chapter focuses specifically on technical aspects and the overall outcome of elbow arthroplasty in inflammatory conditions. Juvenile idiopathic arthritis (JIA) (also known as juvenile RA) presents a number of particularities that deserve specific attention, and the role of elbow arthroplasty in juvenile rheumatoid patients will be discussed separately.
When a rheumatoid patient is referred to the orthopedic surgeon for a surgical consultation regarding the elbow joint, the evaluation should not only assess the affected elbow in detail but also determine involvement of other joints in the upper extremity (shoulder, wrist, hand), as well as the cervical spine (it may impact anesthesia techniques) and the lower extremities, as the use of assistive devices may increase the loads across the elbow joint.
On inspection, some patients may present with rheumatoid nodules, olecranon bursitis, and various amounts of swelling secondary to synovitis. The condition of the skin may also be affected by chronic use of steroids, malnutrition secondary to systemic problems, or previous surgical procedures.
Elbow range of motion is assessed and recorded in flexion, extension, pronation, and supination. Elbow stability is assessed by stressing the elbow into varus and valgus to detect attenuation of the medial and lateral stabilizing structures. Special attention should be paid to examination of the ulnar nerve for both motor and sensory changes; not uncommonly, the ulnar nerve is involved by synovitis, bony changes and angular deformity. Pain related specifically to the radial head may be assessed by trying to reproduce pain with pronation and supination or by flexing and extending the elbow with a valgus torque. In patients with previous surgical exposures that may have violated the extensor mechanism, careful examination of the triceps is required to determine its integrity.
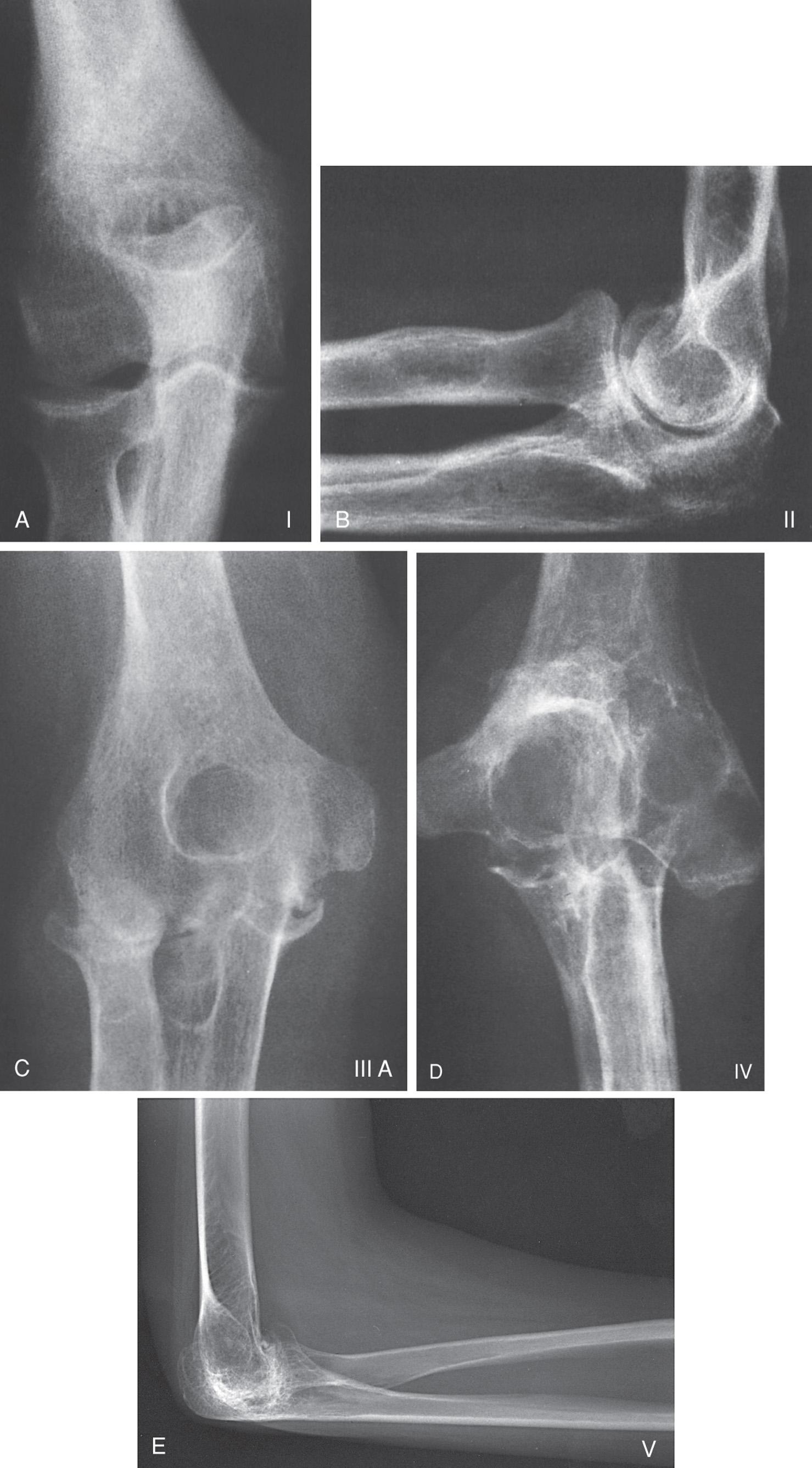
Plain radiographs are the main imaging modality used for the evaluation of most rheumatoid elbows ( Fig. 91.1 ). Typical findings may include various degrees of joint line space narrowing, osteopenia, cysts, and structural bone loss in the distal humerus, proximal ulna and/or proximal radius. Radiographic changes may be graded using the Larsen evaluation system ( Table 91.1 ), which can be used for any joint involved. More commonly, we use the Mayo classification system, specifically designed to classify the rheumatoid elbow in various degrees of severity ( Table 91.2 , Fig. 91.2 ). Advanced imaging studies are selectively used. Computed tomography scans are useful in planning joint débridement procedures, commonly performed arthroscopically. Magnetic resonance imaging offers the greatest sensitivity for detecting synovitis and early bone and cartilage changes.

| Grade 0 | Normal radiographs |
| Grade 1 | One or more of the following are present: periarticular swelling, periarticular osteoporosis, mild joint space narrowing |
| Grade 2 | One or more small erosions (typically under 1 mm) |
| Grade 3 | Large erosions |
| Grade 4 | Severe destructive abnormality |
| Grade 5 | Complete absence of the articular cartilage, destruction of the original bony outline, mutilating changes |
| I | Osteopenia, subchondral cysts, and synovitis without marked joint line space narrowing |
| II | Joint line space narrowing with preservation of the overall bony architecture |
| III | Moderate bone loss affecting one (IIIA) or both (IIIB) humeral columns |
| IV | Complete disintegration of the elbow joint with dysfunctional instability ( mutilans RA) |
| V | Ankylosis secondary to juvenile RA |
Elbow surgeons should be familiar with the overall management strategies for inflammatory arthritis and work in close collaboration with a rheumatologist (see Chapters 77 and 78 ). Pharmacologic options to treat RA have changed tremendously over the last few years. Currently, nonsteroidal antiinflammatory drugs (NSAIDs) and steroids are used mostly as adjunctive drugs, and most patients benefit from so-called disease-modifying antirheumatic drugs (DMARDs). DMARDs are classified as conventional (e.g., methotrexate [MTX]) or biologic (e.g., anti-tumor necrosis factor [anti-TNF], interleukin-1 [IL-1] and interleukin-6 [IL-6] receptor antagonists, T-cell blockers, and B-lymphocyte modulators).
Most patients are started on MTX with the addition of a biologic DMARD for nonresponders. Patients may be switched between various biologic DMARDs depending on their response, while maintaining MTX in the background. Corticosteroids are used when DMARDs are first introduced, in order to control symptoms while the DMARDs are becoming effective (typically 4 to 6 weeks), as well as for episodes of flare-up; they are rarely used chronically for patients not responding to anything else. Intraarticular injections with steroids may also be considered when inflammatory symptoms at the elbow flare up. NSAIDs are selectively used for pain control.
A comprehensive program of physical therapy also seems to improve overall muscle strength and perceived health status for patients with RA. However, physical therapy per se has little value for the rheumatoid elbow prior to surgery. Selective use of elbow braces that splint the elbow in extension overnight may help those patients developing a flexion contracture.
Patients not responding to nonoperative modalities as described previously should be considered for surgery. The main indications for surgery in patients with inflammatory arthritis of the elbow are (1) inability to provide adequate pain relief with nonoperative treatment, (2) stiffness that interferes with the ability to perform activities of daily living, (3) gross instability leading to marked dysfunction, and/or (4) progression of disease with almost catastrophic bone loss compromising future surgical options or leading to impending fracture. Various procedures may be considered for surgical treatment of the rheumatoid elbow, including synovectomy and débridement, total elbow arthroplasty, and interposition arthroplasty. The indication for each of the procedures is mostly based on disease severity, patient's age, activity level, and expectations. Other chapters of this book review synovectomy and interposition arthroplasty.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here