Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Early onset (<24 hours of age) or new jaundice is never normal and should be investigated.
Initial evaluation of a jaundiced infant should always include conjugated and unconjugated bilirubin levels.
Infants presenting with jaundice secondary to conjugated hyperbilirubinemia should undergo expedient evaluation for potentially life-threatening and treatable causes of cholestasis and then for other causes.
The liver is the largest abdominal organ and serves as the body’s main location of energy production, metabolism, protein synthesis, and detoxification. Embryologically, the liver is derived from an endodermal outgrowth from the foregut into the septum transversum. There are multiple cell types within the liver parenchyma, including hepatocytes, cholangiocytes, stellate cells, endothelial cells, and cells of the innate immune system. The key roles of the hepatocyte include protein synthesis, fatty acid synthesis and oxidation, formation of lipids, cholesterol and bile salts, bilirubin metabolism, gluconeogenesis, glycogen synthesis, urea cycle and production of ammonia, and detoxification. The hepatocyte is the only cell in the body that manufactures albumin, fibrinogen, and prothrombin clotting factors. In the setting of significant liver injury, loss of normal hepatocyte synthetic function often results in the development of coagulopathy and hypoalbuminemia.
Bile is primarily composed of bile acids, bilirubin, cholesterol, and phospholipids, which are manufactured in the hepatocyte, secreted into the canaliculus, transported into the biliary ducts, and, ultimately, secreted into the intestine or stored within the gallbladder. Bile is critical for solubilizing dietary fats and fat-soluble vitamins (A, D, E, and K) to make them available for absorption. Disruption of this process at any level results in cholestasis. Cholestasis refers to obstruction of the normal excretion of bile from the liver resulting in the abnormal accumulation of bile components within the liver and serum. While cholestasis is not synonymous with jaundice from conjugated hyperbilirubinemia, serum conjugated bilirubin level is the most clinically useful marker of cholestasis.
Like the lungs, the liver is unique in that it has a dual blood supply: nutrient-rich venous blood from the portal vein, and oxygen-rich arterial blood from the hepatic artery. Venous drainage of the liver occurs through the hepatic veins. In the fetus, the umbilical vein delivers oxygenated blood to the liver via the left portal vein and the ductus venosus, which then joins the left hepatic vein as it drains into the inferior vena cava. The ductus venosus closes spontaneously at birth. Congenital anomalies of the portal vein or thrombosis associated with umbilical vein catheter placement may lead to portal vein obstruction and portal hypertension. Portal hypertension describes a pathologic increase in venous pressure in the portal venous system and occurs when the portal pressure rises above 10 mmHg. Portal hypertension may be prehepatic (portal vein), intrahepatic (cirrhosis), or posthepatic (hepatic venous) in etiology. Signs and symptoms of portal hypertension include splenomegaly, ascites, and gastrointestinal bleeding secondary to bleeding varices.
Neonates with liver disease may present with an array of clinical signs ranging from asymptomatic jaundice to acute liver failure. Clinical evaluation and management differ depending on underlying etiology. Clinical signs suggestive of underlying liver disease include ascites, hepatomegaly with or without splenomegaly, coagulopathy, elevated transaminases, hyperammonemia, hypoglycemia, and cholestasis. The initial evaluation of suspected liver disease must include a careful physical examination, laboratory evaluation, and imaging. The initial laboratory evaluation for suspected liver disease includes an assessment of hepatocellular injury and function, including aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyl transpeptidase (GGT), conjugated and unconjugated bilirubin levels, prothrombin time/international normalized ratio (INR), and albumin levels. Elevations in serum ALT and AST indicate hepatocellular injury; however, they are not specific to the liver and may be found in other tissues such as red blood cells and skeletal muscle. An elevation in ALP and GGT may indicate biliary obstruction or inflammation; however, care must be taken in children, as elevated ALP is also indicative of normal bone growth and metabolism. ALP can be particularly elevated in preterm infants with osteopenia of prematurity. As stated previously, an elevation in transaminases (AST, ALT) indicates hepatocyte injury, whereas an elevation in prothrombin time/INR and hypoalbuminemia indicates a loss of normal hepatocyte function and most likely a greater degree of hepatocyte injury. The most appropriate initial imaging modality is abdominal ultrasound (US) with Doppler, which can detect anatomic or vascular anomalies, thrombosis, or suggest underlying portal hypertension.
Liver disease in the neonate frequently presents with new or persistent jaundice. Infants presenting with new jaundice deserve an urgent evaluation, as this is never normal. Term infants with jaundice persisting beyond 14 days and preterm infants with jaundice beyond 21 days of life deserve expedient evaluation. In any jaundiced infant, it is necessary to determine whether jaundice is due to conjugated versus unconjugated hyperbilirubinemia. Although the differential of potential causes will vary by the type of predominant bilirubin, it is prudent to prioritize the evaluation to identify conditions where early intervention is associated with improved outcome.
Elevated unconjugated hyperbilirubinemia is often seen secondary to breast milk jaundice, sepsis, hemolysis secondary to blood group incompatibility (ABO and rhesus) or red blood cell dyscrasia, and, more rarely, Crigler–Najjar syndrome. While physiologic jaundice and breast milk jaundice are common, jaundice secondary to unconjugated hyperbilirubinemia should still be investigated if it is of very early onset (within 24 hours of life), prolonged beyond 14 days, or at high levels. Breast milk jaundice is the most likely etiology of unconjugated hyperbilirubinemia if the serum level is downtrending; there is no evidence of hemolysis, infection, abnormal thyroid function, or elevated serum aminotransferases; and the child is clinically well. However, if unconjugated hyperbilirubinemia persists or is rising, or the child is ill, disorders influencing bilirubin conjugation and hemoglobin metabolism should be investigated.
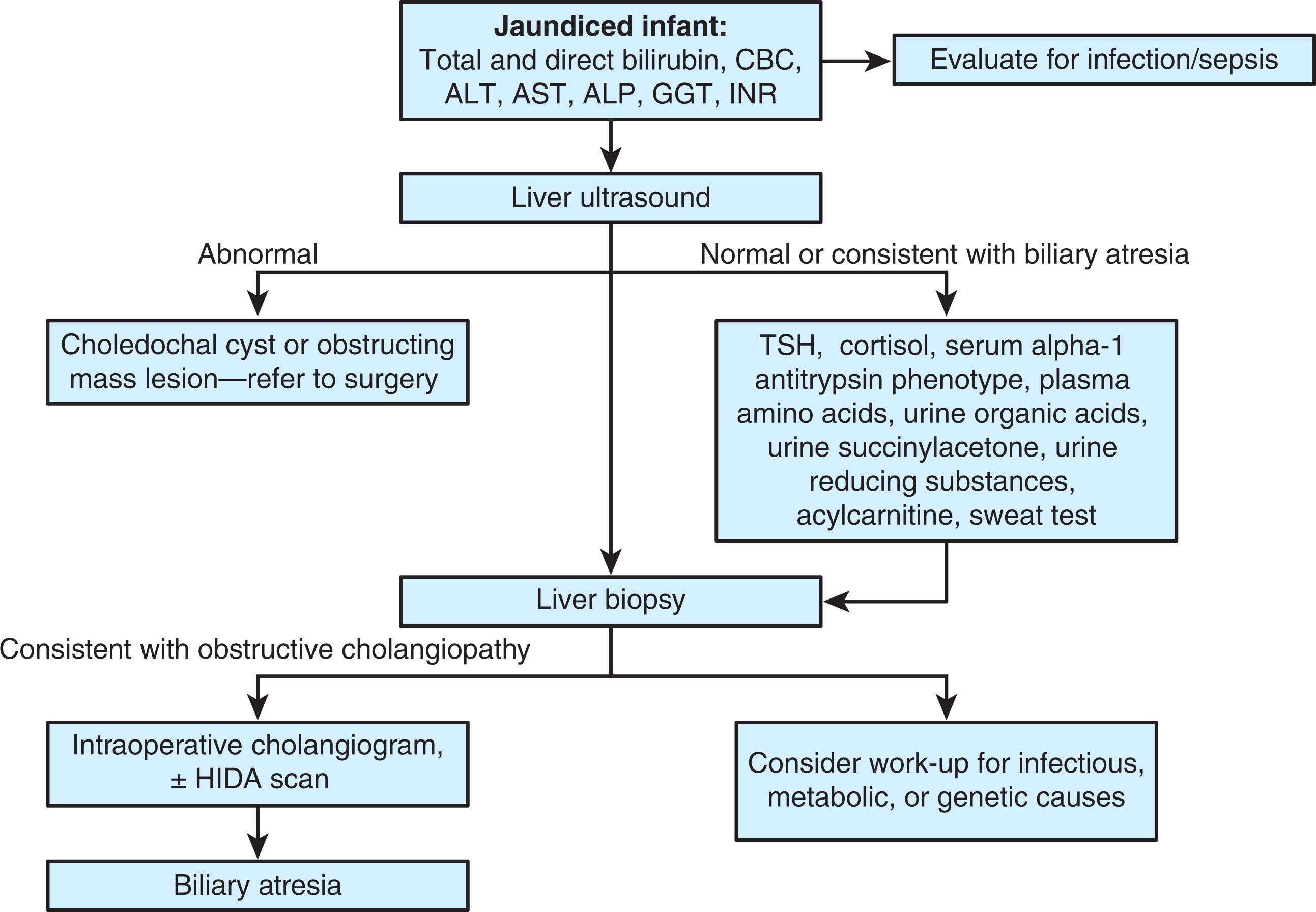
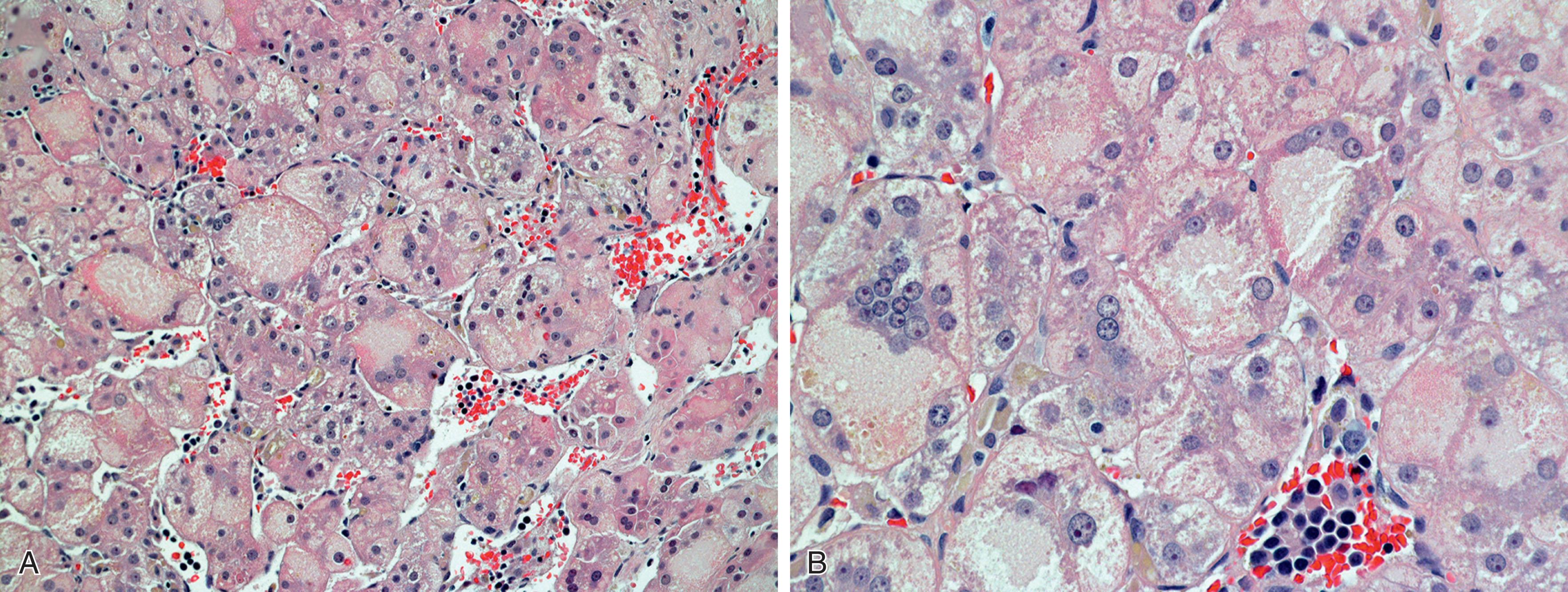
The presence of conjugated hyperbilirubinemia (defined as conjugated bilirubin level ≥15% of the total) should raise concern for underlying liver disease. An initial approach to the evaluation of neonatal conjugated hyperbilirubinemia is shown in Fig. 65.1 . Specific etiologies of neonatal cholestasis are reviewed below and summarized in Table 65.1 . Idiopathic neonatal hepatitis is a term historically applied to infants presenting with neonatal cholestasis or hepatitis in whom no specific etiology can be identified. Liver biopsies in these infants often demonstrate nonspecific intrahepatic cholestasis and giant cell transformation of hepatocytes ( Fig. 65.2 ). Currently, it is recognized that multinucleated giant cells represent a stereotypical response by the immature liver to many etiologies of hepatocellular injury, including infection, biliary obstruction, and metabolic disease. Today, with advancements in next generation DNA sequencing, the number of identifiable etiologies of neonatal cholestasis and hepatitis has increased dramatically, further reducing the frequency and utility of the idiopathic neonatal hepatitis diagnosis.
| Infection |
|
| Endocrine |
|
| Metabolic/Genetic |
|
| Cardiovascular |
|
| Syndromic |
|
| Biliary |
|
| Nutritional |
|
Cholestasis refers to obstruction of the normal excretion of bile from the liver, resulting in abnormal accumulation of bile salts, bilirubin, and lipids in the blood. In infants, cholestasis may present as asymptomatic jaundice, pruritus, unexplained fat-soluble vitamin deficiency, or acute liver failure. The presence of acholic stools suggests functional or anatomic biliary obstruction. The following sections review the most common etiologies of neonatal cholestasis and discuss the corresponding disease-specific evaluation and clinical management.
Nutritional management is critical and central to the care of infants with chronic cholestasis. Growth failure commonly occurs secondary to malabsorption from inadequate bile flow, intestinal congestion from portal hypertension, and increased caloric needs in the setting of chronic liver inflammation. The estimated daily caloric intake for infants with chronic cholestasis may approach 150% of that of healthy infants. In addition, malabsorption of fat-soluble vitamins (A, D, E, and K) can result in progressive coagulopathy and pathologic fractures. While enteral nutrition is preferable, some infants go on to require nutritional optimization with total parenteral nutrition. The general principles of nutritional management in cholestatic infants include assurance of adequate absorbable calories and nutrients, monitoring levels of and supplementation with fat-soluble vitamins, and preparation to escalate the nutritional support and supplementation in infants who cannot sustain adequate intake for growth orally, with supplemental enteral feeds via nasogastric tube, or initiation of parenteral nutrition in situations of failure to grow or gain weight adequately with maximal enteral nutrition. The selection of formula should consider medium-chain triglyceride (MCT) content, as this fat source is directly absorbed into the portal venous system and does not require emulsification by bile acids or active transport that is disrupted in cholestasis. Children with portal hypertension and ascites also benefit from sodium restriction.
Biliary atresia (BA) is an idiopathic hepatobiliary disorder of infancy characterized by inflammation and progressive fibrosis resulting in the obliteration of the extrahepatic biliary ducts within weeks of birth. As the disease progresses, the end result is variable destruction and obliteration of the intrahepatic bile ducts with subsequent biliary cirrhosis. BA is the most common cause of infantile chronic liver disease and the most frequent indication for liver transplantation in the pediatric population. The reported incidence of BA is 0.5 to 3.2 per 10,000 live births but varies based on ethnicity and geography with higher incidence in the Far East and Oceania. Babies with BA generally present between 2 and 5 weeks of age. Without rapid intervention the natural history of BA is uniform fatality by 2 years of age.
Biliary atresia generally presents in one of two broad clinical phenotypes: sporadic/nonsyndromic, which is the more common form (85% to 90%) and is not typically associated with other congenital anomalies; and embryonic/syndromic/congenital form, which accounts for 10% to 15% of the cases, and is associated with non-hepatic anomalies. The embryonic/syndromic/congenital form is commonly associated with non-hepatic congenital anomalies such as situs inversus, polysplenia or asplenia, vascular and cardiac malformations, and intestinal malrotation. In a large North American multicenter study, the latter group was further divided into two distinct subgroups based on the presence of laterality defects. The group with at least one major malformation, but without laterality defects, has a higher incidence of genitourinary defects like cystic kidney and hydronephrosis. The other group is syndromic with laterality defects.
BA typically presents with cholestatic jaundice and hepatosplenomegaly between 2 and 5 weeks of age. Acholic stools suggest biliary obstruction and are frequently present, but onset is commonly well after the onset of jaundice. If the infant also had a preceding history of physiologic jaundice, the cholestatic jaundice may not be recognized as new; this highlights the importance of evaluating any prolonged or new jaundice in infants. Although splenomegaly is commonly present at diagnosis, other signs of portal hypertension such as ascites generally occur later in the course of disease. As chronic inflammation and cholestasis lead to malabsorption, many infants with BA present with inadequate weight gain.
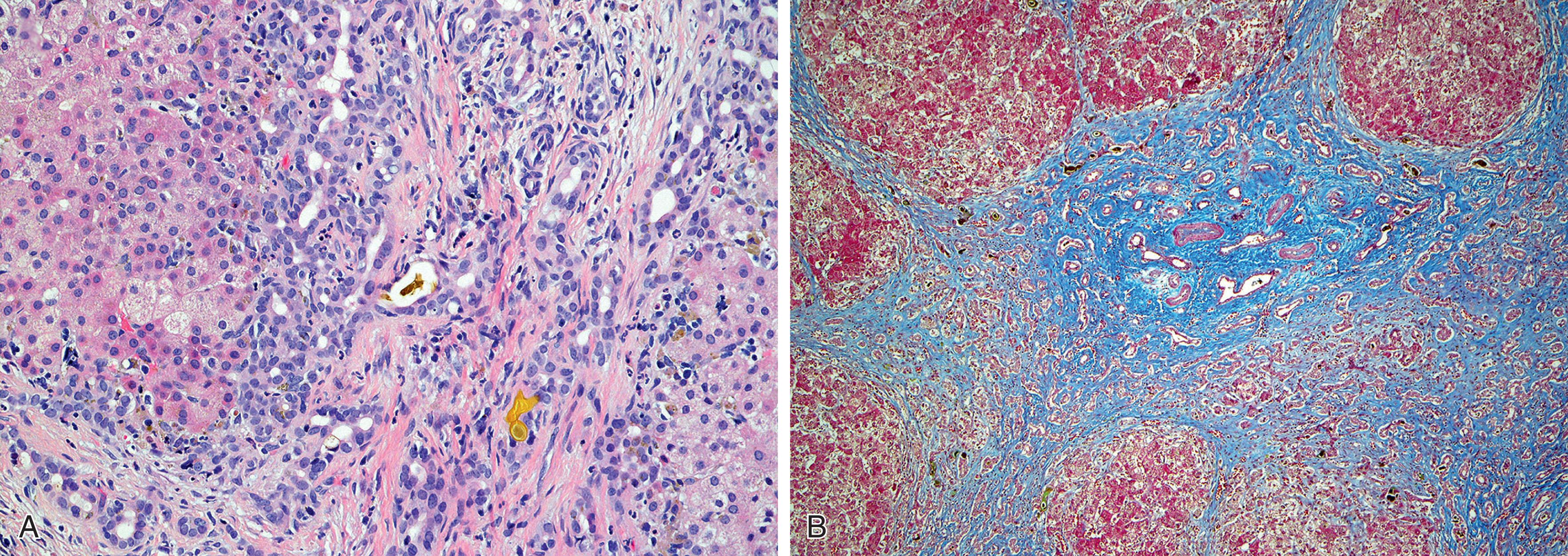
Expedient differentiation of BA from other causes of neonatal cholestasis is critical, as surgical intervention before 2 months of age has been shown to improve surgical success and outcome. If early laboratory evaluations are suggestive of BA, consultation with a pediatric hepatologist is mandatory. Laboratory evaluation early in the course of disease typically demonstrates conjugated hyperbilirubinemia between 2 and 7 mg/dL and total bilirubin levels between 5 and 12 mg/dL. Elevations in ALT, ALP, and GGT are generally seen. Abdominal US is recommended as the first-line imaging modality and may demonstrate absence of the gallbladder after adequate fasting or a fibrotic remnant of extrahepatic bile duct. However, the presence of the gallbladder does not necessarily exclude BA. In the porta hepatis, a triangular or tubular echogenic cord of fibrous tissue representing the biliary remnant may be described as “triangular cord sign.” The reported sensitivity of this sonographic finding is 80%. As a follow-up to abdominal US, hepatobiliary scintigraphy with technetium-labeled iminodiacetic acid derivatives (HIDA scan) may be used to assist in the differentiation between obstructive and nonobstructive causes of neonatal cholestasis. In BA, radionucleotide scans demonstrate rapid update of tracer but absence of excretion into the bowel at 24 hours. The sensitivity of the HIDA scans may be increased by pretreatment with oral phenobarbital (5 mg/kg/day) for 5 days. Care must be taken, however, to not delay definitive diagnosis by awaiting scan results and recognition that functional causes of cholestasis (such as hypothyroidism) can also result in a nonexcreting HIDA scan. Percutaneous liver biopsy is helpful in excluding alternate causes of cholestasis. Histopathologic findings supportive of a diagnosis of BA demonstrate bile ductular proliferation and bile duct plugging ( Fig. 65.3 ). Given the progressive nature of BA, the histologic findings will vary with the point in progression. Matrix metalloproteinase-7 (MMP-7), a protease involved in tissue remodeling, was found to have good accuracy in BA diagnosis. However, more studies are needed to further validate its use in clinical practice.
Failure to exclude BA after the above evaluation is complete necessitates surgical exploration with intraoperative cholangiogram. The diagnosis of BA may be made or confirmed at the time of laparotomy with the observation of an atretic biliary tree and intraoperative cholangiogram demonstrating lack of patency in the biliary ductal system. If BA is confirmed, surgical intervention with a Kasai hepatic portoenterostomy is recommended. The Kasai is a surgical procedure that works to restore the normal flow of bile by excising the obstructed bile ducts and creating an anastomosis of a jejunal limb of a Roux-en-Y with the liver at the porta hepatis, the area of the liver from which the bile ducts become extrahepatic. Restoration of bile flow may prevent or delay progression of disease, worsening of fibrosis, and development of end-stage liver disease. However, despite Kasai portoenterostomy, most children progress to cirrhosis and portal hypertension and ultimately require liver transplantation.
Choledochal cysts are congenital dilations of the biliary ducts which can impede bile flow, leading to liver injury. The incidence of choledochal cysts is high in the Asian population with a female predominance. Choledochal cysts can present at any age, including infancy. However, 80% of choledochal cysts are diagnosed in the first decade of life, with cholestasis being the most common sign in infants, and cholangitis or pancreatitis being less common. Choledochal cysts are associated with increased risk of choledocholithiasis, ascending cholangitis, and liver cirrhosis. There are five types of choledochal cysts based on the location of biliary dilation. The most common forms are type I (spherical or fusiform dilation of the extra hepatic biliary tree) followed by type IV (includes multiple cysts that can involve intrahepatic and extrahepatic biliary tree). The pathogenesis of choledochal cyst formation is not entirely clear. However, anomalous pancreaticobiliary union may play a role by causing reflux of pancreatic secretions into the bile duct. Diagnosis is usually made with abdominal ultrasound. Choledochal cysts need to be excised surgically, and in their entirety whenever possible. Continued surveillance for malignancy (cholangiocarcinoma and squamous cell carcinoma) is warranted after excision due to increased risk over the general population. Although not well defined for pediatric ages, screening should include regular biochemical evaluation and imaging (ultrasound or cross-sectional CT).
Alagille syndrome (ALGS) is an autosomal dominant or sporadic de novo genetic disorder with variable penetrance, characterized by chronic, progressive cholestasis secondary to a paucity of intralobular bile ducts. The estimated prevalence is 1 in 30,000 live births. The majority (more than 90%) of children with ALGS carry a mutation in the gene JAG1 , located on chromosome 20. The product of JAG1 is a ligand in the Notch signaling pathway that plays a key role in embryogenesis and the pathogenesis of the disorder. A small number of infants with ALGS have mutations in NOTCH2 .
ALGS is a multisystem syndrome characterized by cholestatic liver disease, stereotypical facial features, congenital heart disease, ocular abnormalities (most commonly posterior embryotoxon which represents prominence of Schwalbe line), skeletal abnormalities (butterfly vertebrae and rib abnormalities), and renal disease. Other features include short stature, as well as vascular and dental abnormalities. Most infants with ALGS present within the first 3 months of life with cholestasis; however, those with severe extrahepatic manifestations (usually caused by associated congenital heart disease) may present at birth or even be identified by prenatal US. Although many forms of congenital heart disease have been associated with ALGS, the most common is peripheral pulmonary stenosis. The characteristic facial features are frequently difficult to appreciate in the neonatal period but include a prominent forehead and pointed chin, giving the face a triangular appearance, deep-set eyes with hypertelorism, and a saddle nose.
When cholestatic jaundice occurs in the first 6 weeks of life, care must be taken to discriminate ALGS from alternate etiologies of neonatal cholestasis, particularly BA and other treatable etiologies for which timely initiation of treatment may change the outcome. Initial evaluation for ALGS should include serum biochemistries, abdominal US, and echocardiogram when a heart murmur is identified. In ALGS, the conjugated hyperbilirubinemia is associated with elevated serum aminotransferases and GGT, reflective of the biliary involvement. If there is clinical concern for ALGS, a spinal radiograph should be obtained to evaluate for hemivertebra or butterfly vertebra, and an ophthalmologic evaluation for posterior embryotoxon is recommended.
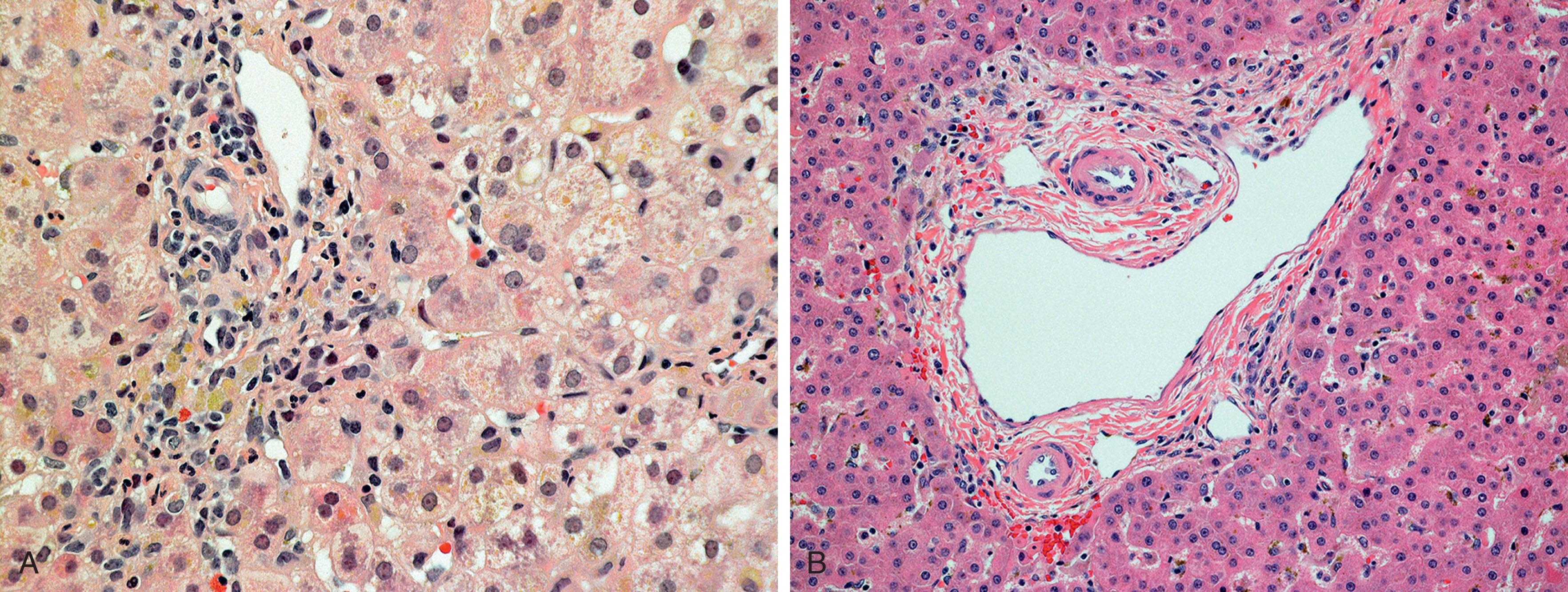
Although a liver biopsy is not required for the diagnosis of ALGS when other stereotypical syndromic features are present, biopsy should be performed when the diagnosis is in question. The histopathology in ALGS is characterized by bile ductular paucity; however, this is not pathognomonic. In the preterm infant the number of bile ducts is normally diminished, and hence care must be taken to not incorrectly make the diagnosis of pathologic paucity ( Fig. 65.4 ). In term infants and older children, the normal bile duct to portal tract ratio ranges from 0.9 to 1.8; ratios less than 0.9 are suggestive of paucity. Given the normal developmental progression of the biliary system in infancy and the importance of excluding BA, infants with cholestatic jaundice and elevated GGT usually require liver biopsy and hepatobiliary scintigraphy. Additionally, an intraoperative cholangiogram to verify patency of the extrahepatic biliary system may be required.
Metabolic bone disease is especially striking in ALGS. Elevated ALP commonly reflects abnormal bone metabolism in addition to the biliary disease. Serum bile salt levels can be extremely elevated, even in the absence of jaundice, leading to intractable and refractory pruritus. Hypercholesterolemia and hypertriglyceridemia can lead to the development of xanthomas, most prominent on extensor surfaces and areas of minor trauma, including the diaper area and plantar surfaces of feet, abdomen, and neck.
Treatment of ALGS is directed at improving or maintaining adequate nutrition, treating the complications if there is cholestasis, and supporting the cardiovascular health. The introduction of this section has details regarding nutritional management of cholestatic infants. About 21% to 31% of patients who fail medical therapy will require liver transplantation.
α-1 Antitrypsin (A1AT) deficiency is the most common genetic cause of liver disease and affects approximately 1 in 2000 live births. It is an autosomal codominant disorder that results in a reduction in α-1 antitrypsin, a serine protease produced in the liver whose role is to inhibit other proteases and elastases that can lead to cellular destruction. The genetic defect results in a single amino acid substitution within the A1AT protein, resulting in abnormal molecular folding, and inability of the protein to be processed beyond the Golgi apparatus. Excessive hepatic accumulation of the abnormal A1AT protein results in hepatocellular injury.
The clinical phenotype of A1AT deficiency includes both liver and pulmonary manifestations. Pulmonary disease generally manifests in adulthood, whereas liver involvement commonly presents in neonates. Liver disease in A1AT is most often characterized by cholestatic jaundice, which can develop in 10% of infants with PI ZZ genotype. Hepatosplenomegaly and ascites can also be seen in the most advanced cases.
A1AT deficiency is diagnosed by serologic testing and liver histology. The most specific serum test is A1AT phenotyping (Pi type). While commonly used as a less costly and widely available screening test, the serum levels of A1AT can be falsely elevated into the normal range in times of systemic inflammation or infection and so should not be used in the diagnosis of A1AT. A1AT variants are named according to their electrophoretic migration pattern. The normal protein is designated M, and the S and Z variants are the most common, leading to a reduction in serum A1AT. The homozygous PiZZ is named because it has the slowest gel migration and causes the most severe disease phenotype. Generally liver disease manifests only in PiZZ, PiSZ, or, rarely, PiMZ variants.
The classic, but not pathognomonic, histologic finding in A1AT deficiency is periodic acid-Schiff (PAS)-positive diastase-resistant eosinophilic globules within the hepatocytes. These globules represent the accumulated abnormal protein trapped within the endoplasmic reticulum. Liver histology may also demonstrate bile duct destruction, proliferation, and, potentially, bile duct paucity, making it important to exclude BA and ALGS.
Although recombinant A1AT has been used for the treatment of the pulmonary manifestations, management of the associated liver disease is primarily supportive, as there are no specific or targeted therapies currently available. As in all disorders resulting in cholestasis, fat malabsorption is common with A1AT deficiency. Cholestatic infants usually benefit from MCT-rich formula to aid the fat absorption and supplementation with fat-soluble vitamins as needed. Additionally, ursodeoxycholic acid may be utilized to improve bile flow; however, no study has demonstrated clear benefit. Historically, breastfeeding was thought to be of some benefit. However, in a study comparing formula-fed with breastfed infants, no benefit was found. To prevent acceleration of pulmonary manifestations, including early emphysema, avoidance of smoking and environmental pollution is critical.
For infants and children with end-stage liver disease, liver transplantation is indicated. As most A1AT is manufactured in the liver, the recipient assumes the donor’s Pi phenotype and, posttransplant, experiences normal serum levels of the functional protein, decreased risk of pulmonary disease, and no chance of recurrent disease in the transplanted organ.
While cystic fibrosis (CF) is common, affecting approximately 1 in 2500 births in North America, CF-related liver disease is uncommon in the neonatal period. It is estimated that less than 2% of infants with CF present with cholestasis. Given the low incidence of CF-related liver disease in neonates, testing for CF beyond state-mandated newborn screens should be reserved for those infants in whom alternate causes of cholestasis have been excluded or in infants with other typical features of CF, including meconium ileus or inadequate weight gain despite theoretically adequate caloric intake.
There are several steps in the synthesis of bile acids that may be disrupted, leading to an accumulation of hepatotoxic bile acid intermediates. Bile acid synthesis disorders are rare autosomal recessive disorders, with a prevalence of 1 in 50,000 in the general population. In the neonatal period, phenotypes of bile acid synthetic disorders include acute hepatitis, acute liver failure, persistent cholestasis, and progressive chronic hepatitis.
Cholic acid and chenodeoxycholic acid are the primary bile acids in humans, and disruption at any step in their synthesis results in the accumulation of toxic intermediate metabolites. Liver injury associated with disorders of bile acid synthesis occurs secondary to direct hepatocellular injury from accumulation of toxic intermediates or secondary to the accumulation of cholesterol, drugs, and other toxins within the liver from abnormal bile excretion.
The age at presentation with a disorder of bile acid synthesis is variable, ranging from early infancy to adulthood. The most common clinical presentation includes neonatal jaundice, failure to thrive, hepatosplenomegaly, metabolic bone disease, and bleeding early in childhood. Pruritus is usually absent. Some disorders are associated with progressive neurologic disease, manifesting with seizures, developmental delay, deafness, blindness, and neuromuscular weakness.
Laboratory testing in infants with bile acid synthetic disorders demonstrates normal or low serum bile acid levels, elevated serum aminotransferases, normal GGT, and complications of fat malabsorption, including fat-soluble vitamin deficiency. If serum bile acids are found to be low, urinary bile acids should be measured for identification of the particular synthetic defect. Liver biopsies are generally nonspecific and can demonstrate canalicular bile plugging, inflammation without bile duct proliferation, and sometime a picture similar to those observed in idiopathic neonatal hepatitis such as giant cell transformation.
Treatment of inborn errors of bile acid synthesis focuses on supporting normal growth and supplementation of fat-soluble vitamins. Treatment with cholic acid is a preferred therapy for the most common disorders of primary bile acid synthesis because cholic acid suppresses the production of the toxic bile acid intermediates. Ursodiol is not indicated as it does not suppress production of abnormal bile acid intermediates.
Progressive familial intrahepatic cholestasis (PFIC) is a group of autosomal recessive disorders characterized by defective bile export leading to cholestasis. This group of disorders is classified based on the genetic mutation, and they are named PFIC 1, PFIC 2, and PFIC 3. Liver disease in PFIC results from accumulation of bile salts within the hepatocytes leading to profound cholestasis, fat-soluble vitamin deficiency, and intractable pruritus.
PFIC 1, also known as Byler disease, is caused by a mutation in the gene ATP8B1 on chromosome 18q21-22, which encodes for a protein flippase (FIC 1) that facilitates the flipping of aminophospholipids from the outer to inner canalicular membrane. As the gene is also expressed in many extrahepatic tissues, affected individuals may also have short stature, deafness, pancreatitis, and persistent diarrhea.
PFIC 2 results from a defect in the bile canalicular bile salt export pump (BSEP) caused by a mutation in the gene ABCB11 on chromosome 2q24. BSEP is responsible for transporting bile acids from inside the hepatocyte to the canaliculus. Disruption of BSEP results in accumulation of bile acids within the hepatocyte resulting in severe cholestasis and rapid progression to end-stage liver disease. PFIC 2 presents earlier and is a more rapidly progressive liver disease than PFIC 1. Children with PFIC 2 have an increased risk of developing hepatocellular carcinoma, a risk that persists even after liver transplantation.
PFIC 3 is caused by a mutation in the gene ABCB4 on chromosome 7q21, which encodes for multidrug resistance–associated protein 3 (MDR3) and mediates flopping of aminophospholipids from the inner to outer canalicular lipid bilayer. Rather than a deficiency in bile acid export, patients with PFIC 3 have a deficiency in phospholipid export. The resultant bile lacks phospholipids, making the micelles unstable and toxic to bile ducts, leading to a progressive intrahepatic cholangiopathy. In contrast to PFIC 1 and 2, only a third of children with PFIC 3 present with cholestasis during infancy, with most presenting in later childhood and adolescence. When infants with PFIC 3 do present with liver disease, they commonly have cholesterol gallstones complicating their intrahepatic cholestasis.
Infants with PFIC generally have markedly elevated serum bile acid levels with only mildly elevated serum bilirubin. The characteristic biochemical markers of PFIC 1 and 2 are a normal or low GGT, normal serum cholesterol, and only mild transaminitis; however, specific diagnosis requires genetic testing. PFIC 3 presents with an elevated GGT in the absence of extrahepatic biliary obstruction. The intrahepatic cholestasis that is commonly seen in PFIC often progresses to end-stage liver disease. Liver biopsy shows canalicular cholestasis and biliary plugs. More pronounced hepatocyte injury and giant cell hepatitis is noted in PFIC 2.
Treatment for PFIC initially focuses on the nutritional management of cholestasis because of insufficient absorption of fat and fat-soluble vitamins. Most dietary fat should be provided from MCT oil, which does not depend on bile salts for absorption. Additionally, aggressive treatment of debilitating pruritus with ursodiol, antihistamines, cholestyramine, rifampin, and opioid antagonists is often required. In refractory cases, treatment may include partial biliary diversion, interruption of the enterohepatic circulation by surgical ileal exclusion, and liver transplantation.
Congenital hepatic fibrosis (CHF) is a hereditary malformation of the bile ducts resulting from failure of remodeling during embryogenesis. It is an autosomal recessive disorder that may present in isolation but is more often seen as a feature of several syndromes, including Ivemark, Berdet-Biedl, Caroli, and Joubert syndromes; autosomal recessive polycystic kidney disease (ARPKD); and disorder of glycosylation type 1b.
Caroli syndrome is characterized by CHF and ductal ectasia with cystic dilation of intrahepatic ducts. Infants with CHF most commonly present with portal hypertension and splenomegaly, although some present with cholestasis caused by cholangitis. Characteristically, CHF is associated with normal transaminases and intact synthetic function despite advancing portal hypertension. When complicated with cholangitis, transient elevation of GGT and conjugated bilirubin are typically seen. Diagnosis of Caroli syndrome may be made by imaging with abdominal US with Doppler or magnetic resonance imaging (MRI) of the liver with magnetic resonance cholangiopancreatography. When associated with ARPKD, CHF can be diagnosed clinically, but if in isolation, histologic diagnosis is necessary.
Treatment of CHF is aimed at treating complications of portal hypertension and preventing and treating cholangitis. Portosystemic shunting is commonly required to decompress advanced portal hypertension. In Caroli syndrome, focal cystic dilation may be amenable to liver lobectomy, but, if diffuse, liver transplantation is required.
Congenital or perinatal infections and sepsis are common causes of neonatal liver cholestasis, hepatitis, and sometimes liver failure. A careful history and physical examination may suggest infection as an etiology of neonatal liver disease. For ill-appearing infants with cholestasis, a rapid evaluation for bacterial infection (such as sepsis or urinary tract infection) is recommended. Judicial selection of antimicrobials must be considered, as several are known to exacerbate cholestasis by displacing bilirubin from albumin (e.g., ceftriaxone) or cause direct hepatotoxicity (e.g., sulfamethoxazole/trimethoprim and fluconazole). In addition to common bacterial infections, TORCH infections (toxoplasmosis, rubella, cytomegalovirus, herpes, and syphilis), as well as infections with hepatitis B, parvovirus B19, adenovirus, or echoviruses, can result in neonatal cholestasis and hepatitis. For more detail regarding diagnosis and specific treatments for congenital or neonatal infections, please refer to Part IX of this text, Immunology and Infections.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here