Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Earache (otalgia) is pain that arises from a pathologic process in the external, middle, or inner ear or that is referred to the ear from another structure. Acute otitis media (AOM) is the most common cause of otalgia in children ( Table 5.1 ). At least 80% of children will experience one or more episodes of AOM in the first 3 years of life. The second most common cause of ear pain is otitis externa, followed by dermatitis and infections of the pinna ( Table 5.2 ). Other causes of otalgia are rare ( Table 5.3 ). A careful examination of the pinna, external auditory canal, and tympanic membrane can identify most causes of ear pain. When the findings are normal, referred pain should be considered ( Table 5.4 ).
| Disorder | Clinical Features |
|---|---|
| Acute otitis media | Immobile tympanic membrane that may appear bulging, red, and/or opaque |
| Bullous myringitis | Hemorrhagic or serous bullae on the tympanic membrane; more severe pain than acute otitis media |
| Mastoiditis | Tenderness and erythema over mastoid with periostitis process; no destruction of bone trabeculae |
| Acute mastoid osteitis | Destruction of bone trabeculae; tenderness and erythema over mastoid process coupled with outward displacement of pinna |
| Granulomatosis | Severe necrotizing vasculitis; ulcerative and destructive granulomatous lesions of upper and lower respiratory tract with polyangiitis |
| Langerhans cell histiocytosis | Pituitary dysfunction, exophthalmos, seborrheic dermatitis, and bone lesions; if bone lesions involve the ear, patient presents with mastoid tenderness and otorrhea |
| Disorder | Clinical Features |
|---|---|
| Acute otitis externa | Diffuse redness, swelling, and pain of the canal with greenish to whitish exudate; often very tender pinna |
| Necrotizing (malignant) otitis externa (± skull base osteomyelitis) | Rapidly progressive, severe swelling and redness of pinna; pinna may be laterally displaced; risk factors include diabetes mellitus, congenital or acquired immunodeficiency, severe neutropenia |
| Dermatitis | |
|
History of atopy, presence of lesions elsewhere; lesions are scaly, red, pruritic, and weeping |
|
History of cosmetic use or irritant exposure; lesions are scaly, red, pruritic, and weeping |
|
Scaly, red, papular dermatitis; scalp may have thick, yellow scales |
|
History or presence of psoriasis elsewhere; erythematous papules that coalesce into thick, white plaques |
| Cellulitis | Diffuse redness, tenderness, and swelling of the pinna |
| Furuncles | Red, tender papules in areas with hair follicles (distal third of the ear canal) |
| Infected periauricular cyst | Discrete, palpable lesions; history of previous swelling at same site; cellulitis may develop, obscuring cystic structure |
| Insect bites | History of exposure; lesions are red, tender papules |
| Herpes zoster oticus | Painful, vesicular lesions in the ear canal and tympanic membrane, hearing loss, vestibulitis; with addition of seventh cranial nerve palsy—Ramsay Hunt syndrome |
| Perichondritis | Inflammation of the cartilage, usually secondary to cellulitis |
| Relapsing polychondritis | Recurrent episodes, involves other cartilage sites (nose) |
| Granulomatosis with polyangiitis | Fever, weight loss, respiratory and/or renal manifestations |
| Tumors including Langerhans cell histiocytosis | Palpable mass, destruction of surrounding structures |
| Foreign body | Foreign body may cause secondary trauma to the ear canal or become a nidus for an infection of the ear canal |
| Trauma | Bruising and swelling of external ear; there may be signs of basilar skull fracture (cerebrospinal fluid otorrhea, hemotympanum) |
| Intrinsic |
|
|
|
|
| Extrinsic |
|
|
|
|
|
|
|
|
|
|
|
|
| Neck |
|
|
|
| Salivary Glands |
|
| Thyroid |
|
| Teeth and Gums |
|
|
|
|
| Temporomandibular Joint |
|
|
|
| Tonsils |
|
|
|
| Pharynx |
|
| Paranasal Sinuses |
|
| Other |
|
|
|
Older, verbal children with ear pain are often able to localize and accurately describe their symptoms. Younger children often cannot localize their pain and may present with a variety of nonspecific symptoms, including fever, irritability, emesis, rhinorrhea from an associated upper respiratory tract illness (URI), and ear rubbing or pulling. Even though ear pulling is associated with ear pain, it is neither specific nor sensitive in the diagnosis of ear disease . In addition, infants with AOM may occasionally be afebrile and present with various degrees of irritability, such as sleep disturbances and/or eating or drinking inadequately. Ear disease should be considered in infants during the first year of life or in any preschool child with fever, irritability, or a URI.
In taking a history from a child who presents with ear pain, true ear pain must be distinguished from the sensation of fullness and discomfort that children experience when they have an effusion or retracted tympanic membrane secondary to a dysfunctional eustachian tube. The clinician should review the child’s history for factors placing the child at risk for infection such as craniofacial abnormalities (e.g., cleft palate), immunodeficiencies, autoimmune disease, diabetes, previous ear infections, placement of tympanostomy tubes, and recent dental procedures, trauma, and air travel. Immunization status should also be reviewed. A careful review of systems should elicit associated fevers, sore throat, reflux symptoms, otorrhea, neurologic symptoms, and symptoms of sinusitis. Children with a middle ear effusion may have decreased hearing acuity.
Acute otitis media presents with abrupt onset of otalgia associated with middle ear fluid, signs and symptoms of inflammation, and local or systemic infection. Risk factors for AOM include a family or personal history of recurrent AOM, trisomy 21, household cigarette smoke exposure, lack of breast-feeding, lower socioeconomic status, males, cleft palate, immunodeficiency, and group daycare attendance or siblings in the household. Children with otitis externa (“swimmer’s ear”) present with either ear pain, purulent otorrhea, or both as well as ear fullness, localized ear pain with mastication, and ear itching. Relapsing polychondritis is a rare multisystemic inflammatory disorder that targets cartilaginous structures throughout the body. If the external ears are involved, symptoms may include episodic swelling and redness of the pinnae that is usually bilateral and recurrent. Other cartilaginous structures are often affected, though if findings are unilateral and subtle, the disorder may mimic otitis externa and the diagnosis may remain elusive until symptoms recur. With referred ear pain, such as from tooth decay or teething, there are often additional symptoms associated with the respective head and neck structures (see Table 5.4 ). Patients with ear pain secondary to maxillary sinusitis may also complain of headaches and purulent rhinorrhea.
In a child presenting with a chief complaint of ear pain, the general examination includes the temperature, the respiratory rate, and a determination of whether the infant or child has a toxic appearance. Then the clinician proceeds with the complete head, eyes, ears, nose, oral cavity, and throat examination and with an appropriately focused physical examination of other pertinent systems.
The examination of the ear begins with the less symptomatic ear. The clinician should inspect the pinna and adjacent tissues for dermatitis, redness, and edema. The mastoid process and the pinna, including its cartilaginous portions, are palpated for any tenderness. Erythema, swelling, and tenderness over the posterior auricular mastoid process suggest mastoiditis , whereas localization of these findings to the external auditory canal and the pinna suggests otitis externa. In both conditions, the swelling may be so severe that the pinna is laterally displaced. The opening of the external ear canal is also examined for the presence of discharge or exudate. Manipulating the tragus and pinna causes extreme pain with otitis externa. Most disorders of the external ear can be detected through this examination (see Tables 5.2 and 5.3 ).
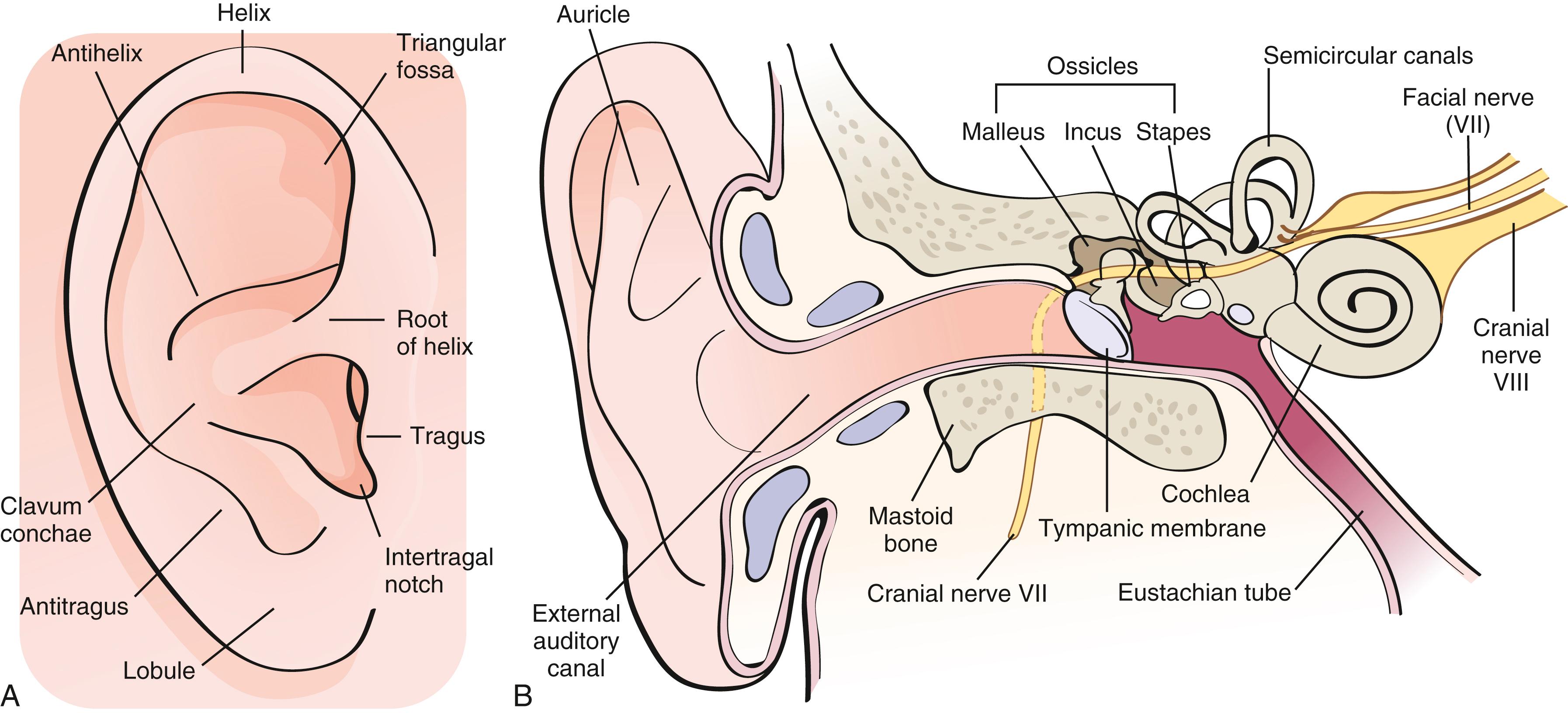
Otoscopy provides an opportunity to indirectly view the middle ear through the tympanic membrane. The middle ear is normally an air-filled cavity that transmits sound from the eardrum to the ossicle and then into the internal ear ( Fig. 5.1 ). Otoscopy begins by properly positioning and, if necessary, gently restraining the patient. Both shoulders and hips need to be stabilized so that the patient cannot roll during the examination. Infants are best examined on an examining table in the prone position, with a parent or an attendant firmly holding the patient’s shoulders, thus preventing the patient from moving. Toddlers should sit on a parent’s lap, with the examiner sitting in a chair opposite them. The child is held against the parent’s chest, with one of the parent’s hands and arms holding the child’s arms and the other around the child’s head so that one ear is exposed. To avoid trauma with movement, the otoscope should be held in the examiner’s hand making direct contact with the patient’s head, allowing the otoscope to move with the head.
Cerumen (ear wax) is a waxy substance consisting of glandular discharge from cells in the outer external canal mixing with exfoliated epithelial cells. Cerumen can both obscure visualization of the eardrum leading to diagnostic errors and be a cause of otalgia if impaction occurs. To view the eardrum properly, the examiner should remove the wax by irrigating the ear canal gently with lukewarm water, lifting the wax out with a blunt curette, or dissolving the wax by placing 1–2 drops of docusate sodium liquid in the canal for 10–15 minutes. Contraindications for irrigation or use of a cerumenolytic solution are the presence of a tympanostomy tube, a perforated tympanic membrane, or an organic foreign body (e.g., legumes swell in contact with fluids).
During the insertion of the speculum, the clinician should note any redness, edema, tenderness, exudate, furuncles, or vesicles that may be present in the external auditory canal. In some illnesses such as otitis externa, the ear canal may be so edematous that the speculum cannot be inserted, and the eardrum cannot be seen. In addition, in neonates and in some children with craniofacial anomalies such as trisomy 21 or Goldenhar syndrome, the external canal may be so small that it precludes an accurate assessment of the tympanic membrane.
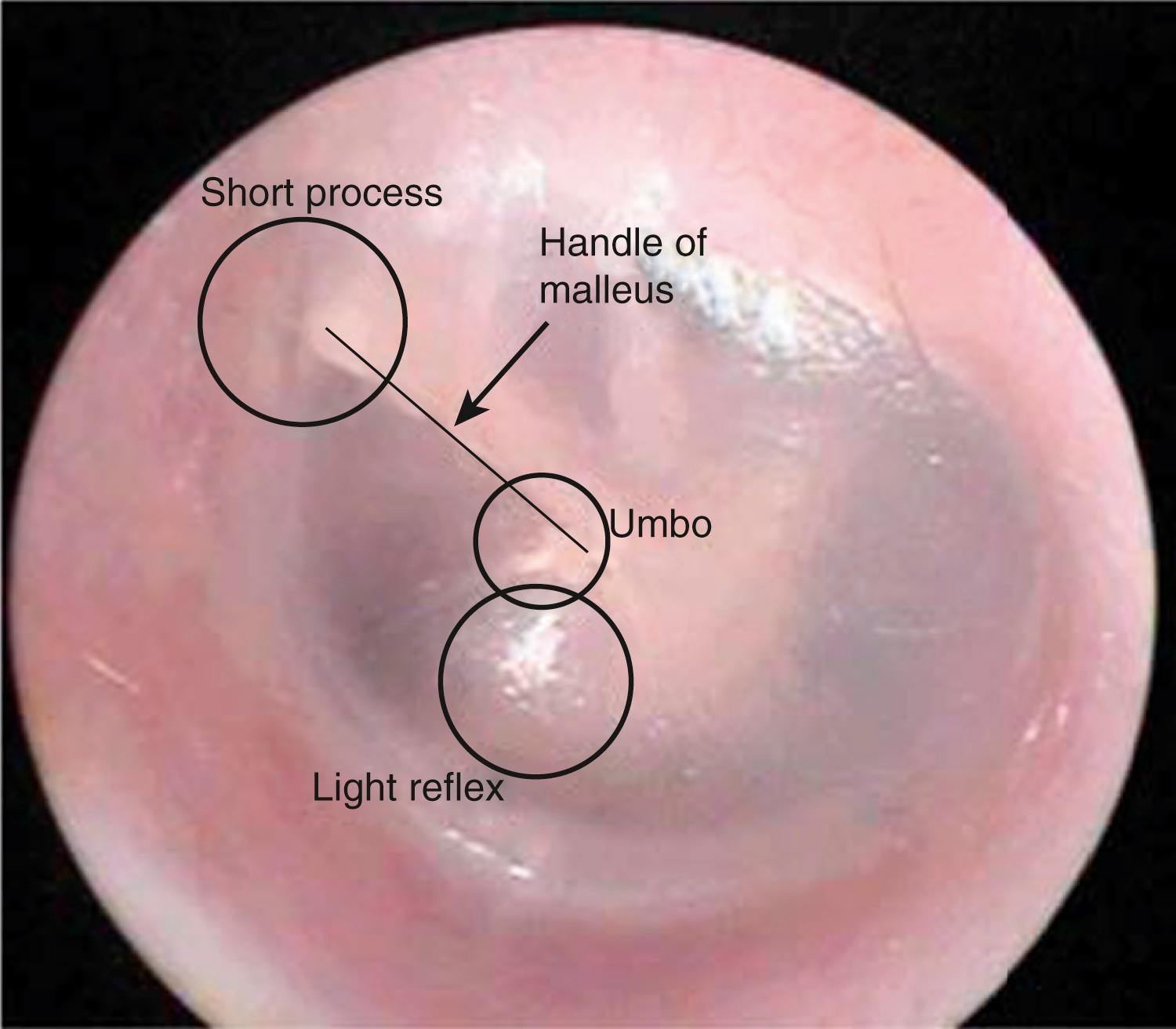
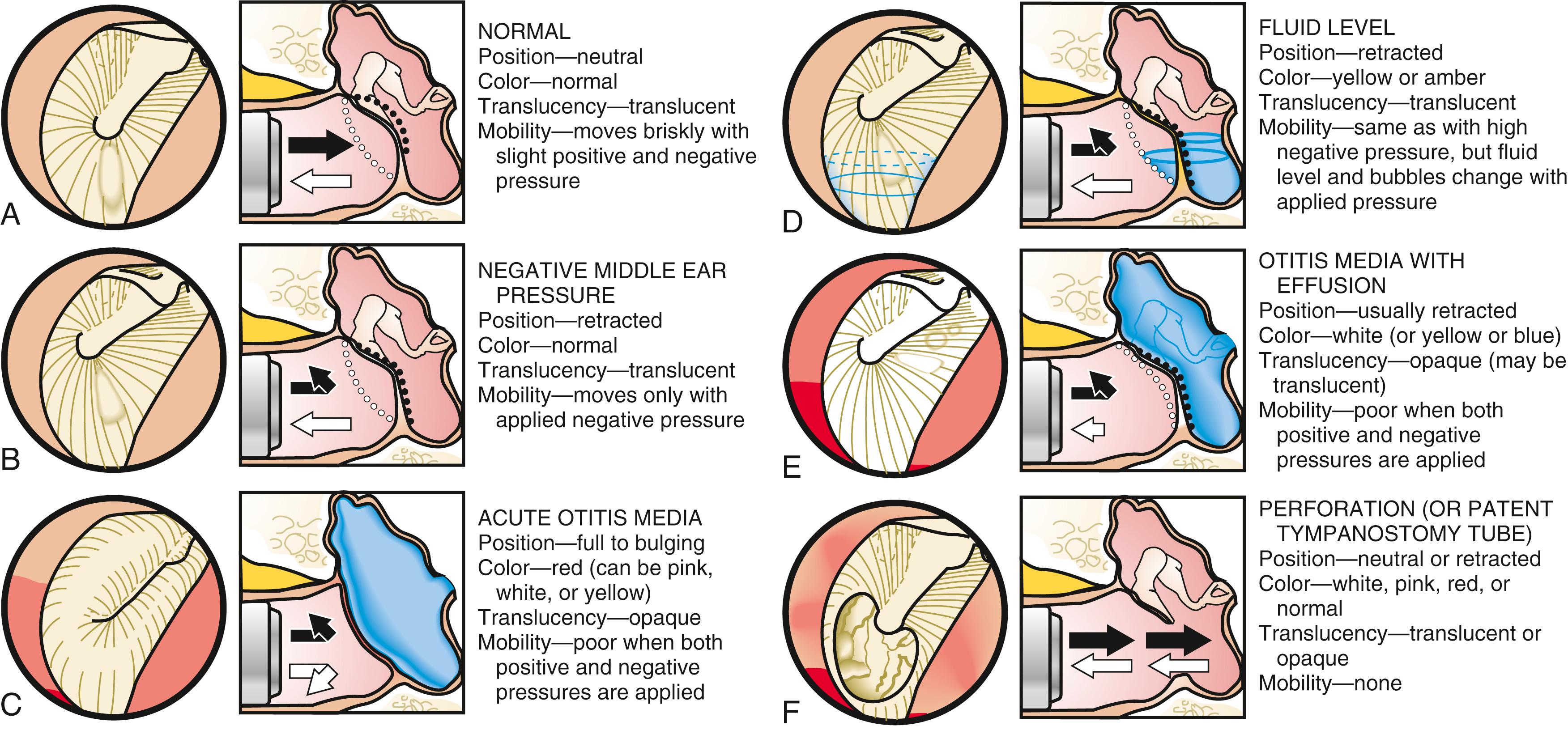
Pneumatic otoscopy allows evaluation of the tympanic membrane’s mobility. Because it is more accurate than otoscopy alone in detecting middle ear effusion, pneumatic otoscopy should be part of every ear examination. In performing pneumatic otoscopy, the examiner should select a speculum that fits snugly in the external auditory canal. The examiner then partially depresses the rubber bulb of the pneumatic otoscope and inserts the otoscope into the ear canal ( Fig. 5.2 ). Once the eardrum is seen, the examiner should observe the color, appearance, position, bony landmarks, and mobility of the tympanic membrane ( Table 5.5 and Fig. 5.3 ). If the eardrum is not perforated, the clinician observes its mobility by alternating positive and negative pressure by gently depressing and releasing the bulb of the pneumatic otoscope. Poor mobility of the eardrum may be secondary to middle ear effusion, a perforated tympanic membrane, or lack of an airtight seal ( Fig. 5.4 ).

| Characteristic | Normal Findings | Acute Otitis Media | Otitis Media with Effusion | Comments |
|---|---|---|---|---|
| Color | Gray to pink | Often red from inflammation; yellow to white from purulent fluid behind tympanic membrane | Usually gray to pink, but may still be yellow or white; not red | Interobserver variation of color is high; redness can occur from crying alone |
| Appearance | Translucent | Opaque | Translucent or opaque | Opacity is caused by opaque fluid or by scarring of tympanic membrane |
| Position | Neutral | Fluid under pressure produces bulging of tympanic membrane; bony landmarks may be distorted and the light reflex lost | Not bulging; may be retracted | |
| Mobility | Tympanic membrane moves freely | Mobility to positive and negative pressure reduced | Mobility to positive and negative pressure reduced | |
| Other findings | Perforation with otorrhea |
In neonates and young infants, the eardrum is less perpendicular to the observer, the bony landmarks are less distinct, and the eardrum is less mobile than in older infants and children. Failure to appreciate these normal otoscopic findings may lead to the overdiagnosis of middle ear effusion.
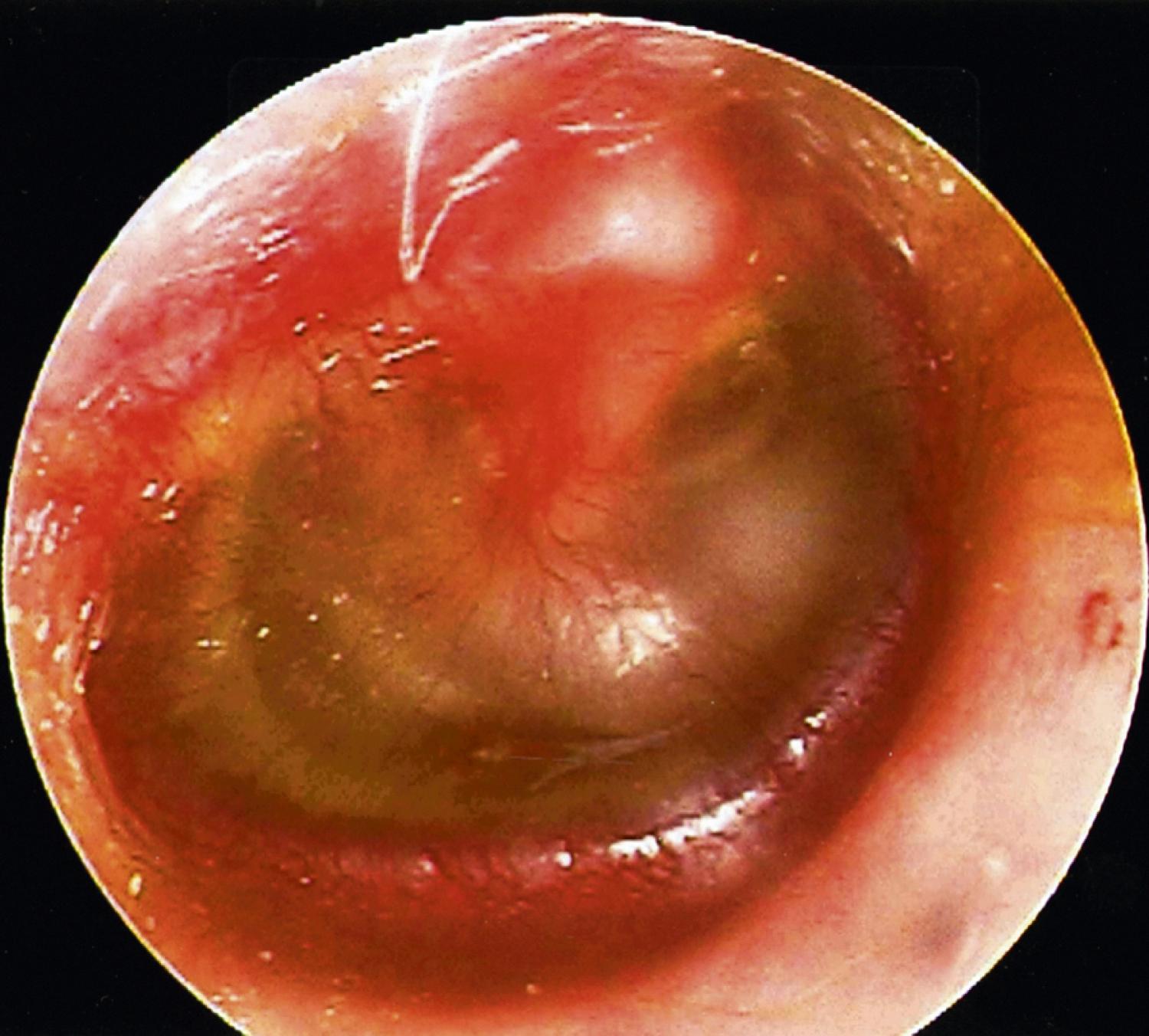
In the first few hours of AOM, the middle ear cavity may not yet be filled with fluid, and the mobility may be normal. By the time the patient is examined, though, the middle ear is usually filled with fluid, and the eardrum is opaque and bulging with decreased mobility (see Fig. 5.4 ). A reddened eardrum may indicate inflammation of the tympanic membrane (TM), but this physical finding is not specific because crying alone can induce diffuse redness of the eardrum. In addition, differentiation of color is highly variable among observers, which may in part result from the intensity and type of light source used in otoscopy.
In otitis media with effusion (OME) , also known as serous otitis media, the cardinal sign is decreased mobility of the eardrum. The eardrum may be opaque, but not bulging or grossly inflamed (see Fig. 5.5 and Table 5.5 ). A challenge for the clinician is the child with symptoms consistent with AOM (ear pain) but with the physical findings of OME. In such cases, it is difficult to decide whether there is an acute infection of the middle ear or whether it is OME with an illness at another site causing the symptoms.
When the external ear and tympanic membrane are normal in a child with an earache, the clinician must consider the possibility of referred pain (see Table 5.4 ). Innervation of the external and middle ear includes pain fibers of the trigeminal, glossopharyngeal, and vagus nerves and, to a lesser extent, the facial nerve and upper cervical nerves. The clinician should examine the neck, parotid gland, thyroid, mouth, tongue, teeth, temporomandibular joint, tonsils, and throat. In children, the cause of referred pain is usually infectious rather than noninfectious (e.g., a tumor).
Routine cultures of middle or external ear fluid are not required because most infections are self-limited and respond to empiric antimicrobial therapy. In selected instances (e.g., persistent treatment failure, severe pain, an immunocompromised host, a neonate), culture of otorrhea from the external auditory canal or cultures of middle ear fluid by tympanocentesis may guide therapy. In a child with AOM, the offending pathogen is usually also present in the nasopharynx. Unfortunately, nasopharyngeal cultures are not helpful in directing therapy because multiple pathogens are typically isolated, and it is unclear which organism is actually causing the middle ear infection. With the emergence of strains of Streptococcus pneumoniae that are resistant to commonly used antibacterials, the incidence of treatment failures may increase. This increasing rate of treatment failure may necessitate a greater reliance on tympanocentesis for culture of middle ear fluid to determine the appropriate antimicrobial agent.
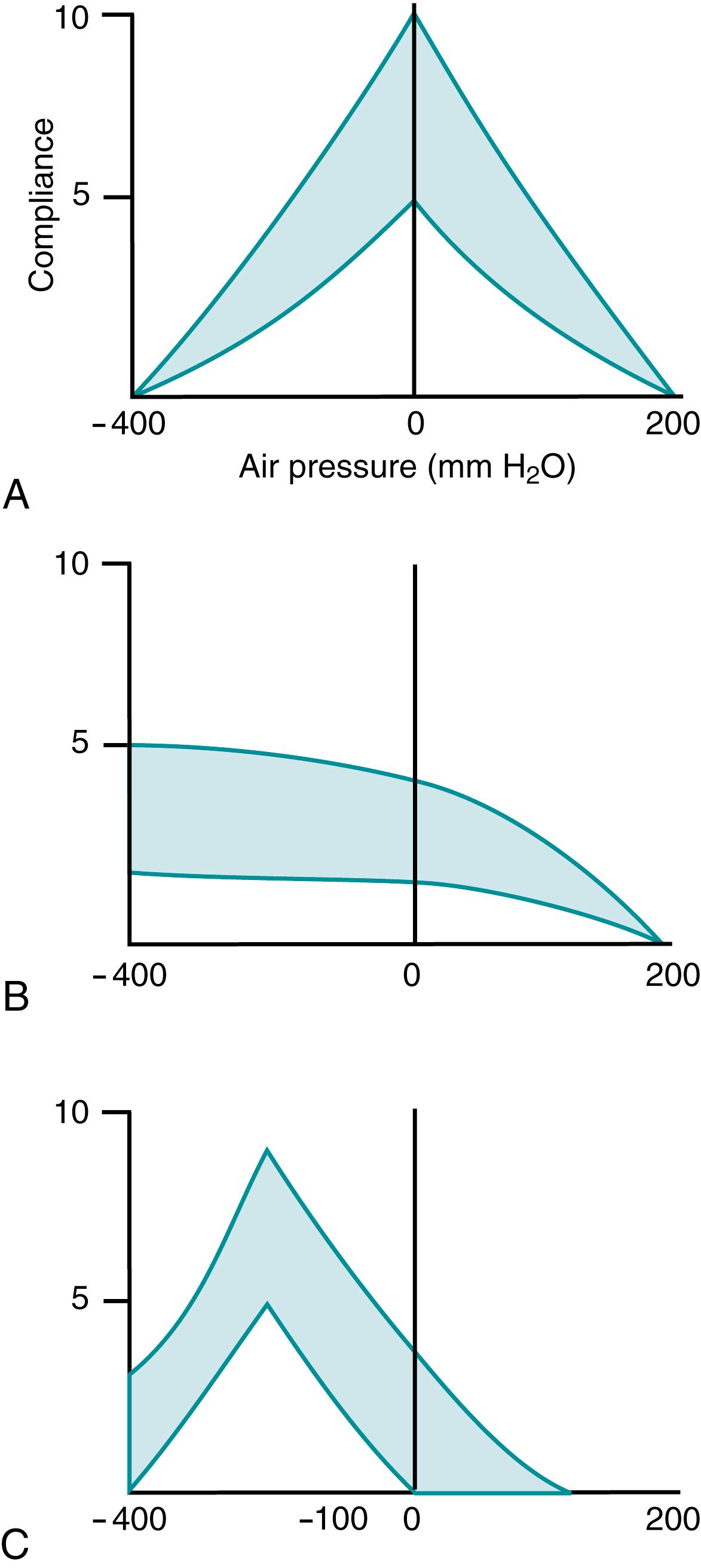
Tympanometry is an objective, painless method for detecting the presence of middle ear effusion by providing information about tympanic membrane compliance. A soft plastic probe is inserted into the external auditory canal to obtain an airtight seal. The tympanometer measures the flow of sound energy into the middle ear under conditions of changing air pressure. When the air pressure is equal on both sides of an intact eardrum, with the drum in neutral position, the transmission of sound energy through the tympanic membrane is at its maximum. The peak on the tympanogram represents the pressure at which the flow of sound energy is maximal. For example, in a normal air-filled middle ear cavity, the peak occurs at ambient atmospheric pressure ( Fig. 5.6 A ). With eustachian tube dysfunction (a retracted eardrum but no middle ear effusion), the peak occurs in the negative pressure range on the recording ( Fig. 5.6 C ). With middle ear effusion, the sound energy flowing into the middle ear is reduced, which produces a flat tympanogram ( Fig. 5.6 B ). A flat tympanogram may also result from cerumen, a foreign body, or occlusion of the opening of the probe by the wall of the external auditory canal. In these circumstances, the tympanogram is flat and the estimated volume of the ear canal is lower than anticipated. In a perforated eardrum, the sound energy is readily transmitted through the hole in the drum throughout the entire pressure range, resulting in a flat tympanogram with a higher-than-anticipated ear canal volume.
The use of tympanometry can be limited by patient age and cooperation with testing, cerumen impaction, and the skill of the individual performing the testing. When performed by experts, tympanometry and pneumatic otoscopy have equivalent sensitivity (approximately 90%) and specificity (70–80%). Tympanometry is neither more accurate nor more convenient than is properly performed pneumatic otoscopy. Some tympanometers do not perform well in infants younger than 6 months of age. Tympanometry is advantageous if the clinician is unsure of the otoscopic findings. Tympanometry can only indicate presence of middle ear effusion but cannot distinguish between AOM and OME.
Acoustic reflectometers are used to detect middle ear effusion. The device directs sonar-like sound waves of varying frequency toward the tympanic membrane and measures the intensity of reflected sound. This hand-held instrument is similar in size to an otoscope. The tip of the reflectometer is inserted into the ear canal. In contrast to tympanometry, an airtight seal is not required. The frequency of maximal reflected sound depends on the distance of the probe from the eardrum. Middle ear effusion is detected not by the frequency but by the magnitude of maximal reflected sound. When middle ear effusion is present, reflectance is increased in comparison with that in the air-filled middle ear.
Improvements in technology have been made such that reflectometry includes spectral gradient analysis. Reflectometry is easily learned, quick, convenient, and useful in a crying child. It has a lower sensitivity and specificity than properly performed pneumatic otoscopy in detecting middle ear effusion. Because the accuracy of current models decreases in infants younger than 1 year, this technique should not be used in infants younger than 6 months of age. Like tympanometry, reflectometry can reveal only whether middle ear effusion is present and cannot reveal whether the effusion is secondary to AOM or OME. Reflectometry is useful if otoscopic findings are indeterminate.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here