Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Dysuria is defined as painful urination and can be related to uncomfortable contraction of the muscles of the bladder or when urine comes into contact with the inflamed genitourinary mucosa. The differential diagnoses for a patient presenting with dysuria are extensive ( Table 21.1 ) and can be due to infectious or noninfectious causes. The cause of dysuria varies based on age of the child or adolescent; therefore, specific elements of the patient history, potential causes, and diagnostic evaluation will vary with age ( Fig. 21.1 ). With every patient, the provider must elicit a history of signs and symptoms outside the genitourinary tract, including fever, weight loss, generalized rash, involvement of other mucosa, and joint pain or swelling. Physical examination for every patient should include temperature, blood pressure, inspection of the genitals for skin lesions or discharge, abdominal palpation, pelvic examination when indicated, and neurologic examination in children with voiding dysfunction to exclude spinal cord pathology. It is important to also consider less common etiologies of dysuria such as genetic disorders including hyperoxaluria and acute intermittent porphyria.
| Infectious causes | Urinary tract infection (cystitis, pyelonephritis) Urethritis Herpes simplex virus infections Varicella infections Epstein-Barr virus infections Hemorrhagic cystitis (adenovirus) Prostatitis Vaginitis ∗ Renal tuberculosis Urinary schistosomiasis Sexually transmitted infections |
| Urinary tract abnormalities (congenital and acquired) | Urinary calculi Urethral stricture Meatal stenosis Prostate enlargement Malignancy Urethral diverticulum Bladder diverticulum Idiopathic hypercalciuria Bladder outlet obstruction Urethral prolapse |
| Genital tract abnormalities | Sexually transmitted infections Vaginitis Prostatitis Endometritis Endometriosis Labial adhesions Phimosis Paraphimosis Balanitis Foreign body Vulva, vaginal ulcerations |
| Medications and irritants | Primary irritant dermatitis Chemical irritants (soaps, detergents, bubble baths, feminine hygiene products, spermicides) NSAIDs Anticholinergics (amitriptyline, imipramine, and antihistamines) Anti-infectives (isoniazid, sulfonamides) Chemotherapy-related hemorrhagic cystitis (cyclophosphamide) |
| Other | Trauma Stevens-Johnson syndrome/toxic epidermal necrolysis Behçet syndrome Inflammatory bowel disease Toxic shock syndrome Reactive arthritis (in conjunction with urethritis, conjunctivitis) Neurologic conditions that impact bladder emptying Pinworms Lichen sclerosus Appendicitis (if inflamed appendix or periappendiceal abscess lies low in iliac fossa) Tumor (bladder, kidney, uterus, vagina) Foreign body (urethral, vaginal) Perianal group A streptococcus |
∗ Vaginitis; chemical, nonspecific bacterial, Candida albicans , Trichomonas vaginalis , herpes simplex, gonorrhea, group A streptococcus, gram-negative organisms.
Neonates and infants cannot complain of dysuria; however, urinary tract infections (UTIs) are prevalent in this age group and a major source of morbidity. In this age group, it is difficult to distinguish between upper UTI (pyelonephritis) and lower UTI (cystitis) based on signs and symptoms alone. Unlike UTIs in older children, neonatal UTIs are more common in male neonates compared to females. In neonates, UTIs are associated with bacteremia and/or congenital abnormalities of the kidney and urinary tract. In term infants, infections tend to be community acquired and present in the 2nd to 3rd week after birth. UTIs can be caused by either hematogenous spread or an ascending infection. In preterm infants, infections are more likely to be hospital acquired.
The symptoms suggestive of a UTI in the neonate are the same as those for suspected sepsis ; therefore, major presenting symptoms include fever, poor feeding, weight loss, lethargy, and vomiting (see Chapter 52 ). Neonates may also present with jaundice or abdominal distention. A maternal urinary infection at or near term may increase the risk for neonatal pyelonephritis. A mother whose vaginal culture is positive for group B streptococci or who presents with fever, prolonged rupture of the amniotic membranes (>18 hours), uterine tenderness, or preterm labor is at an increased risk for delivering a premature baby with pyelonephritis as part of the neonatal sepsis syndrome. Family history is also important. There is a high genetic component to the presence of vesicoureteral reflux (VUR) ; the siblings of children with known VUR also have a significant risk of reflux, with or without infection. Children with a UTI and VUR are at increased risk of pyelonephritis and renal scarring. However, the screening for VUR in an asymptomatic sibling of an index case of VUR is controversial; a voiding cystourethrogram (VCUG) is recommended if there is evidence of renal scarring on ultrasound or if there is a history of UTI in the sibling who has not been tested. Given that the value of identifying and treating VUR is unproven in the absence of a UTI, an observational approach without screening for VUR may be taken for siblings of children with VUR, with prompt treatment of any acute UTI and subsequent evaluation for VUR.
Physical examination of a neonate suspected of having a UTI should include the palpation of the abdomen to identify hydronephrosis, obstructive lesions, or cystic kidneys. Urine culture should be obtained by suprapubic or bladder catheterization, as bag collection has a high rate of contamination with perineal flora. Because of the associated risk of bacteremia, blood cultures and cerebrospinal fluid (CSF) cultures should be obtained in all neonates in whom UTI is suspected. Initial empirical therapy should be started after collection of urine, blood, and CSF cultures. The empirical therapy should provide broad coverage against probable uropathogens and is initially administered parenterally, as the risk of urosepsis is higher in neonates than in other age groups. Common empirical therapy includes ampicillin in addition to either gentamicin or a third-generation cephalosporin. Therapy is then tailored according to the specific uropathogen identified on culture and the antimicrobial sensitivity.
Ultrasound is the first-line imaging method in neonates after the first UTI. The main purpose of diagnostic imaging is the detection of risk factors, such as anomalies of the kidney and urinary tract or VUR, as well as any renal damage acquired from the infection. Clinical practice guidelines do not recommend DMSA (dimercaptosuccinic acid) scans as part of routine evaluation of infants with their first febrile UTI because the findings rarely affect acute clinical management.
Like neonates, young children 2–24 months of age cannot report dysuria. Nonetheless, UTIs are common (see Chapter 52 ). The main risk factor for febrile infant males is whether or not they are circumcised; other individual risk factors for UTI in males include temperature >39°C, fever for at least 24 hours, and absence of another source of infection. Individual risk factors for UTI in infant females include age younger than 12 months, temperature of at least 39°C, fever for at least 2 days, and absence of another source of infection ( Table 21.2 ).
| Past History |
|
|
|
|
|
|
|
|
| Current Illness |
|
|
|
|
|
|
|
|
|
The method of collecting urine for testing is dependent on the risk factors of the child. Culture of a urine specimen from a bag attached to the perineal area has a high false-positive rate; this method of urine collection is not suitable for diagnosing UTI. However, a culture of a urine specimen from a sterile bag that shows no growth is strong evidence that UTI is absent; if growth of a single uropathogen is present, it may represent a UTI. Nonetheless, one approach provides several recommendations in testing and treatment of UTIs in febrile infants ( Fig. 21.2 ):
If a febrile infant (2–24 months) with no apparent source for fever requires antibacterial therapy, a urine specimen should be obtained via suprapubic aspiration or catheterization for both culture and UA prior to the initiation of antibacterials.
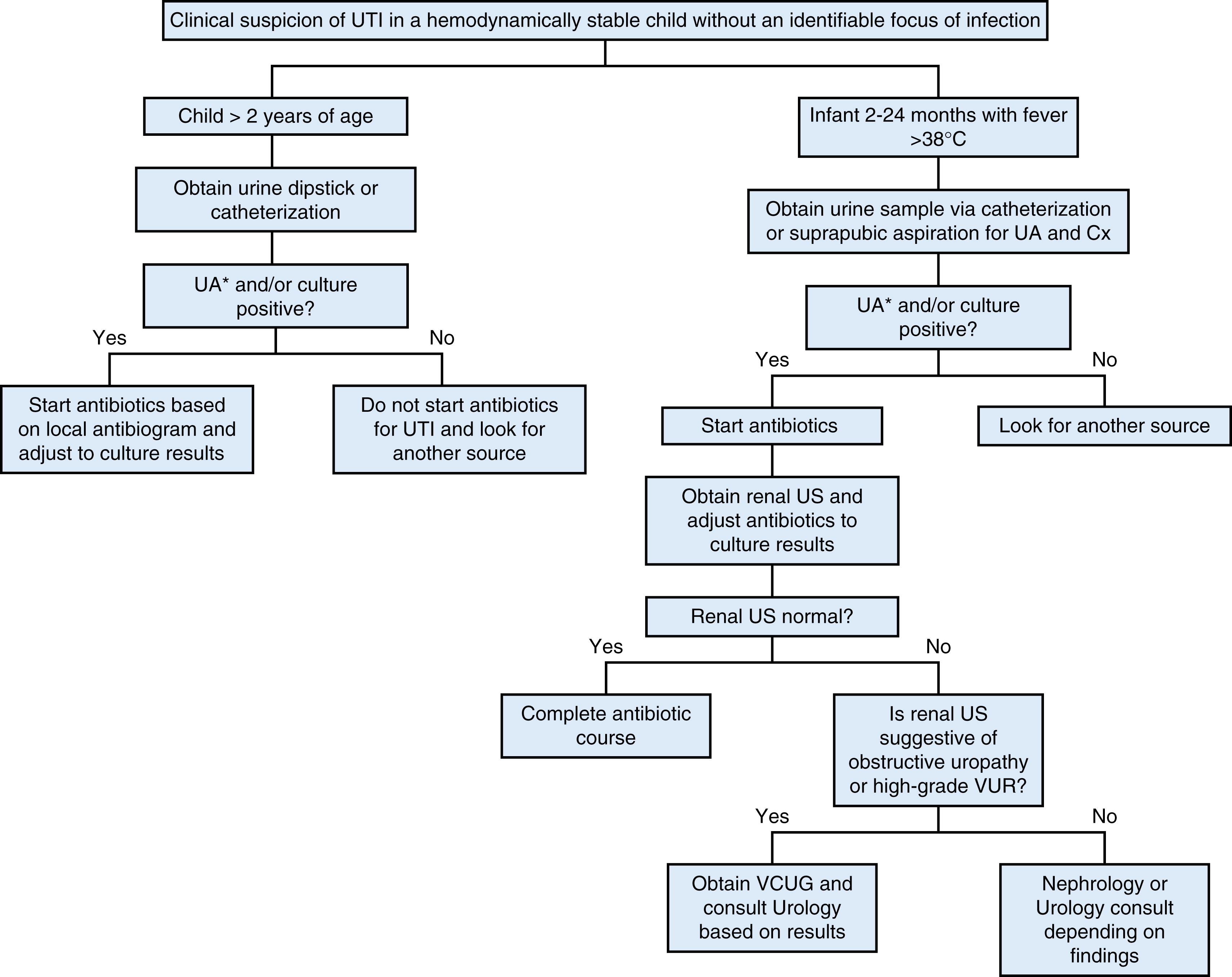
If immediate empiric antibiotic therapy is not indicated:
Clinician should obtain urine sample for UA and culture through catheterization or suprapubic aspiration.
or
Clinician can obtain a clean-void bagged urine sample. If UA results suggest UTI, then an additional urine specimen for culture should be obtained via catheterization or suprapubic aspiration and empiric treatment initiated.
Diagnosing a UTI in young children generally requires both a positive UA (for white cells and/or bacteria) and >50,000 CFU/mL of a single urinary pathogen on urine culture from a suprapubic or catheterized urine specimen. A combination of a positive urine nitrite test plus positive leukocyte esterase plus white blood cells ≥10/mm 3 or ≥5 per high-power field is highly suggestive of a UTI. Some labs also report the microscopic presence of bacteria. Nitrite testing may be negative with high urine flow rates and frequent bladder emptying (bacteria need ∼4 hours to produce nitrites); leukocyte esterase may be negative with certain bacteria or localized infections (abscess). Negative leukocytes, nitrites, and leukocyte esterase in the presence of bacteria suggest asymptomatic bacteriuria, which requires no treatment.
Sterile pyuria (leukocytes with no bacterial growth) may be seen in a partially treated UTI, renal or perinephric abscess, infection proximal to an obstruction (duplication), nephronia, interstitial nephritis, renal tuberculosis, Kawasaki disease, MIS-C (multisystem inflammatory syndrome in children), adenovirus or JC viruses, endocarditis, sexually transmitted infections (STIs), schistosomiasis, prostatitis, appendicitis, epididymitis, or lupus.
The usual choices for empirical antibacterial therapy include a third-generation cephalosporin, amoxicillin plus clavulanic acid, or trimethoprim-sulfamethoxazole. The clinician should base choice of antibacterial on local antimicrobial sensitivity patterns if available and should adjust according to sensitivity results of the isolated uropathogen. Most well-appearing infants can be treated orally. Fever persisting after 48 hours of appropriate antibiotic therapy raises the suspicion of a complicated UTI (obstructive uropathy, abscess, nephronia).
The rationale for imaging infants with UTI is to identify abnormalities of the genitourinary tract. Renal and bladder ultrasound is the first-line imaging modality to identify anatomic abnormalities. VCUG to detect VUR should not be performed after the first febrile UTI. It is indicated if the ultrasound reveals hydronephrosis, renal scarring, or other findings that suggest high-grade VUR or obstructive uropathy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here