Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Lumbar intervertebral discs are complex structures subjected to significant axial compressive forces. Because of biomechanical demands and the inability to remodel as a result of an avascular nature, lumbar disc herniation (LDH) is a relatively common cause of back pain and/or leg pain. The clinical course of LDH is often favorable and many patients improve with conservative treatment. Yet LDH can induce significant radicular symptoms or weakness, which may lead to permanent neurological dysfunction, thus necessitating surgical intervention. Approximately 300,000 lumbar discectomy procedures are performed each year in the United States. The etiology is multifactorial, with family history, obesity, and heavy lifting being implicated. Isolated trauma or injury has not been found to be a consistent risk factor, occurring in only 0.2% to 10.7% of adults with a herniation.
From a pathophysiology perspective, LDH results from degeneration of the intervertebral disc constituents, causing disc dehydration and inability to resist axial compression of the spine. Several different surgical techniques have been used to manage LDH including open discectomy (with or without the use of a surgical microscope), automated percutaneous discectomy, minimally invasive tubular endoscopic discectomy, and chemonucleolysis. The clinical outcome for these procedures is generally favorable with 65% to 90% of patients undergoing surgery reporting good or excellent results. Several studies have demonstrated improved clinical outcomes with surgery compared with conservative treatment.
Despite these favorable outcomes, a number of patients who initially respond well to surgery have a return of symptoms similar to their preoperative state because of a recurrence of herniated disc material at the prior surgical site. The reported incidence of recurrent LDH ranges from 2% to 25%. When it occurs, recurrent herniation is a major contributor to debilitating pain, disability, and the need for reoperation following the primary procedure. It also places a significant burden on the healthcare system. Ambrossi et al. have demonstrated that the mean cost of caring for patients requiring reoperation for recurrent disc herniation to be 39,386 US dollars per patient compared with a mean cost of 2315 US dollars for patients responding to conservative management. In this chapter, we discuss the anatomy and clinical presentation, along with the treatment of LDH, including primary, recurrent, and residual herniation. Additionally, existing literature comparing the various techniques employed for the treatment of LDH is briefly reviewed.
Intervertebral disc consists of an outer annulus fibrosus (AF) and inner nucleus pulposus (NP). The inner NP is composed of type II collagen and proteoglycans that facilitate water retention, producing hydrostatic pressure to resist axial compression. In contrast, the AF functions to maintain the NP within the disc epicenter and is comprised of concentric type I collagen fibers. LDH are classified based on their shape and are a result of displacement of the disc’s inner substance beyond the intervertebral boundaries. Herniations are categorized into three shapes: protrusion, extrusion, or sequestration ( Fig. 8.1 ). Protrusion occurs when the height of the hernia is less than the length of the base. Extrusion is when the height of the hernia exceeds the base and sequestration is when there is loss of continuity between the herniated material and the intervertebral disc. Correlating clinical presentation with radiographic findings is paramount, as LDH position will dictate the surgical approach.

Although the entire pathophysiological response to disc herniation can vary, it is accepted that neural structures surrounding the disc can become compressed and/or mechanically irritated with the resultant chemical inflammation invoking radicular pain and subsequent radiculopathy. Signs and symptoms of LDH include radicular pain, sensory abnormalities, and weakness in the distribution of one or more lumbosacral nerve roots. Focal weakness, restricted trunk flexion, and increased leg pain exacerbated by Valsalva maneuvers are reported. Additionally, increased pain when sitting, attributed to increased disc pressure, is reported.
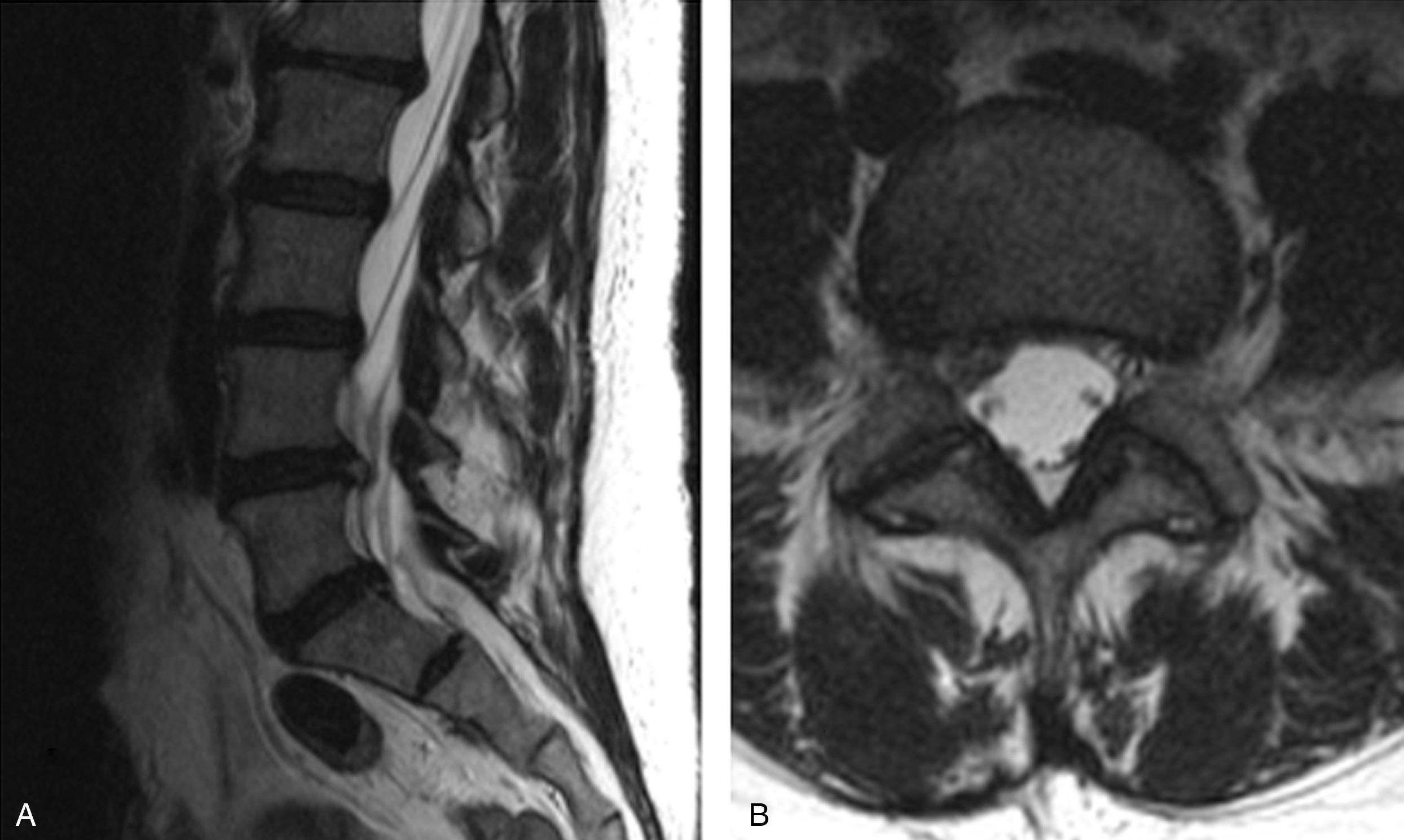
Physical examination including manual muscle testing, sensory testing, reflex testing, and supine straight leg resistance testing are key components for the clinical diagnosis of LDH. It is of paramount importance to correlate the clinical presentation with the radiographic findings. The affected dermatome is dependent on the spinal level of the herniation in addition to the herniation type ( Fig. 8.2 ). Paracentral disc herniations compress the traversing nerve root, whereas far lateral disc herniations affect the exiting nerve root. For instance, a paracentral disc herniation at L4–L5 causes on L5 radiculopathy, whereas a far lateral herniation at the same level results in an L4 radiculopathy ( Fig. 8.3 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here