Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Patients with long-standing inflammatory bowel disease (IBD) are at an increased risk for development of colorectal cancer (CRC). Risk factors for the development of CRC in ulcerative colitis (UC) or Crohn's colitis include young age of disease onset, longer duration of disease, greater extent of colonic involvement, coexistent primary sclerosing cholangitis (PSC), active endoscopic or histological inflammation, family history of CRC in a first-degree relative diagnosed before 50 years of age, a history of dysplasia, stricturing disease in UC, inflammatory (“pseudo”) polyps, a shortened tubular colon, and possibly male gender.
Of all the risk factors associated with the development of CRC in IBD, colitis-related dysplasia appears to confer the greatest risk, leading gastrointestinal (GI) societies to advocate colonoscopic surveillance to detect dysplasia in high-risk patients. The goal of endoscopic surveillance is to reduce mortality and morbidity of CRC by either detecting and resecting dysplasia or detecting CRC at an earlier and potentially curable stage. Surveillance strategies, until recently, relied on examination of the mucosa with targeted biopsies of visible lesions and random biopsy sampling, based on the prevailing notion that dysplasia is frequently not associated with visible mucosal abnormalities. Meanwhile, advances in optical technology allowing for greater endoscopic identification of dysplasia and consensus that most dysplasia in patients with IBD is visible have led to a paradigm shift in our approach to surveillance and management of dysplasia. This chapter will review the epidemiology of CRC in IBD, the evolution in our understanding of dysplasia, outline the most recent surveillance guidelines from scientific societies, and discuss the management of dysplasia and controversies therein.
Colorectal cancer (CRC) in IBD, accounting for 1% to 2% of CRC cases in the general population, is responsible for 10% to 15% of all deaths in IBD patients. Indeed, after genetic causes of CRC (such as familial adenomatous polyposis and Lynch syndrome), IBD ranks as the third highest risk factor for CRC, underpinning the need to better define associated risk factors and optimize surveillance strategies, thereby achieving meaningful reduction in IBD-CRC associated morbidity and mortality.
The risk of CRC in IBD (and UC in particular) increases with time but risk estimates have been difficult to quantify, often limited by heterogeneity and methodology in the retrospective cohorts studied. A large meta-analysis in 2001 estimated a cumulative CRC risk of 2% at 10 years, 8% at 20 years and 18% after 30 years of colitis. A 2012 population-based study from Copenhagen County, Denmark, demonstrated a decreasing incidence of CRC in IBD patients over the last few decades. More recently (2015), a 40-year colonoscopic surveillance program from St. Mark's Hospital, UK, reported a cumulative incidence of developing CRC in IBD patients at 0.1% in the first decade since UC symptom onset, followed by 2.9%, 6.7%, and 10% by the second, third, and fourth decade, respectively. The authors reported a significant decrease in the incidence of colectomy for dysplasia and a reduction in the incidence rate of advanced CRC and interval cancers over 4 decades of surveillance. Population-based meta-analyses have shown an overall CRC incidence ratio of 1.7 in all IBD patients, with patients with CD reported to have a 1.9-fold and patients with UC having a 2.4-fold increase in lifetime CRC risk compared to the general population. Thus, recent studies suggest a decrease in the risk of CRC in IBD, a temporal reduction that may be explained by more aggressive control of inflammation through medication, the greater uptake of surveillance colonoscopy allowing detection and resection of dysplastic lesions before the development of CRC, and appropriate timing of colectomy.
Several risk factors are associated with the development of CRC in UC or Crohn's colitis as stated previously and include young age of disease onset, longer duration of disease, greater extent of colonic involvement, coexistent PSC, active endoscopic or histological inflammation, family history of CRC in a first-degree relative diagnosed before 50 years of age, a history of dysplasia, stricturing disease in UC, inflammatory (“pseudo”) polyps, a shortened tubular colon, and male gender ( Fig. 39.1 ). Subtotal colitis or pancolitis confers the highest risk of developing CRC and patients with colonic CD disease involving more than one-third of the colon are also at increased risk of CRC. The extent of colonic involvement should be based on both endoscopic and histological criteria and on whichever reveals more extensive disease. Although patients with proctitis or distal proctosigmoiditis alone are not at increased risk compared with the general population, many patients with proctitis will develop more proximal disease over the course of their lifetime and a screening colonoscopy is recommended 8 years after the onset of symptoms even in patients with previously isolated proctitis to confirm extent of disease. The relative risk (RR) of CRC rises with longer disease duration and is the rationale behind initiation of surveillance colonoscopy after 8 to 10 years of disease. PSC confers a high risk for CRC. A meta-analysis of 11 trials reported a 4-fold increased risk of developing colonic neoplasia in patients with PSC and UC compared to those with UC alone. Additionally, several clinical trials have demonstrated a persistently elevated risk of CRC in PSC despite undergoing orthotopic liver transplantation. Thus, patients with IBD and PSC should undergo surveillance colonoscopy annually beginning at the time PSC is diagnosed. Studies examining a link between early age of onset of IBD and CRC are conflicting and the American Gastroenterological Association (AGA) recommends that surveillance be based on duration of illness and not chronological age.

The known risk factors for CRC in IBD are almost all nonmodifiable with the possible exception of inflammation. A positive association between the degree of microscopic inflammation and advanced neoplasia has been noted in several studies. Colonic strictures in UC (but not in CD), a shortened tubular colon, and multiple pseudopolyps also increase CRC risk, with the latter significantly limiting the ability to adequately survey the colon. These clinically important associations must be considered when counselling patients about their risk of developing CRC and planning surveillance examinations.
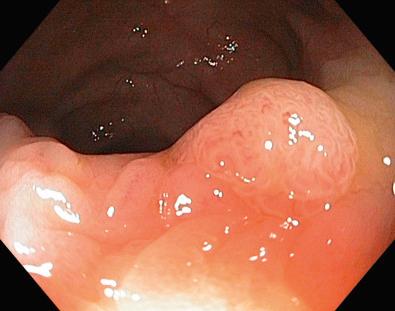
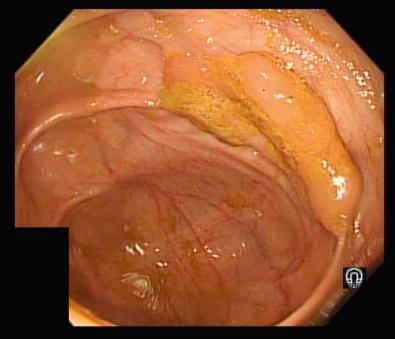
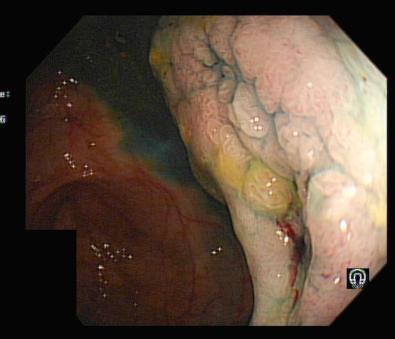
The detection of dysplasia is currently the best marker of CRC risk in IBD patients, the prevention of which is the ultimate goal of surveillance colonoscopy. Biopsies taken at surveillance colonoscopy should be graded as “positive” for dysplasia, “negative” for dysplasia, or “indefinite” for dysplasia and further classified as low-grade dysplasia (LGD), high-grade dysplasia (HGD), or carcinoma. Considerable interobserver variability exists amongst pathologists around interpretation of “low-grade” dysplasia and “indefinite for dysplasia” categories, mandating a second opinion from a specialist GI pathologist to confirm dysplasia when detected. Older guidelines recommended that lesions be characterized as sporadic adenomas if found outside an area of known colitis or as dysplasia–associated lesion or mass (DALM) if detected within an area of colitis; however, this terminology has been abandoned and should no longer be used. The terms “visible” and “invisible” should be used instead to describe dysplasia within clearly identified lesions or within random biopsy samples, respectively, with the addition of terms for ulceration and border of the lesion. Visible dysplasia is further classified as polypoid (pedunculated or sessile) or nonpolypoid (superficial elevated, flat or depressed) in accordance with the Paris Classification ( Figs. 39.2 and 39.3 ). Accordingly, the term endoscopically resectable indicates that distinct margins of the lesion can be identified, the lesion appears completely excised on visual inspection after endoscopic resection, histological assessment of the resected specimen is consistent with complete removal, and that biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histological assessment ( Fig. 39.4 ).

Recognition that most dysplasia is endoscopically visible, bolstered by advanced imaging techniques facilitating dysplasia detection, has had a significant impact on modern dysplasia management and surveillance strategies.
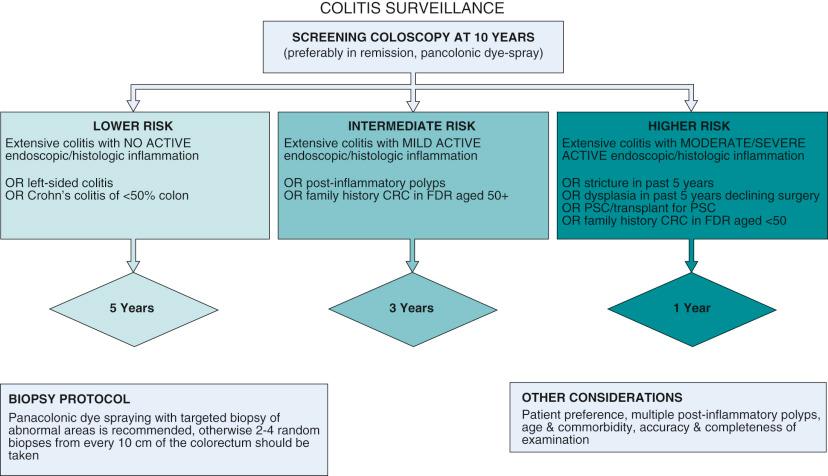
The aim of endoscopic surveillance is the reduction of mortality and morbidity from CRC through detection and resection of dysplasia or by detecting CRC at earlier and potentially curable stages. Endoscopic surveillance has been shown to reduce the risk of death from CRC in the IBD population and also to be cost-effective in various case-series, case-control studies and population-based cohort studies. Thus, despite the lack of randomized controlled trials, the invasive nature of assessment, and utilization of societal resources, surveillance colonoscopy in IBD patients has been endorsed by multiple societies. Most societies recommend that all patients with UC (including isolated proctitis) and Crohn's colitis should be offered screening colonoscopy approximately 8 to 10 years after onset of clinical symptoms to restage disease extent and evaluate features that may confer a higher risk for IBD–CRC. In the absence of evidence from prospective studies, societies vary in their recommendations with surveillance intervals after a screening colonoscopy but universally agree and recommend annual screening for patients with the highest risk of IBD associated CRC. Thus, patients with concomitant PSC, extensive colitis with active endoscopic or histological inflammation, a family history of CRC in a first-degree relative under the age of 50, a personal history of dysplasia, and stricturing disease (in UC patients) should be offered annual surveillance. Normal appearing mucosa appears to be associated with a lower risk of IBD associated colorectal neoplasia. The British Society for Gastroenterology (BSG), European Crohn's and Colitis Organization (ECCO), National Institute for Health and Clinical Excellence (NICE), and Cancer Council of Australia (CCA) support a risk-stratification approach, increasing surveillance intervals to 5 years in lowest risk patients. Societies in the United States do not currently recommend lengthening the surveillance interval to beyond 3 years. Recommendations from the AGA guidelines are outlined in Box 39.1 . The BSG guidelines incorporating risk factors and newer imaging techniques are outlined in Fig. 39.5 .
All patients, regardless of the extent of disease at initial diagnosis, should undergo a screening colonoscopy a maximum of 8 years after onset of symptoms, with multiple biopsy specimens obtained throughout the entire colon, to assess the true microscopic extent of inflammation.
Patients with ulcerative proctitis or ulcerative proctosigmoiditis are not considered at increased risk for IBD-related CRC and thus may be managed on the basis of average-risk recommendations.
Patients with extensive or left-sided colitis should begin surveillance within 1 to 2 years after the initial screening endoscopy.
Patients with PSC should begin surveillance colonoscopy at the time of PSC diagnosis and then yearly.
Patients with a history of CRC in a first-degree relative, ongoing active endoscopic or histologic inflammation, or anatomic abnormalities (shortened colon, multiple pseudopolyps, or stricture) may benefit from more frequent surveillance colonoscopy.
Representative biopsy specimens from each anatomic section of the colon is recommended. Though no prospective trials have determined the optimal number of biopsies to take, one study has recommended a minimum of 33 biopsy specimens.
Surveillance colonoscopy should ideally be performed when the patient is in remission.
These recommendations apply to patients with Crohn's colitis who have disease involving at least one-third of their colon.
AGA, American Gastroenterological Association; CRC, colorectal cancer; IBD, inflammatory bowel disease; PSC, primary sclerosing cholangitis.
The success of surveillance depends on several factors, of which the ability to detect dysplasia is probably most crucial. Surveillance traditionally performed by taking random colonic biopsies was based on the premise that dysplasia is frequently not associated with mucosal abnormalities. To detect dysplasia with 90% probability, 33 serial colonic biopsies from four quadrant biopsy specimens need to be obtained every 10 cm from each anatomical segment of the colon, a practice endorsed by many GI societies.
Evolution in endoscopic technology from standard definition (SD) colonoscopy using video chips to high-definition (HD) colonoscopy, and indeed evidence that most dysplasia is visible at standard white light colonoscopy, has challenged the practice of random biopsy sampling as the basis of surveillance assessment.
The practice of random biopsies would sample less than 1% of total colonic mucosa, and one study suggested that up to 1266 random biopsies would be needed to detect one additional episode of dysplasia. In a study in which UC patients underwent colonoscopy every 2 years, interval cancers were observed to develop between 10 and 28 months after dysplasia-free examination, reflecting poorly on the practice of random biopsies alone for dysplasia detection at surveillance.
Surveillance strategies must take additional aspects such as resectability of dysplasia, anatomical features such as pseudopolyps, and a shortened tubular colon into consideration; these may pose difficulties with dysplasia detection. Furthermore, colonic inflammation can make pathologic discrimination of dysplasia difficult; thus surveillance should ideally take place when the patient is in clinical remission. These factors merit careful consideration with patients when committing to a surveillance program. Evidence suggests that patients do not wish to consider colectomy until there is a relatively high certainty of cancer underpinning the importance of careful consideration and meticulous assessment, employing best available technology and technique to detect and resect dysplasia to avoid IBD-associated CRC and colectomy.
New imaging techniques such as chromoendoscopy (CE), narrow band imaging (NBI), and confocal endomicroscopy have been developed as an adjunctive technique to detect more subtle mucosal abnormalities. Several studies have demonstrated a superior diagnostic yield and therapeutic advantage with CE when compared with standard random biopsy and white light technique for index screening of dysplasia in colitis, supported by meta-analyses providing evidence that the use of CE with targeted biopsies is 8.9 times more likely to detect any dysplasia and 5.2 times more likely to detect nonpolypoid dysplasia than white light endoscopy (WLE) with random biopsy. This evolution in knowledge has seen cautious translation in societal recommendations over the years. Although the American College of Gastroenterology's (ACG) 2010 guidelines considered it premature to endorse CE in low-risk patients, the Crohn's and Colitis Foundation of America's (CCFA) 2004 and AGA's 2010 guidelines considered CE with targeted biopsies as a reasonable alternative to WLE for endoscopists experienced in this technique. CE with targeted biopsies is endorsed by all recent European guidelines (ECCO, BSG, NICE) and recent American Society for Gastrointestinal Endoscopy (ASGE) guidance. The recently published Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus Recommendations (SCENIC) recommends CE over standard white light colonoscopy and suggest CE over HD colonoscopy for dysplasia surveillance in IBD, with meta-analysis demonstrating a significantly greater proportion of dysplasia detection at CE (RR 1.8, absolute risk increase 6%) than white light colonoscopy alone. Furthermore, this strategy has also been shown to be cost-effective, especially with increasing surveillance intervals based on the risk of CRC.
CE involves the use of topical contrast agents, either 0.1% methylene blue or 0.03% to 0.5% indigo carmine. Excellent bowel preparation is a prerequisite. Colonic mucosa is sprayed segmentally with contrast agent after cecal intubation and upon withdrawal, using a spray catheter or through the forward water-jet channel using an automated pump. CE enhances mucosal irregularities and helps delineate the lesion morphology, size, and border to evaluate for endoscopic features of submucosal invasion ( Figs. 39.6 and 39.7 ; and ). Thus, endoscopically resectable lesions may be resected if feasible, or tattooed and referred to an endoscopist with expertise in endoscopic mucosal resection or dissection as appropriate. Targeted biopsies should be taken from lesions deemed endoscopically unresectable and lesions of uncertain significance. Furthermore, at least two histological staging biopsies from several colonic segments are recommended to determine histological extent and severity of disease, which, in turn, affects the risk of dysplasia. Random biopsies are not recommended if CE is used for dysplasia surveillance. Despite heightened sensitivity of CE in detecting dysplastic foci and other purported benefits, its universal adoption and acceptance has been met with by some scepticism. The natural history of additional, smaller, flatter lesions identified at CE is poorly understood. The rate of progression from indefinite and LGD to cancer appears to be low in some high-risk cohorts, even when considering variables such as PSC and previous advanced dysplasia. Moreover, data from the Surveillance, Epidemiology and End results Medicare-linked database of patients over 67 years old showed that interval cancers 6 to 36 months after colonoscopy occurred in a much higher proportion of patients with IBD (15.1% with Crohn's disease and 15.8% with ulcerative colitis) than patients without IBD (5.8%), suggesting that clinically relevant areas of neoplasia may be missed with current colonoscopy surveillance. Considering this, the SCENIC consensus acknowledges that its recommendation for CE over HD white light colonoscopy is conditional, being based on small observational studies.

Since the publication of the SCENIC consensus paper in 2015, several studies have added to the body of evidence supporting CE as the preferred technique, with others expressing reservations regarding its universal adoption, through demonstration of its limitations and identifying gaps in our knowledge and understanding of the natural history of dysplasia. Marion et al (2016) reported a follow-up evaluation of their 2008 study of patients in an IBD surveillance program. Sixty-eight patients (from the original cohort of 115), with median disease duration of 21 years, were followed over a 5-year period, between 2005 and 2011. All patients underwent colonoscopy surveillance with random biopsy specimens, targeted WLE, and dye-spray CE. After a mean of three surveillance colonoscopies per patient, six dysplastic lesions were detected by random biopsy technique, as compared with 11 and 27 dysplastic lesions seen at WLE and CE respectively. CE demonstrated superiority to random biopsy specimens (odds ratio [OR] 5.4; 95% confidence interval [CI], 2.9–9.9) and targeted WLE (OR 2.4; 95% CI, 1.4–4.0). A negative result from CE assessment was the best indicator for a dysplasia-free outcome and a positive result was associated with earlier referral for colectomy (hazard ratio [HR] 12.1; 95% CI, 3.2–46.2). Notably, of the 10 patients with dysplasia referred for colectomy, no carcinomas were found.
Gasia et al (2016), studied a cohort of 454 IBD patients undergoing surveillance assessments between 2011 and 2014. Patients were examined using WLE, HD colonoscopy, virtual electronic, or dye spray CE. Just under one-third of patients underwent WLE or HD colonoscopy with random biopsy, and 14% had virtual CE with random biopsies. A smaller number of patients underwent dye-spray CE with random (n = 4) or targeted (n = 24) biopsies. Targeted biopsies identified more neoplastic lesions than random biopsies (19% vs. 8%). Four dysplastic lesions were seen at HD WLE. The investigators found no difference in yield between dye CE, virtual CE, and targeted WLE in the cohort of 454 patients studied. No dysplasia was identified, however, from random biopsy samples alone. The futility of random biopsy has been demonstrated repeatedly and convincingly in several prospective studies.
In a large Dutch multicenter study, Mooiweer et al (2015) studied the outcomes of adoption of CE from 440 colonoscopies in 401 patients compared with historical outcomes of 1802 colonoscopies in 772 patients with WLE. No difference in dysplasia detection was noted in both groups (11% vs. 10%). An inherent limitation of the retrospective study was the lack of data for examination factors (including bowel prep and withdrawal time), but the remarkably stable neoplasia detection over a 10-year period in highly experienced hands suggests that CE is not superior to WLE.
In contrast, another study from St. Mark's Hospital, London, reporting a 40-year experience with colonoscopic surveillance, found a recent increase in the incidence rate of dysplasia since the adoption of high-definition white light endoscopy (HD WLE) and CE for surveillance, but no decrease in the rate of colon cancer. Although CE seemingly did not affect the outcome of CRC in IBD, there was a significant increase in the proportion of early-stage (Duke's A and B) versus late-stage (Duke's C & D) CRC in the most recent decade. HD WLE and CE were introduced at St. Mark's in 2006 and although patients were not randomized to CE between 2006 and 2012, the CRC incidence rate was 2.2/1,000 patient-years in patients receiving at least one CE versus 4.6 in those who had never received CE ( p = 0.02). Deepak et al (2016) from the Mayo Clinic reported an incremental diagnostic yield from CE. In this retrospective study, IBD patients with colorectal dysplasia on WLE, endoscopic, and histologic findings (median disease duration 18 years) were compared among the index WLE, first, and subsequent CE. Of 95 index cases, dysplasia was identified in 55 patients at index WLE. The first CE identified dysplastic lesions in 50 patients (34 new lesions not seen at index WLE), endoscopic resection was performed for 43 lesions, and 14 patients underwent surgery with two cases of CRC and three cases of HGD. From subsequent CE assessments, 34 lesions were identified in 20 patients. The data support CE as a surveillance procedure in high-risk patients. Indeed, one of the arguments against “CE for all surveillance” is that the natural history of dysplastic lesions identified at CE remains unknown. Choi et al (2016) identified four characteristics that were significantly associated with a later diagnosis of HGD or CRC. Nonpolypoid lesion appearance, defined as Paris type 0-II (visible, slightly elevated, or depressed), type 0-III (excavated), or plaque-like, was the strongest factor (HR 8.6; 95% CI 3-24.8), but macroscopically invisible dysplasia (HR, 4.1; 95% CI, 1.3-13.4), lesion size of 1 cm or greater (HR, 3.8; 95% CI, 1.5-13.4), and previous history of indefinite dysplasia (HR, 2.8; 95% CI, 1.2-6.5) were also significant predictors. There was also strong positive correlation between the number of these risk factors present and a subsequent HGD or CRC diagnosis. The strongest risk factor, nonpolypoid dysplasia, was found at significantly greater frequency in those patients who underwent CE rather than white-light colonoscopy (15.8% vs. 7.8%, respectively), although exposure to CE did not lower the risk of HGD or CRC after Bonferroni correction for multiple testing.
Successful delivery of dysplasia surveillance using CE, however, hinges on several factors, including appropriate training and expertise (endoscopist and nurses), lesion recognition, and interobserver variability amongst pathologists identifying and grading dysplasia, as well as operational barriers, such as the availability of dye and equipment and procedural time, which results in some hesitancy amongst gastroenterologists in adopting CE, and referral to “experts” for its provision in some instances. The evidence favors CE for surveillance where suitable expertise is available and is backed by several scientific societies and international consensus opinion. What constitutes “appropriately trained” for CE is currently debatable, as there is no standardized definitions or accreditation process. One study suggested that completion of 16 CE procedures may be adequate for dysplasia detection training using this modality, but this has not since been replicated. A recent multicenter study from Spain has provided “real-world” experience in support of CE for IBD surveillance, challenging skepticism regarding the effectiveness of CE outside of a clinical trial setting and potential limitations posed by less experience with CE. In a prospective study performed between 2012 and 2014, 350 patients with IBD on dysplasia surveillance were systematically evaluated using WLE (SD in 41.5% and HD in 58.5%) for each colonic segment, followed by CE with 0.4% indigo carmine. An incremental yield of 57.4% was noted with CE, comparable between SD and HD colonoscopy (51.5% vs. 52.3%; p = 0.30). A further interesting observation was a comparable dysplasia detection between expert and nonexpert colonoscopists (18.5% vs. 13.1%; p = 0.20) and no significant learning curve. Endoscopic findings predictive of dysplasia were proximal colonic lesions, protruding morphology, loss of innominate lines, and a neoplastic Kudo pit pattern. Arguable limitations of the study include the potential for a “Hawthorne effect” (diligence with performance of colonoscopy in a prospective study) and an incremental yield from a “second look;” as there was also a small sample size, this study does provide proof of principle for the wider and realistic adoption of CE for dysplasia surveillance in high risk IBD patients and potentially in “nonexpert” hands. Several excellent resources, however, are available for colonoscopists to enhance their skills. Meanwhile, evolution in our knowledge of the natural history of dysplasia and the clinical implications of dysplasia found by CE through its wider adoption may close many gaps in our understanding of its real place in surveillance. Until then, the bulk of the evidence favors CE with targeted biopsy in individuals at high risk or those with previous dysplasia. In the remaining majority of patients undergoing surveillance colonoscopy, careful assessment with either HD WLE and random biopsies or CE with dye spray may be appropriate with no compelling mandate for one over the other at the present time. A summary of recommendations from the SCENIC consensus for surveillance and management of dysplasia in patients with IBD is outlined in Box 39.2 .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here