Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Virtually every woman with a breast lump, breast pain or discharge from the nipple fears she has cancer. The anxiety results from the unknown course of the disease, the threat of mutilation and the fear of dying. This has often prevented women from seeking medical advice, but publicity about self-examination and screening (see Ch. 6 ) and the potential benefits of early treatment has encouraged earlier presentation.
Anxiety may be heightened by friends’ or relatives’ experiences of breast cancer or a recent ‘celebrity diagnosis’; for this reason, reassuring the ‘worried well’ is important. The effects of breast surgery on attractiveness and femininity must be considered; breast care nurses can provide psychological support throughout investigation and treatment.
Rates of referral to breast clinics have increased, reflecting easier access, widespread breast screening and public awareness of breast cancer. Despite the fears of those referred, in the United Kingdom less than 15% prove to have cancer. The rest include benign breast conditions and others within the normal range of anatomy and physiology ( Box 45.1 ).
Ductal adenocarcinoma
Lobular adenocarcinoma
Sarcoma
Metastasis from other tissues
Fibroadenoma
Intraduct papilloma
Lipoma
Fibroadenosis (also known as fibrocystic disease , benign mammary dysplasia and chronic mastitis )
Chronic periductal inflammatory reaction caused by retained duct secretions
Cellulitis and breast abscess
Subareolar abscesses in mammary duct ectasia
The breast consists of 15 to 20 lobes containing lobules linked by ductules that combine to form ducts. The glandular tissue is supported by fibrous tissue connected by Astley Cooper ligaments and lies over pectoralis major and minor. It is supplied by branches of the axillary and internal mammary arteries. Lymph drains primarily to the axillary nodes.
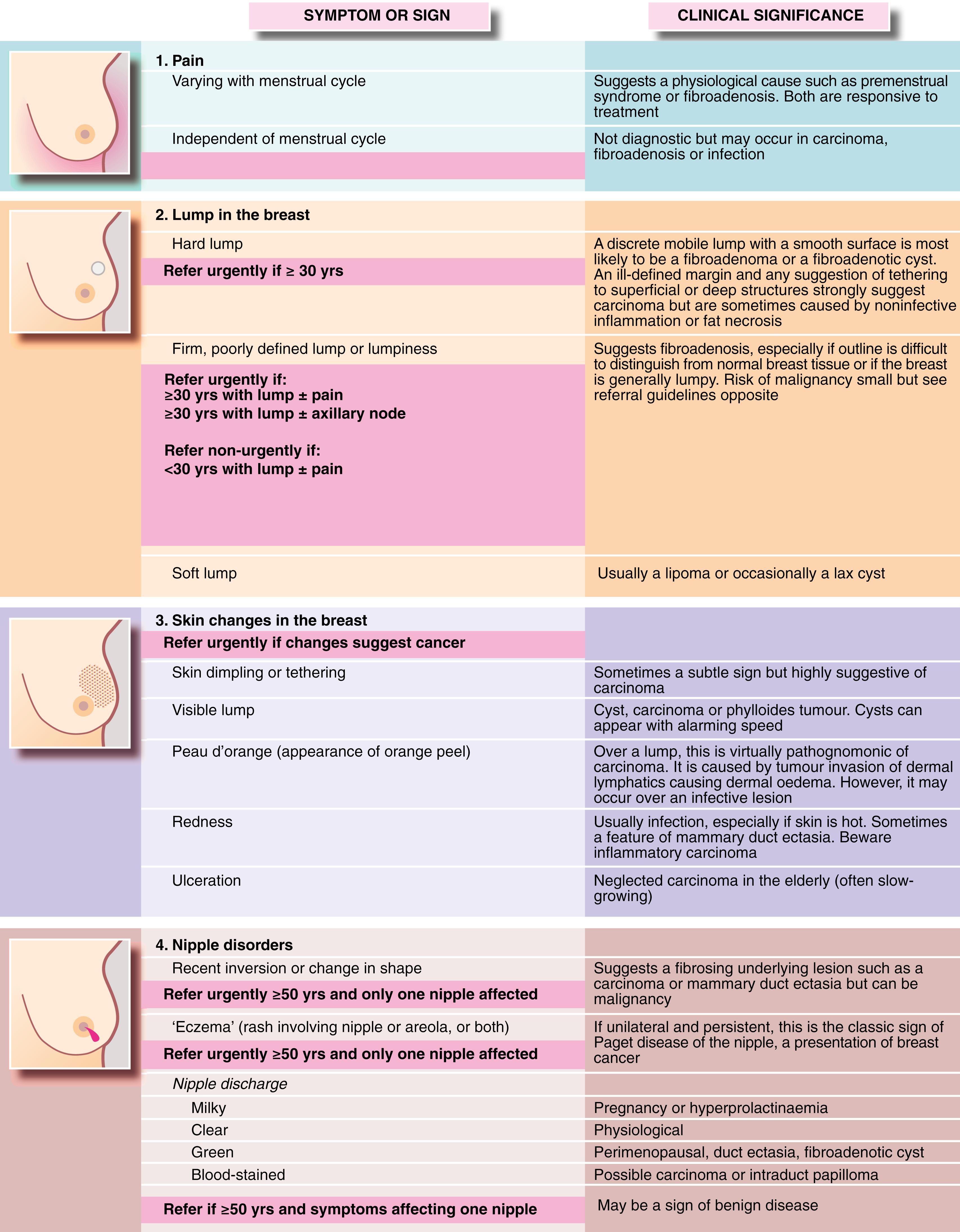
Patients may present with symptoms or signs ( Fig. 45.1 ). Two-thirds complain of a discrete lump or lumpiness.
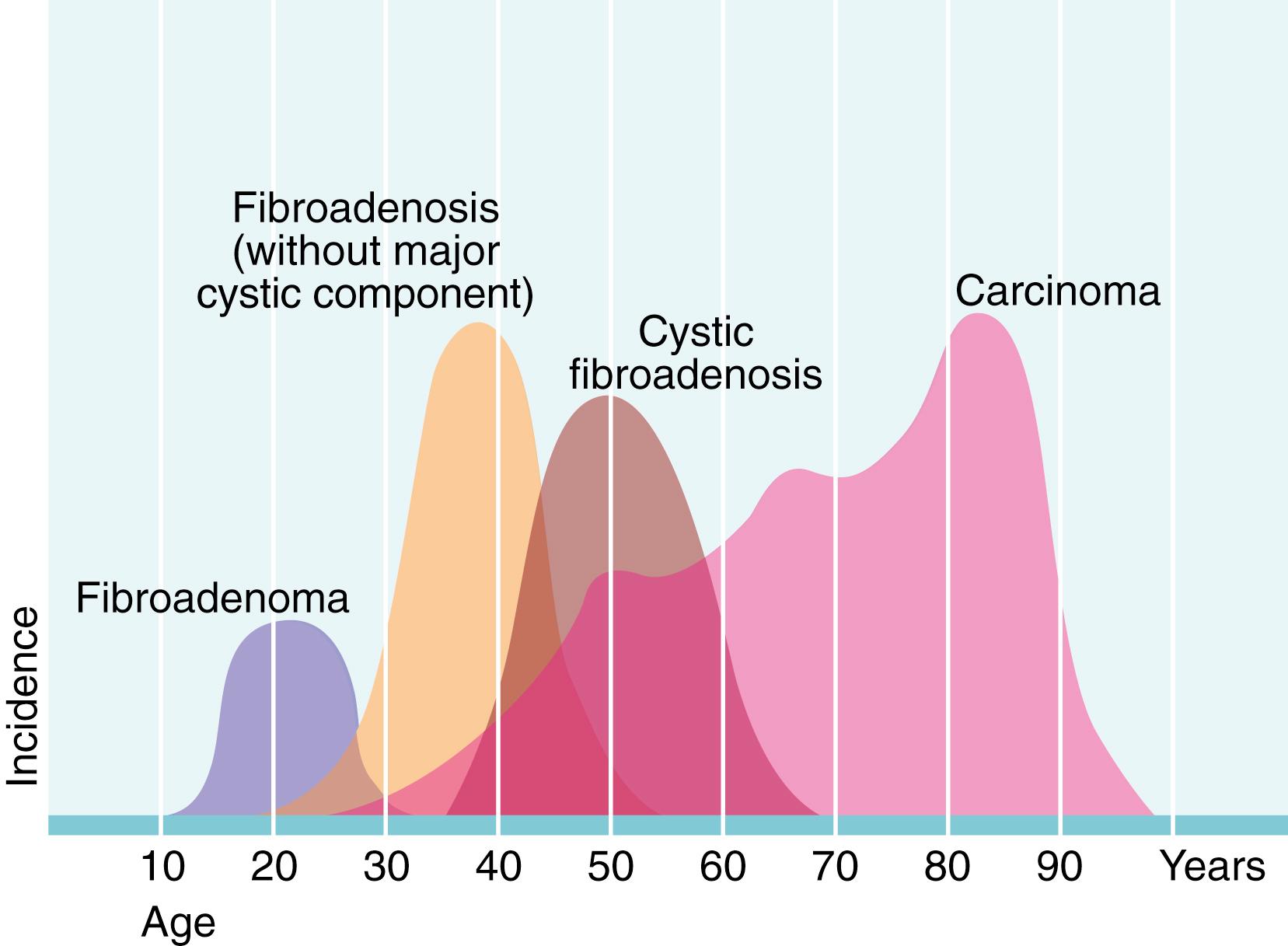
A detailed history can provide important clues to the pathology of a breast problem. Age alters the probability of different breast disorders ( Fig. 45.2 ); in particular, the risk of malignancy rises with age. The duration of symptoms should be established at the outset; cancers are usually slow-growing, whilst cysts can appear rapidly, sometimes almost overnight. Benign conditions, such as fibroadenosis and fibroadenoma may present with lumps that fluctuate with the menstrual cycle or have decreased in size since first noticed. They are also more likely to be painful and tender than a malignant lesion.
A previous history of breast conditions, particularly malignancy, cysts or fibrocystic change, can be an indicator of the nature of a current breast problem. Aside from high risk predisposing germline gene mutations, the greatest single risk factor for breast cancer is a previous history of the condition, however long ago (1% risk per year)— Box 45.2 ). There is some evidence that patients with recurrent benign breast disorders are at greater risk of cancer. If cancer is confirmed, it is important to establish the patient’s menopausal status as this influences future treatment decisions. If this is unclear, serum follicle-stimulating hormone and oestradiol levels should be measured.
Increasing age
Family history (number of first- and second-degree relatives, their age of onset and bilaterality, known BRCA1 / BRCA2 mutations)
Previous history of breast cancer or carcinoma-in-situ
Early age of menarche (age <12 years)
Late age of menopause (age >55 years)
Late age at first full-term pregnancy (age <20 years protective)
Nulliparity
Previous breast biopsies showing nonmalignant abnormalities
Hormonal therapy—oral contraceptive pill or hormone replacement therapy
Radiation at a young age (mantle irradiation for lymphomas, atomic bomb survivors)
See also http://www.cancerresearchuk.org/about-cancer/breast-cancer/risks-causes/risk-factors
Trauma from seatbelt injuries is common and patients should be asked whether bruising of the breast was followed by the appearance of a lump.
Drug history , particularly of the oral contraceptive pill (OCP) or hormone replacement therapy (HRT), should be recorded, including the type, duration and how recently the drug has been used. These drugs modulate the hormonal environment of breast tissue and tend to increase the risk of breast cancer. Other hormone-related risk factors for cancer include late age at first full-term pregnancy, lower parity (number of pregnancies), early age of menarche and late age of menopause. Enquiry should be made about a family history of breast or ovarian cancer, including number of first- and second-degree relatives, age of onset and bilaterality. Some families have mutations in the tumour suppressor genes BRCA1, BRCA2, PALB2 and others, which can strongly predispose to breast and other cancers. Increasing alcohol consumption is fuelling a rise in the incidence of breast cancer.
There are several accepted methods for examining the breasts; one is shown in Fig. 45.3 . All areas of the breast must be examined, with particular attention to the axillary tail and retroareolar regions. Breast examination involves six distinct manoeuvres:
observation with the patient sitting up;
observation with the patient raising and lowering her arms;
examination of the nipples;
systematic palpation of each breast;
palpation of axilla and supraclavicular fossa;
general examination for signs of distant metastases.

During inspection, the signs to be looked for are listed in Fig. 45.1 .
Palpation may be done circumferentially using the flat of one hand, starting at the nipple then moving in progressively larger circles; radially from the nipple outwards, like the spokes of a wheel; or by sectors , examining each quadrant in turn. Axillary lymph nodes are palpated, whilst the examiner’s other hand supports the patient’s arm (see Fig. 45.3G and H ). This helps relax the muscles and aids assessment of the nodal groups ( medial, lateral, anterior, posterior and apical ). Note that clinical assessment of axillary nodes is unreliable, with a 30% false positive and a 30% false negative rate.
A history of nipple discharge can often be confirmed by pressure over the appropriate sector near the areola. Discharges not obviously blood-stained should be tested for blood using urinalysis dipsticks. In all cases, a smear preparation should be examined for cytological abnormalities.
The differential diagnosis of a discrete breast mass is:
cyst
fibroadenoma
focus of fibrocystic change or fibroadenosis
fat necrosis (rare)
carcinoma
During the examination, the patient needs to point out any lump she is worried about. The normal breast has a wide range of textures, from soft through nodular, to hard, so the texture of the rest of the breast must be taken into account. When a lump is found, its characteristics should be defined ( Box 45.3 ), in particular whether it is discrete or dominant or whether it is an area of nodularity or ‘thickening’. If there is a discrete mass, does it appear benign or suspicious for malignancy? (Characteristic signs of cancer are shown in Fig. 45.4 ). Note that even for breast specialists, clinical examination has a low sensitivity (i.e., ability to detect real abnormalities) of 65% to 80%. In one clinical evaluation system, increasing levels of suspicion are graded E1 to E5; an E3 designation may prompt a core biopsy even if radiological findings are not suspicious. Only 3% of breast cancers occur under the age of 30 years but a discrete lump in a patient over 65 years is a cancer until proved otherwise.
Solitary or multiple
Size—in centimetres
Location—quadrant of breast or clock face
Contour—smooth and round/ovoid (likely to be benign) or firm/hard (probable malignancy)
Mobility—mobile (likely to be benign) or fixed (probable malignancy)
Associated changes—skin/nipple retraction, skin tethering, bloody nipple discharge, erythema
Axillary lymphadenopathy—enlarged and mobile or enlarged and fixed
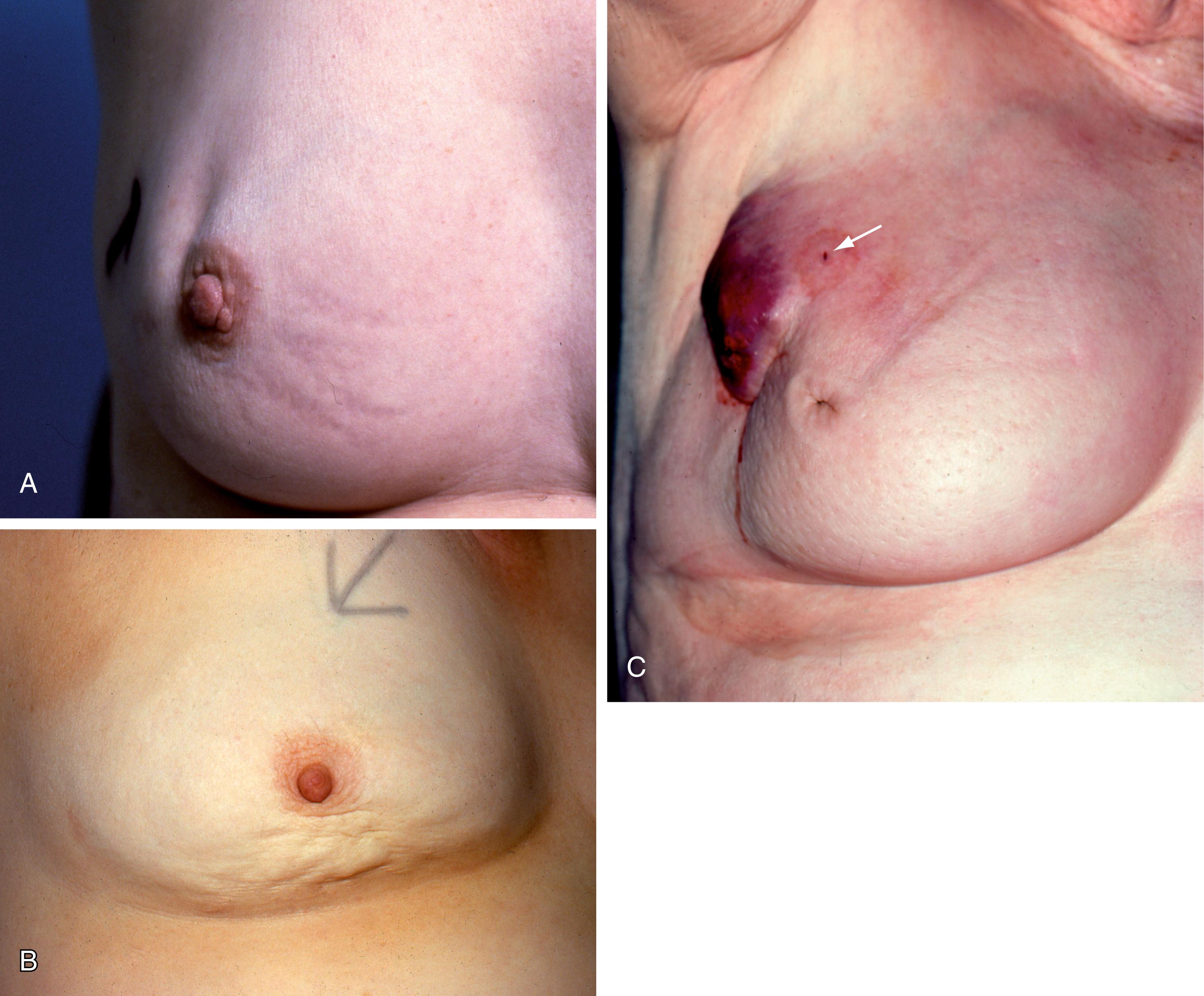
Skin tethering (as opposed to direct infiltration) can be a subtle sign and is accentuated by raising the arms to put the breast suspensory ligaments under tension. Deep fixation can be assessed by checking the mobility of the lump over pectoralis major with the muscle relaxed and then tensed.
Some patients with breast carcinoma present with eczema-like reddening and thickening of the skin of the nipple and areola, together with fissuring and ulceration. This is more common in the elderly and is known as Paget disease of the nipple (see Fig. 45.10 ).
‘One-stop’ clinics allow rapid and comprehensive preliminary assessment. Triple assessment includes clinical examination, breast imaging and biopsy (when indicated) on the same day. This has an overall accuracy of 99.6%, when performed by experienced personnel, meaning the chances of missing a cancer are less than 1%; patients shown not to have cancer can usually be discharged. If there is a clinically suspicious lump and needle biopsy is negative or equivocal, diagnostic excision biopsy should be performed. The discrete lump is completely excised and examined histologically.
Mammography (breast radiography) is an important method of radiological assessment of the breasts. In women over 40 years, it has a sensitivity of 88% for carcinoma. It is less sensitive in younger women because the breast tissue is denser, and is rarely performed below 35 years.
During mammography, the breast is compressed firmly in the machine. This spreads the tissue to an even thickness to give correct exposure for all the breast tissue to make it easier to detect any mass lesion. Radiological views are taken in two directions, mediolateral oblique and craniocaudal. Localised compression views can reduce the problem of superimposed structures simulating a mass. Focused magnified views can better display any abnormal area. Full digital mammography, which permits postprocessing enhancement of the image, has nearly replaced film mammography.
Features looked for on a mammogram include:
the presence of a mass lesion
microcalcification
architectural distortion
asymmetry
skin thickening
lymph nodes
A typical carcinoma appears as a spiculated mass lesion (dense centre with radiating lines), which may have malignant-type fine linear or granular microcalcification ( Fig. 45.5 ). Fine granular microcalcification within a spiculate lesion is virtually pathognomonic of cancer. Tumours as small as 2 to 3 mm are sometimes detectable radiologically, long before they become palpable.
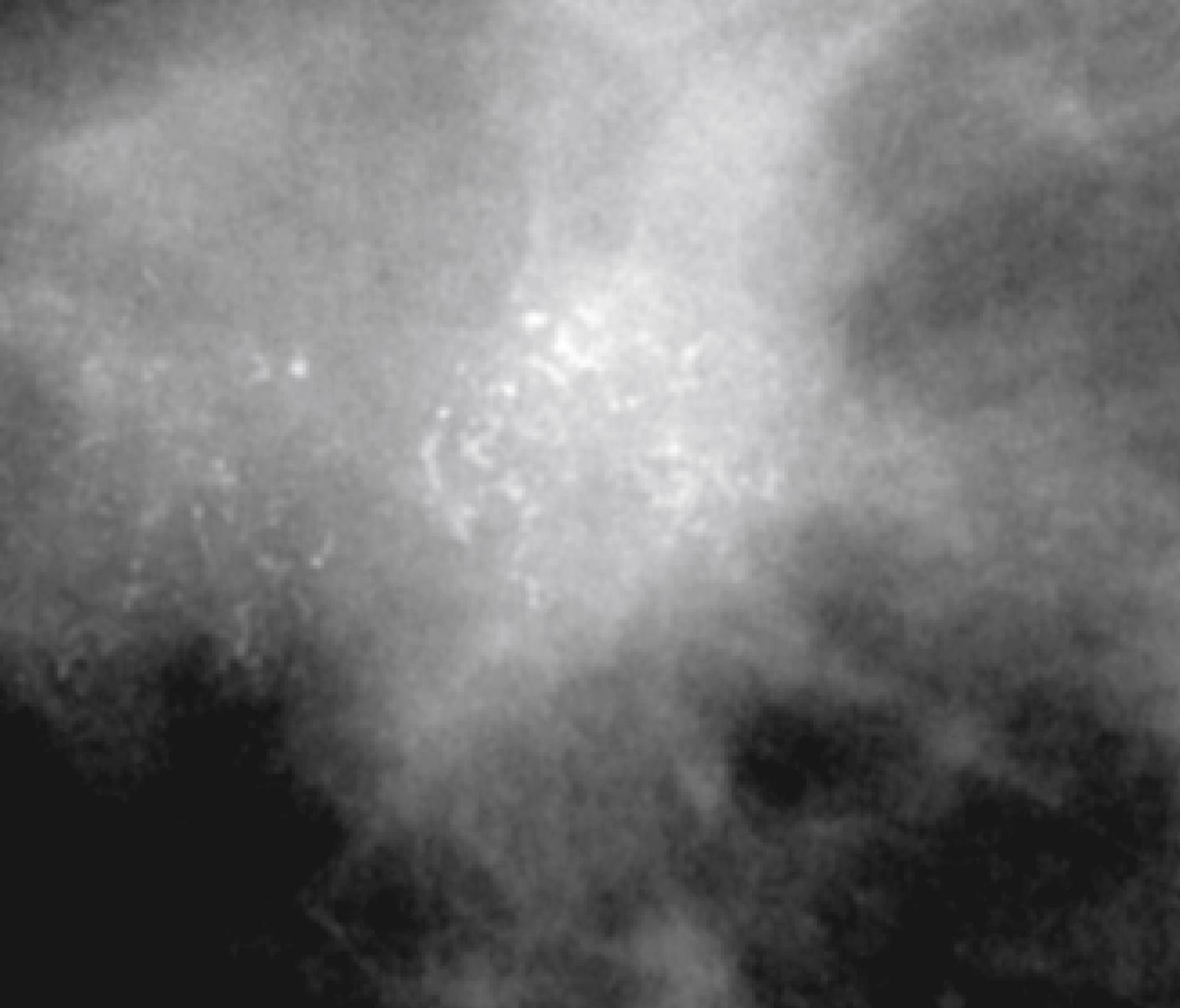
Benign-type microcalcification is coarse and ‘chunky’ ( Fig. 45.6 ). Fine branching microcalcification is characteristic of ductal carcinoma-in-situ (DCIS) . Architectural distortion and asymmetry are subtle radiological signs, but should be viewed with suspicion.
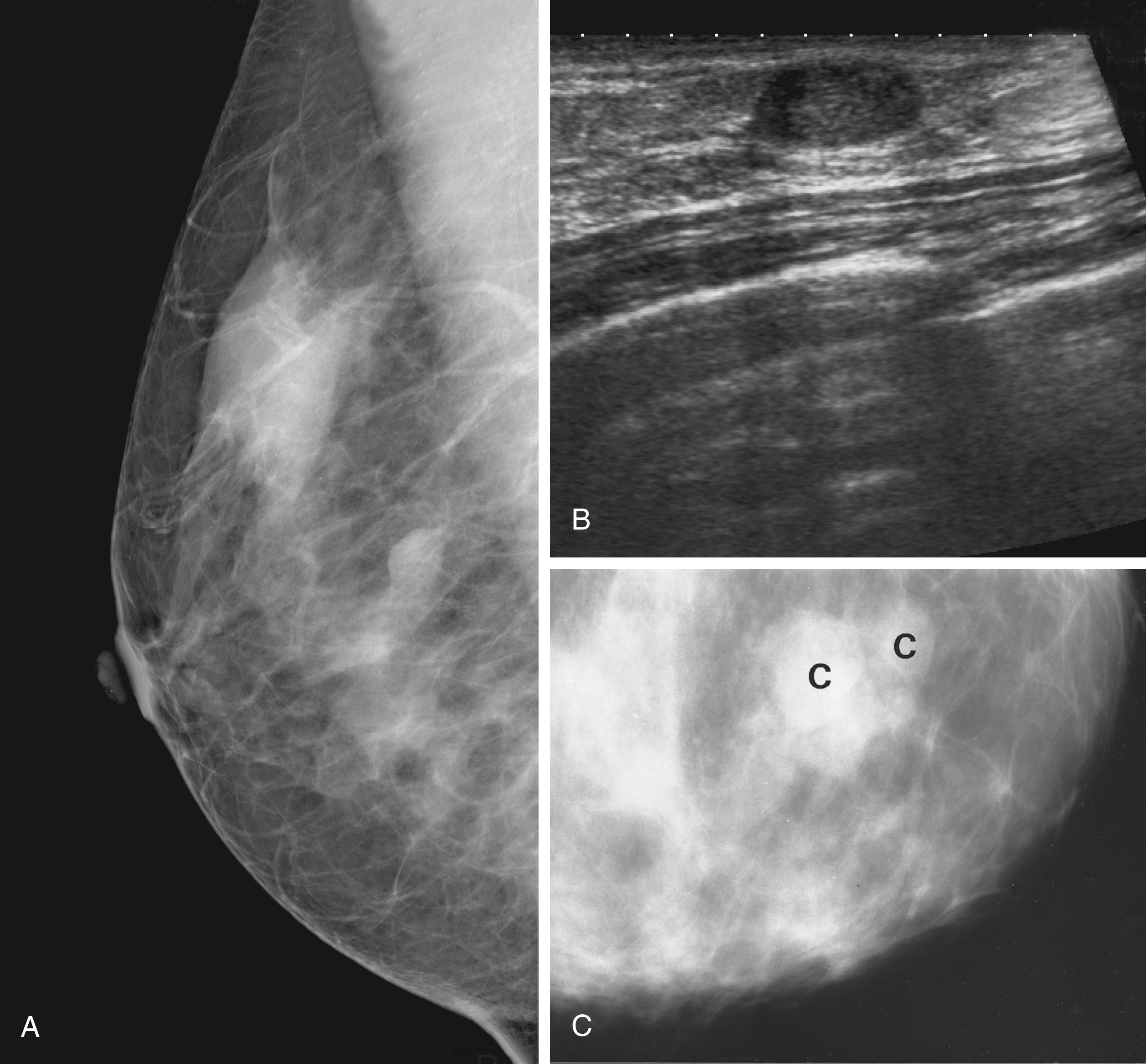
Ultrasound has long been used to distinguish solid lesions from cysts and has a specificity of 100% for this. Modern B-mode ultrasound demonstrates breast anatomy in great detail and is complementary to mammography. Benign lesions can be distinguished from malignancy with a sensitivity for cancer of at least 85%. Ultrasound can accurately measure the size of a cancer ( Fig. 45.7 ) and can guide percutaneous needle biopsies and cyst aspiration ( Fig. 45.8 ).
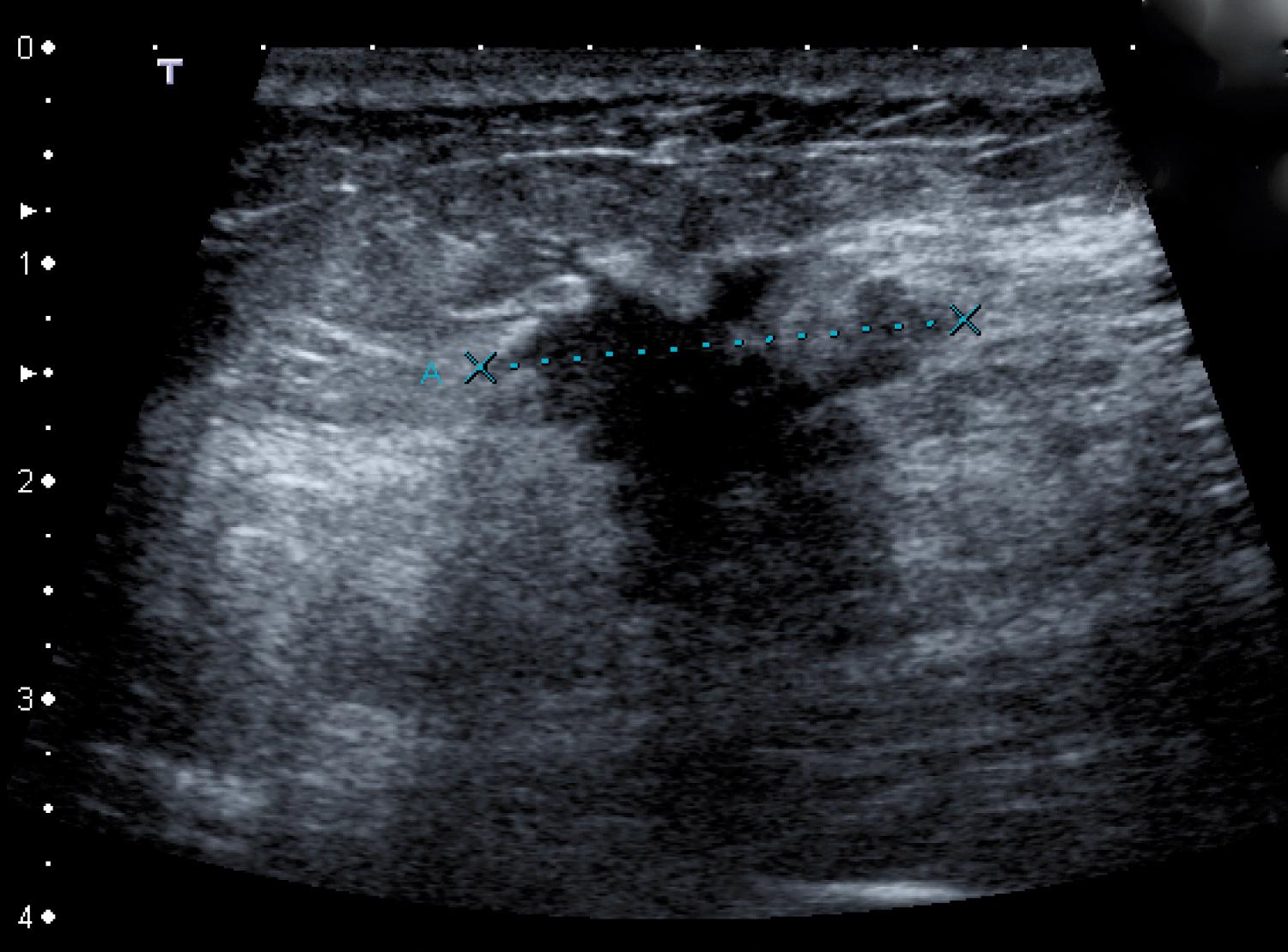
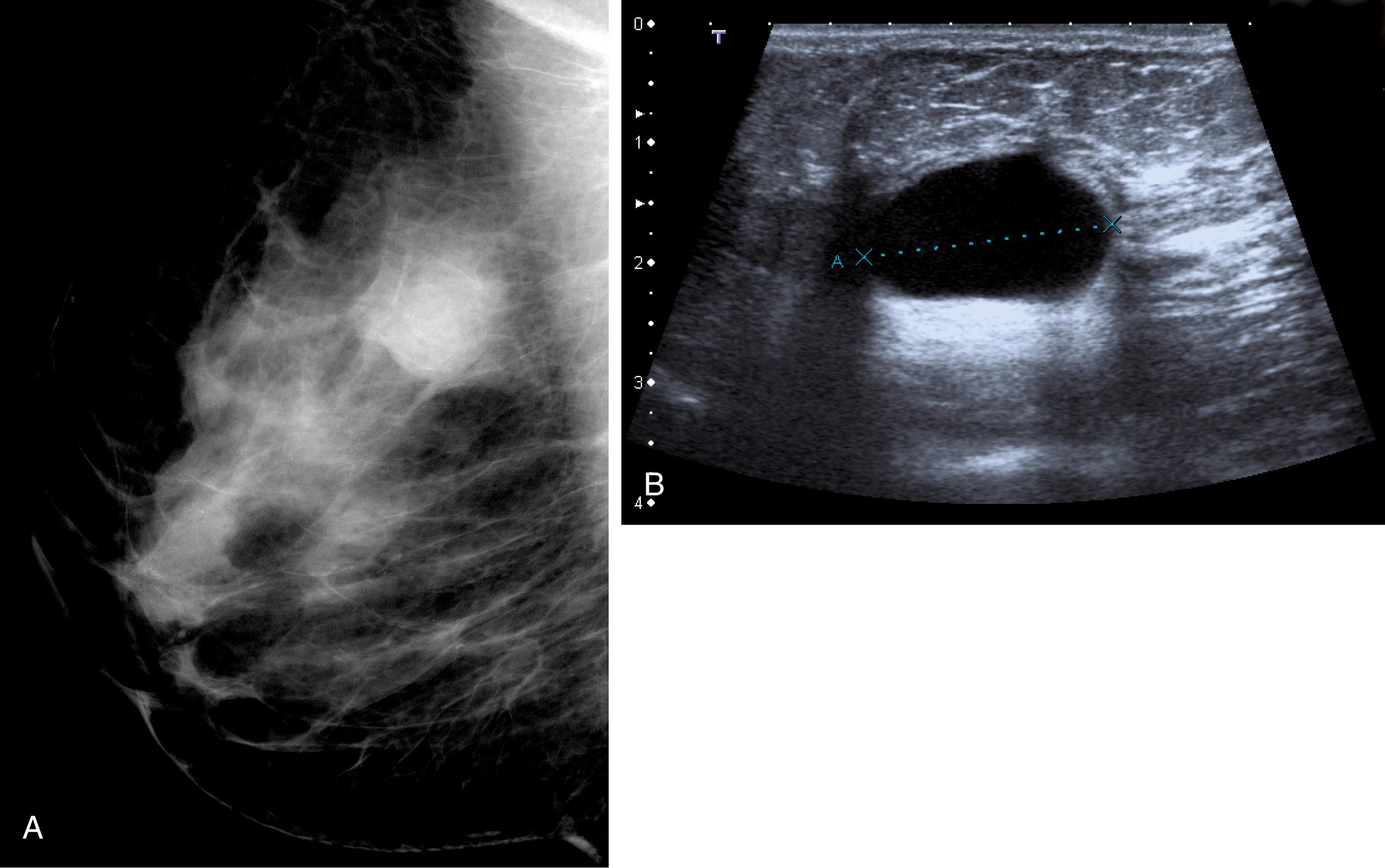
The strength of breast imaging comes from performing mammography and ultrasound together, as the physical characteristics tested by the two techniques are different. The information acquired by mammography results from attenuation of the x-ray beam through breast structures, whilst ultrasound tests the reflectivity of a pulsed ultrasound beam (of about 12 mHz), caused by subtle attenuation changes at tissue interfaces within the breast.
Most palpable and all nonpalpable image-detected masses are biopsied under image guidance, as are suspicious areas of calcification. Fine-needle aspiration cytology (FNAC) specimens are rarely used for tissue diagnosis now ( Box 45.4 ). FNAC has a sensitivity of 95% for detecting malignancy, but cannot distinguish between in situ and invasive cancers. By contrast, core biopsy has a sensitivity of 98%. The tissue architecture is preserved so that invasion can be confidently diagnosed on histology and tumours can be pathologically graded. After core biopsy, patients need to return later for the results as the pathology has to be read after the specimen has been fixed. This has the advantage that any bad news can be broken in a phased manner. If needle biopsy is negative or equivocal, a discrete lump should be completely excised with a wide margin of apparently normal breast tissue and the specimen examined histologically. This procedure, excision biopsy, can also form the first step in controlling local disease.
C1—inadequate specimen
C2—benign
C3—suspicious but probably benign
C4—suspicious and probably malignant
C5—malignant
Eczematous lesions suspicious for Paget disease of the nipple can be ‘punch’ biopsied under local anaesthesia in the clinic.
In Western societies, breast cancer is the leading cause of death in European women. About 1 in 8 to 10 women will develop breast cancer (i.e., a lifetime risk of ∼10%–12%) and ∼1 in 18 will die from it. In the United Kingdom, more than 50,000 new cases are diagnosed annually and ∼12,000 women die each year. Worldwide, there are about half a million deaths from breast cancer each year, but despite this increasing global incidence, mortality rates have gradually fallen with earlier diagnosis and improved treatments, including advances in hormonal and targeted therapy. Around 27% of cases in the United Kingdom are preventable.
Age is a major risk factor. Incidence rates rise from about 25 years, more steeply between 40 and 55 years, with a slight levelling off until about 70 years. After that, another fairly steep rise continues into old age (see Fig. 45.2 ). Breast cancer is the commonest cause of death in women aged between 40 and 50 years.
The aetiology of breast cancer is multifactorial, with genetic factors being relatively more important in premenopausal women and environmental factors more so after the menopause. These play a small role in calculating the risk of breast cancer, but the risk is greater in women with a strong family history (two first-degree relatives, bilateral breast cancer or diagnosis before the age of 50 years). Such a family history accounts for 10% of cancers, with half caused by genetic mutations, mainly BRCA1 (17q21) and BRCA2 (13q41) genes, which are transmitted in an autosomal dominant fashion. A mutation in either of these leads to an 80% to 90% lifetime risk of developing the disease. The same mutations are also strongly linked to ovarian and other cancers. Women with a BRCA mutation should be counselled about their individual risk of breast and ovarian cancer and the treatment options (ranging from surveillance to risk-reducing bilateral mastectomies, which reduce the cancer risk by more than 90%, and oophorectomy).
Growth of most breast cancers is promoted by oestrogens, hence reproductive physiology and behaviour influence cancer risk. It has long been known that nulliparous women are at greater risk: Ramazzini commented in 1703 that breast cancer was common in Catholic nuns, who as ‘Vestalis Virgines’ were prone to ‘horrendis mammarium canceris’.
The interval between menarche and menopause is the oestrogen window and is an estimate of cumulative exposure to endogenous oestrogen; the longer the interval, the higher the cancer risk. Women who begin menses before the age of 12 years, or start the menopause after 55 years are at an increased risk. A natural or a ‘medical’ menopause under 40 years reduces cancer risk by two-thirds. Nulliparity and a late age at first pregnancy increase risk and a first full-term pregnancy under 20 years halves the risk compared with one between 30 and 35 years or nulliparity, although the risk is still small.
Prolonged use of the OCP increases the risk of breast cancer by 20% and combined HRT for more than 10 years also increases the risk, although this falls when HRT is stopped.
Breast cancer is more common in the Western world and in women in higher socioeconomic classes. Obese women are at a higher risk, possibly caused by conversion of androgens to oestrogen in adipose tissue. Consuming more than three units of alcohol a day increases the risk by 50%.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here