Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In 1785 Hunter successfully ligated the popliteal artery of a coachman with a large popliteal aneurysm, relying on collateral circulation to maintain the viability of the limb. In 1916, while working at Johns Hopkins, Bertram Bernheim was the first to report the use of a saphenous vein interposition graft for treatment of a popliteal aneurysm. As a proponent of aneurysm ligation, Halsted did not support Bernheim’s work. Halsted presumed that interposition grafts would be at high risk of thrombosis, which would extend proximally and distally and interfere with natural collaterals. This work was not pursued and only some four decades later did Bernheim’s pioneering work finally enter mainstream clinical medicine as standard of care. Modern surgical treatment combines arterial bypass with ligation or interposition grafting and remains the gold standard for treatment. In addition, endovascular stent grafting has become an alternative treatment option in carefully selected patients. This chapter focuses only on the open surgical approaches.
Popliteal aneurysms may manifest as an asymptomatic pulsating mass behind the knee or with symptoms of either chronic or acute ischemia. A minority of patients experience pain or pressure behind the knee or with compressive symptoms involving the popliteal vein or peroneal nerve. Rupture is an unusual complication, occurring in 0% to 7% of published series with an average of about 2%. Acute limb ischemia is the most feared complication of popliteal aneurysms. Its occurrence can complicate treatment and is associated with significant risk of limb loss. In recent years the liberal use of thrombolytic therapy coupled with distal arterial reconstructive surgery has decreased the likelihood of major limb amputation with acute ischemia; however it remains a significant problem.
Any symptomatic popliteal aneurysm, regardless of size, should be repaired. In most series, however, only 60% to 70% of patients treated had symptoms at the time of presentation. For asymptomatic aneurysms, controversy remains regarding which need to be repaired or safely followed. For bypasses done to repair small, asymptomatic aneurysms, long-term graft patency and limb salvage is usually greater than 95%. Corresponding perioperative mortality with treatment is low, usually around 1% to 2%. Mortality rates can be three to four times higher in patients treated with critical limb ischemia. Aggressive recommendations for repair of asymptomatic aneurysms more than 2 cm in diameter have been proposed, especially in European centers, based on poor outcomes once thromboembolic complication occurs. Some reports have instead suggested that popliteal aneurysms smaller than 3 cm can be carefully watched. Mitigating features that further justify observation include the absence of intraluminal thrombus, normal runoff, and poor overall patient condition. Conversely, in good risk patients even small aneurysms with absent pulses suggesting occult embolization should be repaired, because 86% develop ischemic complications if left untreated. The advent of endovascular stent-graft treatment of popliteal aneurysms and better lytic therapy to improve runoff may also affect individual decision making.
An acceptable approach is to offer elective repair for all asymptomatic aneurysms that are 2.5 cm or greater unless the physician feels the risks of treatment are excessive because of the health status of the patient. For frail patients in poor health or with limited life expectancy the physician should observe even larger aneurysms provided that the estimated risk of complications is low, assuming minimal intraluminal thrombus, palpable distal pulses, and no evidence of continued expansion.
An ankle-brachial index, Doppler waveforms, and pulsed volume recordings or toe pressures are advisable to evaluate for silent distal embolization.
Computed tomography (CT) angiography ( Fig. 46-1 ) or magnetic resonance angiography can be used to determine the extent of the aneurysm and to select inflow and outflow targets for bypass in patients with no evidence of distal embolization on clinical or noninvasive testing. CT angiography, because of its ability to evaluate calcification, is complementary to angiography.
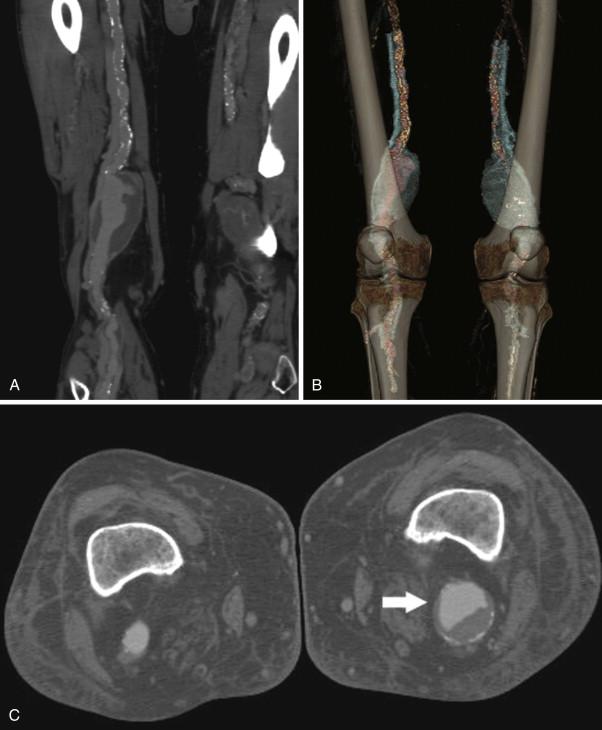
Arteriography remains important for evaluating outflow, especially when there is thrombosis or evidence of distal embolization. Angiography can be combined with preoperative lytic therapies in the setting of acute thrombosis without a suitable bypass target. In the elective evaluation of asymptomatic patients, high-quality CT angiography or magnetic resonance angiography may obviate the need for arteriography, especially with demonstrable normal runoff vessel anatomy.
Preoperative vein mapping, including great and small saphenous veins, should always be performed before popliteal aneurysm repair. Vein location should be marked on the skin and is used for planning the location of the incision. The small saphenous vein is rarely large enough to be a suitable conduit.
As with any peripheral bypass, low-dose aspirin should be initiated preoperatively and continued indefinitely.
Anticoagulation is not required for asymptomatic aneurysms but is advisable for evidence of embolization.
Clinical perioperative cardiac risk assessment is routine with selective use of noninvasive stress testing.
Screening for a contralateral popliteal artery aneurysm and for an aneurysm of the abdominal aorta should be performed. Bilateral popliteal aneurysms are present in approximately 50% of patients, and the combined incidence of aortic and popliteal aneurysm ranges from 40% to 70%.
Avoid excessive manipulation of aneurysms containing thrombus to minimize the risk of distal embolization.
Poor preoperative runoff may require bypass to a distal target artery at the ankle or on the foot. Vein conduit is mandatory for these procedures.
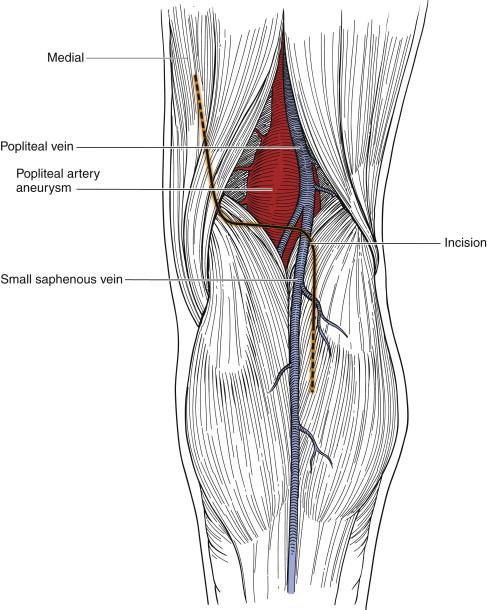
Posterior vertical incision across the popliteal fossa should be avoided. The lazy S -shaped incision ( Figs. 46-2 and 46-3 ) should be used, with the horizontal portion across the flexion crease to avoid wound dehiscence and contracture. Even when done well, the posterior approach is associated with local wound swelling and can be associated with significant incisional discomfort.

Ligation of the aneurysm should be performed proximally and distally, as close as possible to the aneurysmal sac. Jones and associates demonstrated that proximal ligature alone or ligating the inflow and outflow arteries remotely from the aneurysmal sac increases the likelihood of continued aneurysm expansion. Numerous studies have shown that even with proximal and distal ligation, as many as 30% of aneurysms do not thrombose and may continue to enlarge if collateral blood flow into the aneurysmal sac persists in a situation analogous to that of a type II endoleak with endovascular aneurysm repair. Continued expansion can result in pain, compression symptoms, and even rupture.
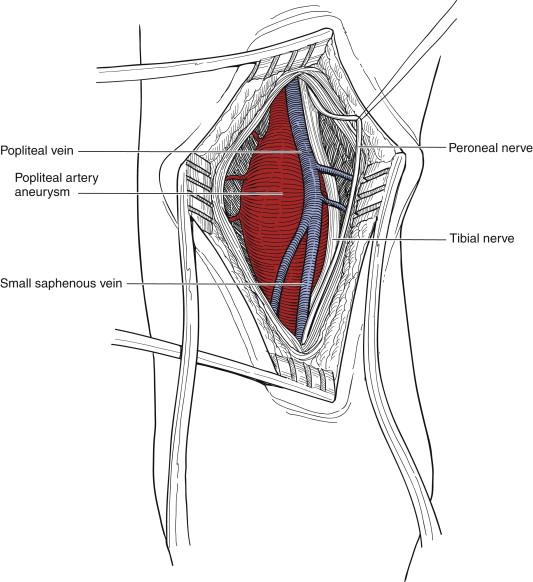
In patients with simultaneous aortic and popliteal aneurysms, treatment of the abdominal aneurysm may precipitate popliteal aneurysm thrombosis. In the posterior approach, care must be taken to avoid injury to the medial cutaneous sural, tibial, and peroneal nerves ( Fig. 46-4 ).
Compressive symptoms created by the aneurysm, such as leg edema, local pain, or weakness, require decompression of the aneurysmal sac.
Arterial exposure of the above- or below-knee popliteal artery can be difficult with large aneurysms or in the presence of arteriomegaly. Extensive kinking, tortuosity, and lateral displacement, especially of the distal popliteal artery, can occasionally make exposure and separation from the adjacent structures challenging.
Small or fusiform aneurysms are best approached medially by conventional bypass with aneurysm ligation. For large aneurysms limited to the popliteal fossa, especially with symptoms attributable to compression of adjacent structures, direct exposure from the posterior approach with interposition grafting from within the aneurysmal sac is preferable, unless the aneurysm extends too far proximally. The posterior approach is also advantageous to decompress an aneurysm that has continued to enlarge after bypass and ligation, because of backfilling from geniculate branches.
The medial approach is the preferred technique for most popliteal aneurysm repairs and the only logical option for bypass grafts that need to extend to distal tibial or pedal vessels. The medial approach has the advantages of being familiar to all vascular surgeons and providing easy access to the entire great saphenous vein. Virtually all of the procedure is performed some distance from the aneurysm, reducing the likelihood of operative injury to structures adherent to the surface popliteal aneurysm. The principal disadvantage of the medial approach is that access to the aneurysm is limited, making decompression of the sac difficult.
Vein conduit, as with peripheral bypasses performed for occlusive disease, is preferred for most reconstructions. Some surgeons prefer the routine use of prosthetic conduits for the posterior approach, because these posterior grafts are quite short, the diameter of the graft can be closely matched to the diameter of the popliteal artery, and their use avoids the complications of vein harvest. Excellent short-term results with prosthetic popliteal bypass have been reported, especially when good outflow exists.
The saphenous nerve must be protected in the medial approach to the above-knee popliteal artery as it exits the adductor hiatus and during harvest of the below-knee great saphenous vein.
The sural nerve is the terminal synthesis of the medial cutaneous sural nerve and cutaneous branches of the lateral sural nerve. In the lower calf, it is closely associated with the small saphenous vein.
The medial cutaneous sural nerve is located deep to the fascia and is the first nerve encountered in the posterior approach. It, like the tibial and peroneal nerves, is best retracted laterally in exposing the popliteal artery.
The tibial nerve is lateral and superficial within the popliteal fossa. It is large and easily identified. In distal posterior approaches a small branch to the medial gastrocnemius muscle may need to be sacrificed but is usually well tolerated by older patients.
The peroneal nerve is the lateralmost nerve in the popliteal fossa and is retracted laterally with the tibial nerve.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here