Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acknowledgment: We would like to acknowledge the contributions of Dean S. Louis, Mark Bagg, and Peter J. L. Jebson.
Traumatic injury is the most common cause of an amputated finger or thumb. In other cases, digital amputation may be necessary because of congenital deformity or acquired pathologic conditions, such as malignant tumors or chronic infection. Sequelae of trauma may also require amputation, such as stiffness, debilitating pain, or revision surgery to improve fit of a prosthesis. Functional recovery is the primary consideration after an amputation. For this reason, the surgeon should be aware of the patient’s occupation and vocations. The surgeon should express empathy and gauge the patient’s emotional response following the amputation. Failure to appreciate the patient’s attitude and ability to adjust to the injury may compromise an otherwise successful operative procedure.
As surgeons, we tend to be influenced by the experience of mentors early in our careers, and later, our own expanding experience. We hold fast to methods that prove satisfactory in our hands and quickly seek alternatives to procedures that yield unsatisfactory outcomes. The numerous articles referenced in this chapter attest to the reasoned contributions of many authors who treat similar amputation situations by disparate methods. For some surgeons, the more technically demanding procedures have great appeal. Other surgeons prefer the simplest yet most effective procedure, such as shortening of bone followed by primary closure, or healing by secondary intention. There is no gold standard technique for every clinical scenario.
The goals of amputation surgery in the upper extremity should be (1) preservation of functional length, (2) provision of durable skin coverage, (3) preservation of useful sensibility, (4) avoidance of symptomatic neuromas, (5) prevention of adjacent joint contractures, (6) prevention of morbidity by minimizing complications, (7) allowance of early prosthetic fitting when applicable, and (8) allowance of early return to work, play, and activities of daily living.
Any amputation in a child, whose ultimate role in life is yet undefined, should be approached with a conservative attitude. Later reconstruction is generally preferable to any early radical ablative procedure. Adults with well-defined functional roles may be better served by a more definitive approach that will accelerate their functional rehabilitation.
At times, deciding whether to perform limb salvage or amputation may be difficult. Consultation with an experienced and knowledgeable colleague is helpful and should be documented in the patient’s medical record. It may help reassure the patient and family. Photographs of the injured extremity before amputation are useful to document the severity of the injury. Although replantation or attempted salvage of a severely traumatized limb is an option at times, it may be more of a technical triumph than a procedure done in the patient’s best interests. The enthusiasm for the successful technical accomplishment of replanting an amputated finger part versus closure and early rehabilitation has been dampened by poor patient outcomes at a greater financial cost, including lost wages. Cold intolerance can be a substantial problem for patients following an amputation, but the symptoms tend to improve over time.
Maintain length.
Restore sensation.
Provide stable soft tissue coverage.
Prevent symptomatic neuromas.
Prevent adjacent joint contractures.
Allow early prosthetic fitting when applicable.
Allow early return to activities of daily living.
An amputation of the fingertip is the most common type of amputation seen in the upper extremity and at the same time provokes the greatest controversy because of the multitude of treatment options. Multiple techniques have been developed to advance local skin or transfer soft tissue to ensure coverage of an area where bone is exposed. The surgeon, in consultation with each patient, must choose the type of coverage that appears to be most appropriate for that individual’s needs and within the technical abilities of the surgeon. Regardless of choice of treatment, the goals of preserving functional length and restoring adequate sensibility remain constant. When one is comparing the various treatment options available or looking for guidance, the injury zone classification systems of Hirase, Allen, and Tamai provide a useful frame of reference ( Fig. 49.1 ).

When the fingertip is amputated, the geometry of the defect dictates the various treatment possibilities. The loss may be transverse or oblique, with more volar skin loss than dorsal skin loss, or the reverse may be true. Some slicing amputations may result in skin loss primarily from the ulnar or radial side of the digit and may spare the distal tip.
If the amputated part is available and not highly contaminated, it may be cleansed and reattached. This can be an effective approach in children with injuries distal to the distal interphalangeal (DIP) joint. The tip is reattached as a composite graft or defatted and sutured to the residual digit as a full-thickness skin graft ( Fig. 49.2 ). The concept of using it as a “biologic dressing” has been advocated by some; however, this is not often appropriate in adults due to the lack of success, and the concept of placing dead tissue into a contaminated field is flawed. If there is bony involvement of the composite graft, stability may be afforded by repair of the amputated tip with absorbable sutures, Kirschner wires, or a hypodermic needle. The nail plate is removed and the nail plate repaired. Timing of repair may be important. Moiemen and Elliot noted that those repaired within 5 hours after injury had a 61% survival rate compared with none after this time point. The tip may become necrotic but should be left in situ as long as there is no developing infection because the tissue acts as a biologic dressing. Butler and colleagues conducted a retrospective review of 120 patients under 16 years of age who underwent composite graft of digital tip injuries and noted 10% complete and 34% partial graft survival rate. Patients younger than the age of 4 years were likely to have complete graft survival. However, 48% of patients developed a hook nail deformity, 17% had cold intolerance, and 95% had some degree of functional limitations in the long term. Similar success has not been noted within adults. Heistein and Cook reported on 53 patients who underwent composite tissue grafting of injuries distal to the DIP joint. The success rate was 43% for injuries between the DIP joint and the eponychium and 58% for injuries distal to the eponychium. Factors linked to suboptimal results were smoking, age older than 18 years, alcohol use, presence of diabetes, and crush injury. In an effort to improve survival, Chen and colleagues reported on a technique whereby the distal amputated tip was defatted and deepithelialized and the bone excised in patients who sustained either a crush injury or a sharp transection injury. The survival rate was higher than 93% with an average two-point discrimination of 6.3 mm after 6 months. Over 90% of patients were happy with the cosmetic appearance and 86% were able to use the finger normally at work.
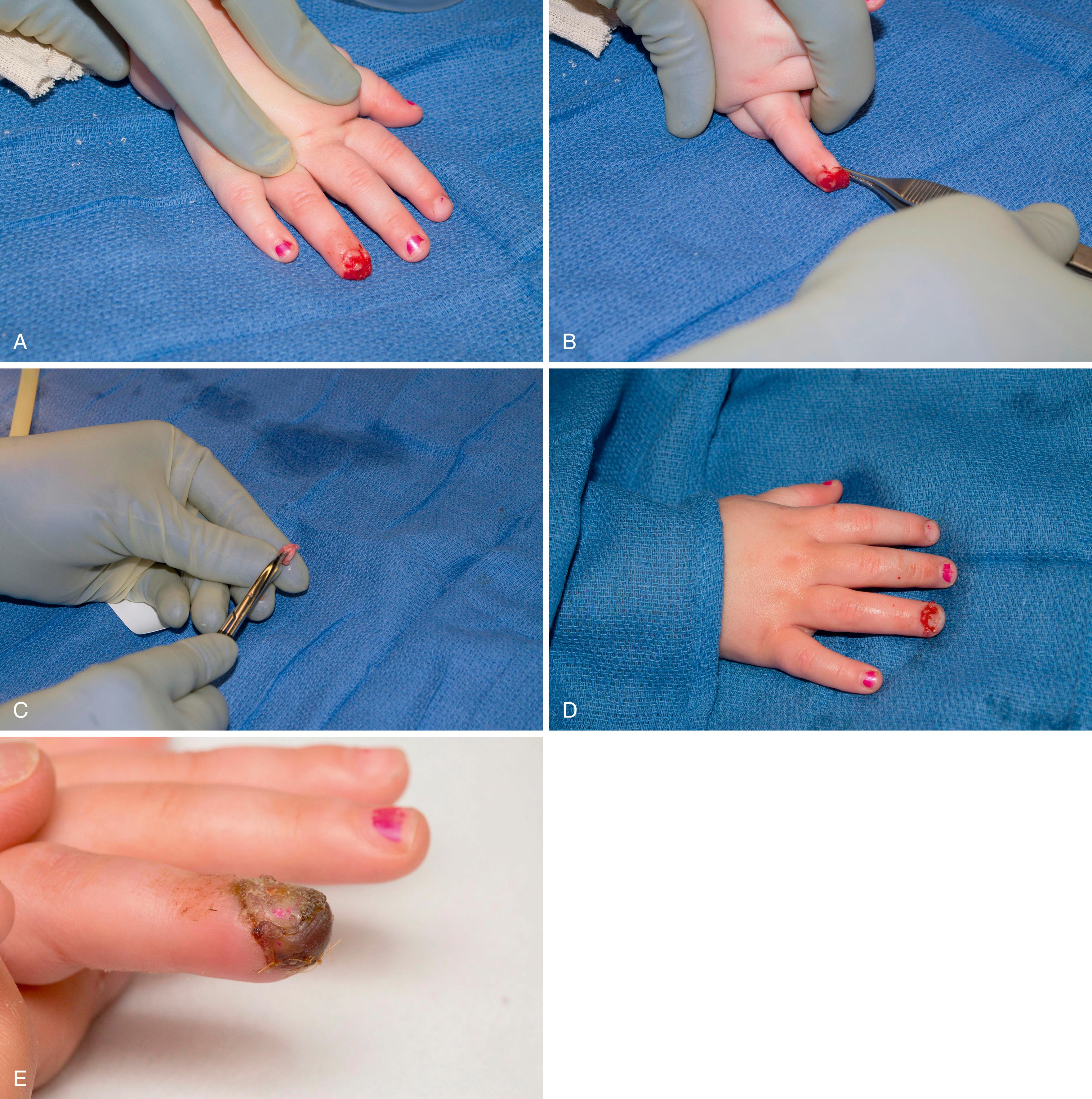
Healing by secondary intention with dressing changes is one of the best options for a tip amputation without exposed bone. This technique is especially applicable when the amputated part is unavailable or cannot be used. The technique is simple, inexpensive, and effective, regardless of patient age ( Fig. 49.3 ). , Healing by secondary intention is most applicable for wounds with skin loss of 1.5 cm or less; healing will occur by wound contracture and reepithelialization over 3 to 4 weeks with return of normal sensation and two-point discrimination. Indeed, recovery of sensation tends to be better than with other forms of surgical reconstruction. , Dressing changes can also be used to treat wounds with additional loss of subcutaneous tissue of similar size, but it may take 1 to 2 months to heal by this method. The patient performs daily dressing changes and local wound care. Protective splinting may be used to protect the healing wound. Patients can be referred to hand therapists within the first few days after injury to use modalities such as MIST ultrasound therapy (Celleration, Inc., Eden Prairie, MN) to encourage granulation tissue formation. Ultrasound works by reducing the bacterial load and promoting tissue regeneration by increasing angiogenesis, release of growth factors, and collagen deposition. Patients are encouraged to work on the range of motion to avoid joint stiffness and/or contractures.

Bojsen-Moller and colleagues reviewed a series of 134 digital tip injuries in 110 patients who were treated by dressing changes, shortening of the digit, or skin grafting. They observed that nonoperative treatment was uniformly compared with surgical cases that developed a variety of complications such as infection or graft failure that prolonged treatment. In addition, there was no significant difference in time off work between the treatment groups. The authors concluded that management of an amputation by skin grafting or dressing changes was superior to surgical shortening and primary closure. Allen reported on 46 patients with 49 fingertip injuries from the lunula and distal. If the distal phalanx was exposed, it was trimmed back to allow soft tissue to cover it. Forty-five patients felt their results were very good or good, 3 believed their outcome was acceptable, and 1 deemed the result as poor. Four of the 49 injuries required secondary surgery, 3 for nail growth problems and 1 because of lack of ample soft tissue coverage. The average two-point discrimination was 6 mm, and the average time off work ranged from 18 to 26 days. None of the patients had any joint stiffness, although 50% did experience cold intolerance that was marked in 10%. Weichman and colleagues compared the outcomes of patients with fingertip injuries treated nonoperatively with those treated operatively (nail removal, revision amputation, or grafting with full-thickness grafts or local flaps, such as the “V-Y” advancement, cross-finger, thenar, or first dorsal metacarpal flap). Those who had surgery had larger wounds (3.3 cm versus 1.75 cm), volar oblique lacerations (50% versus 9%), exposed bone (81% versus 35%), and a distal phalanx fracture (81% versus 47%). The authors found that patients requiring operative treatments required more time off work (4.3 weeks compared with 2.9 weeks), which was likely related to the extent of injury.
Primary closure may be performed if the repair is without tension across the wound edges. This can be difficult because there tends to be a lack of sufficient mobile dermis for a tension-free primary repair. Primary closure, when possible, was shown in the series by Holm and Zachariae to give results equivalent to conservative healing by secondary intention. However, in the series reported by Sturman and Duran, 51% of the patients complained of tenderness with some disability. Shortening of the bone may allow primary closure; however, the surgeon should perform traction neurectomies if the amputation is proximal enough to identify nerve branches to prevent a symptomatic neuroma. A nail bed ablation is performed if the injury is at or through the lunula. The entire germinal and sterile matrix is excised. This is performed by excising the tissue on the undersurface of the proximal nail fold as well as removing all nail matrix from the residual distal phalanx. Use of a curette to scrape the dorsal cortex of the distal phalanx is helpful. The patient should be informed of the potential risk of a symptomatic neuroma and a bothersome nail horn that can be present several months after the procedure.
Split-thickness skin grafting has been a popular method for coverage of the exposed pulp when there is a well-vascularized recipient bed. , Split-thickness grafts contract more than full-thickness grafts, and both are limited by the fact they cannot be placed directly onto bone or tendon devoid of its paratenon. In a study by Holm and Zachariae, only 56% of the patients who had undergone skin grafting considered their results to be good after 5 years of follow-up, compared with 90% of patients treated conservatively with a wound that was permitted to heal by secondary intention. The most notable complaints after skin grafting were induration and fissuring of the skin and reduced sensibility in the graft, as well as complaints about the donor site. Cold sensitivity was present in 39% of the patients treated conservatively and in 33% of those who received a split-thickness skin graft. Hypoesthesia was present in 26% of those treated conservatively and in 67% of those who were treated with a skin graft. The authors concluded that split-thickness skin grafting offered no advantages for fingertip coverage.
Sturman and Duran monitored 235 patients with a fingertip amputation for a minimum of 1 year and reported their late outcomes. Of the patients who had split-thickness skin grafts, 70% reported tenderness in the area of the graft, and in 41%, the tenderness was considered to be marked. Cold sensitivity was present in 49% of the patients who had split-thickness skin grafts, including 27 of the 53 who had thumb or index tip amputations. Fifty-nine percent of the latter group avoided the injured digit when the pickup test was administered. Thirty-two percent of patients noted diminished touch sensibility. The average two-point discrimination measured was 5 mm, considerably greater than the normal 2 mm.
When bone is exposed at the level of amputation, the question becomes whether length should be preserved (necessitating coverage of the site) or whether sacrifice of length is justifiable. However, small areas of well-vascularized bone may support healing if desiccation is prevented with appropriate wound care (such as with semiocclusive dressings or matrix bilayer dressings). For larger areas, flap coverage versus revision amputation via skeletal shortening and closure is the dilemma. An important variable is the extent of nail matrix injury and the possibility of developing a problematic hook nail deformity. The development of a hook nail is related to the wound closure and amount of bony support for the nail bed. Closure of a fingertip amputation by pulling the nail bed over the distal phalanx should be avoided. If a satisfactory amount of distal phalanx is absent, the nail bed should be trimmed back to the same level at the end of the bone so that it does not curve over the end of the bone and result in a hook nail. A nail bed ablation is performed if the injury is at or through the lunula. Since the primary aim is to expeditiously restore function, some wounds with minimal exposed bone are allowed to heal secondarily with appropriate dressing changes to avoid bone desiccation. Minimal skeletal shortening with a rasp or rongeur can allow adequate soft tissue coverage. Our suture preference is an absorbable suture to avoid the need for suture removal as the sutures become covered during the healing process and are painful to remove. Alternatively, the wound may be left to heal by secondary intention, ensuring that the nail bed is supported by underlying bone. Antibiotics are not routinely prescribed if there has been adequate wound debridement without gross contamination. Patients are seen within a week and are sent to occupational therapy to work on edema control and range of motion. Tip desensitization is started once the wound is healed and stable. Many of these injuries are work-related, and most manual workers are able to return to duty without restrictions by 6 to 8 weeks after injury. It is important to emphasize that skin-to-skin closure is not necessary. Flap coverage is reserved for cases with considerable bone exposure. There are a variety of described techniques that will be discussed, each with its own merits and limitations.
Studies have demonstrated successful treatment with the use of an occlusive dressing. , The dressing should be applied within a few days of the injury. Self-adhesive OpSite or Flexifix film (Smith and Nephew, London, UK) is used. The dressing is changed weekly until epithelialization has been completed. Hoigné and associates reported on a series of 17 patients with an exposed distal phalanx; patient satisfaction was good with regeneration of approximately 90% of the original soft tissue volume with an average two-point discrimination of 4 mm. The average duration of dressing use was 6.5 weeks. There were no cases of bone or soft tissue infection. Complications included a single case of a nail horn and neuroma formation.
The Integra Bilayer Matrix Wound Dressing (BMWD) (Integra Life Sciences, Plainsboro, NJ) is an acceptable alternative to flap coverage. The graft consists of an acellular dermal matrix composed of bovine collagen covered by a silicone layer. It is designed to act as a skin regeneration scaffold that allows the host’s cells to grow into the dermal template. It can be placed directly onto bone or tendon once the wound bed is clean and devoid of contamination. It can be sutured in place and its “take” encouraged with bolster dressings. The graft is normally applied as part of a two-stage procedure in which autologous skin graft is applied 3 to 4 weeks after matrix application. Taras and coworkers used two-stage grafting in digital injuries with exposed bone, joint, tendon, or hardware in 21 digits. The area of Integra application ranged from 1 to 12 cm 2 . Twenty of 21 digits demonstrated complete incorporation of the dermal matrix, and following skin grafting, 16 of 20 digits demonstrated complete incorporation. Single-stage use avoids the morbidity of skin grafting and is the same as healing by secondary intention because the healing process relies on both wound contraction and reepithelialization. In a series of 9 patients with an average defect of 2.3 cm 2 (range, 1 to 3.2 cm 2 ), Jacoby and colleagues demonstrated high patient satisfaction, with a mean static two-point discrimination of 9.6 mm (4.6 mm for the opposite unaffected finger). One patient developed an early infection, followed by a hook nail deformity 18 months after treatment. There were no other complications. The Integra BMWD is more expensive than a semiocclusive dressing or healing by secondary intention. However, the matrix may be placed directly on bone, preserving critical length and obviating the need for flap coverage with the associated inconvenience and morbidity ( Fig. 49.4 ).
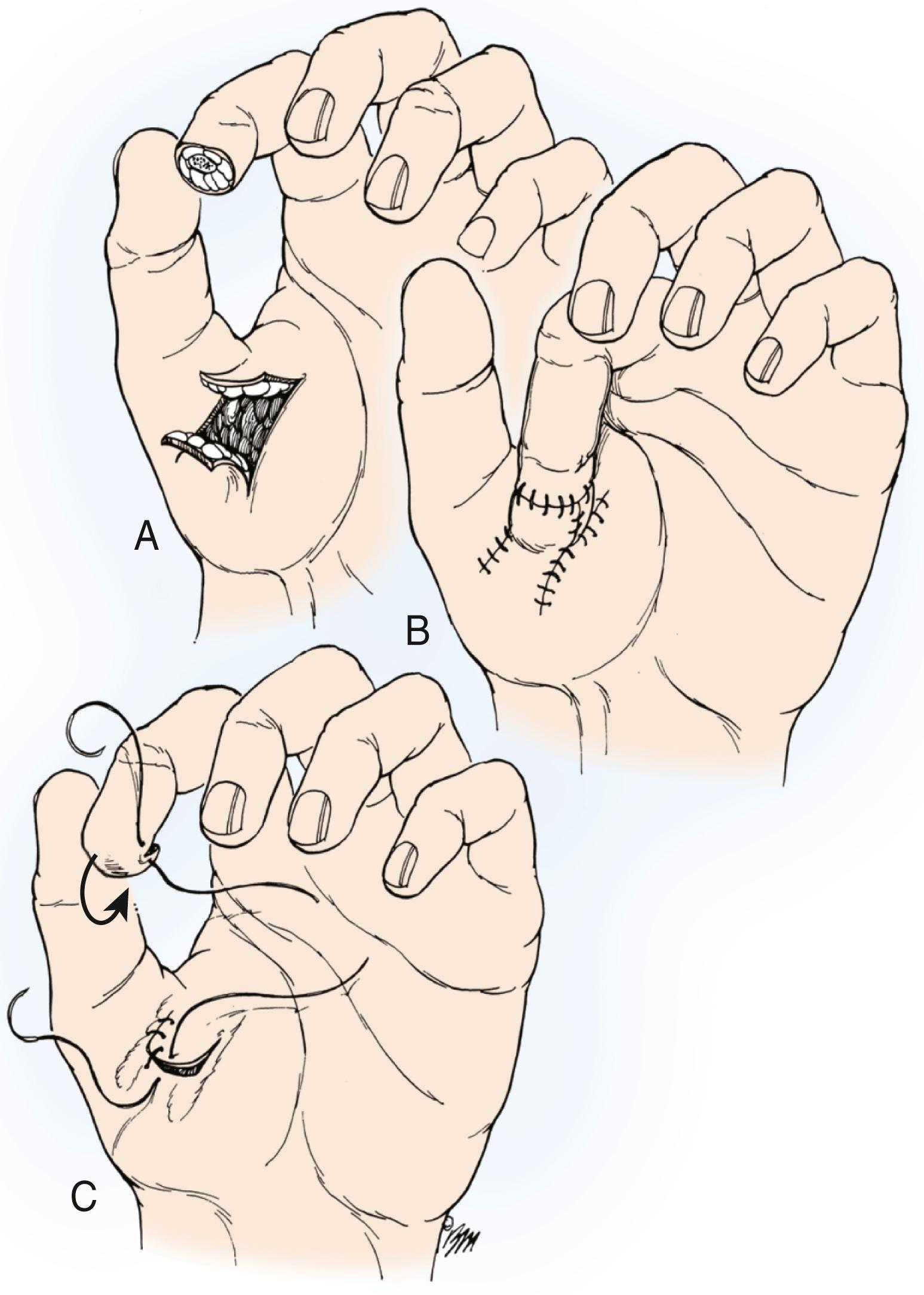
In 1970, Atasoy and associates described a triangular volar “V-Y” advancement flap ( Fig. 49.5 ) for reconstruction of the distal pad with preservation of length when bone is exposed. It is indicated for dorsal oblique or transverse distal fingertip amputations beyond the midpart of the nail. The flap is contraindicated in oblique amputation injuries with more palmar skin loss than dorsal skin loss and injuries with extensive skin loss.
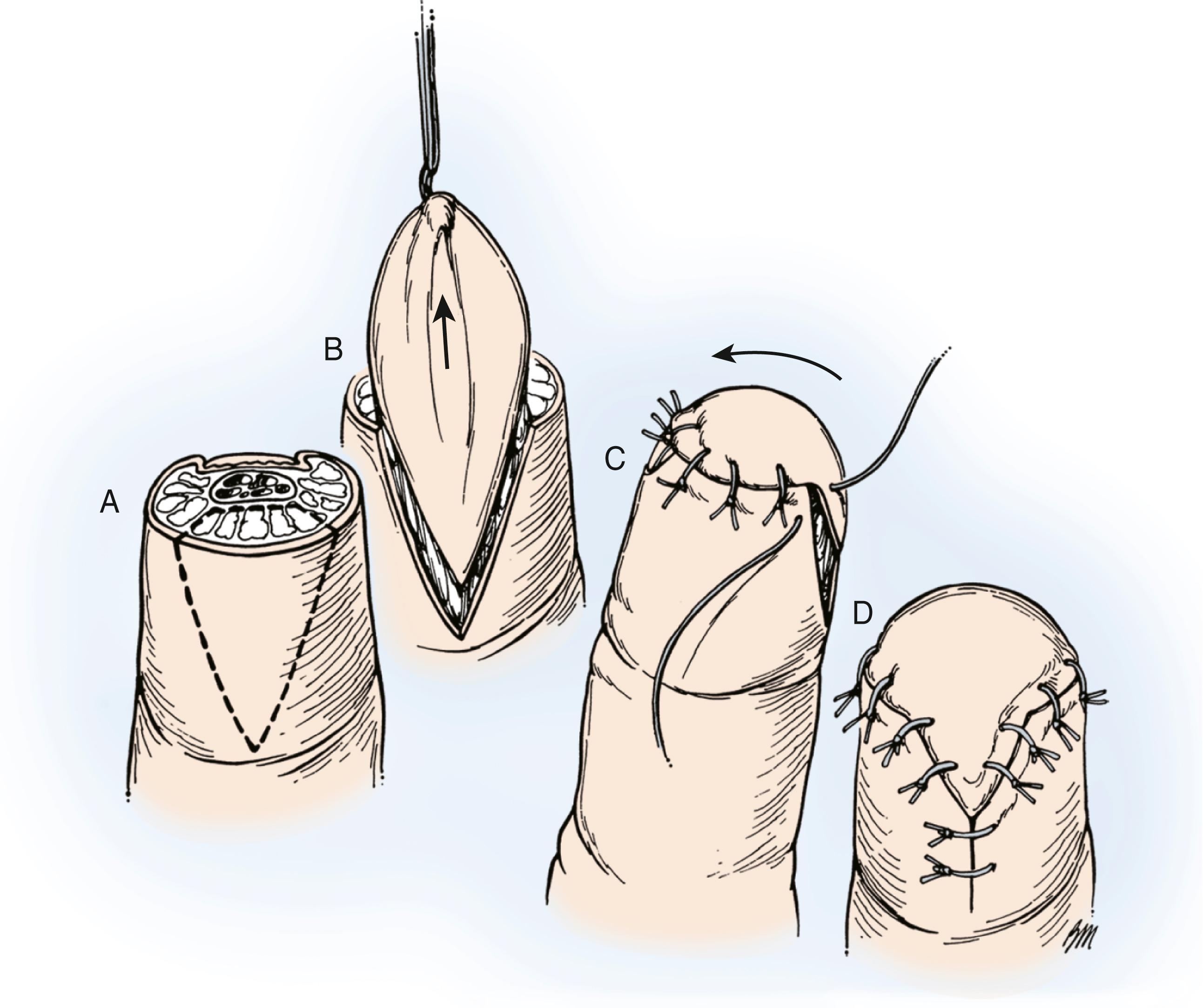
Digital anesthesia is administered before preparation of the wound. After surgical preparation of the hand, a Tourni-Cot (Mar-Med, Grand Rapids, MI) is used to exsanguinate the digit and simultaneously provide tourniquet ischemia. Alternatively, the finger is elevated and a Penrose drain secured at the base of the digit. A pattern may be made to cover the dimensions of the defect and then transposed proximally to the cut edge of the skin that is to be advanced. The base of the triangle will be the distal cut edge, and an appropriate triangle of skin is made according to the pattern, with the apex of the triangle being at the DIP flexion crease. The two sides of the triangle should be at least 1.5 times the length of the desired advancement. Only the full thickness of the skin is cut. The digital nerves and blood vessels of the flap are preserved. Its blood supply is presumed to be axial from proximal small arterial branches of the distal digital arteries. Separation between the flexor sheath and subcutaneous tissue is performed by dividing the fibrous septae that anchor the subcutaneous tissue to the bone, which facilitates advancement of the flap distally. The skin of the flap must be connected to the subcutaneous tissue to maintain its viability. The base of the triangle is carefully contoured and sutured to the nail bed or remaining nail, and the resulting “V” incision on the palmar aspect of the digit is closed, thus converting it to a “Y” (see Fig. 49.5 ). The Tourni-Cot or Penrose drain is removed prior to flap insetting to assess viability. The flap can be adequately mobilized up to 1 cm and if necessary, defatted to facilitate tension-free skin closure. Postoperative management consists of sterile dressings that allow early motion of all adjacent joints, especially the proximal interphalangeal (PIP) joint. Active motion and digital usage are advanced as healing ensues over the next few weeks.
In their initial report, Atasoy and associates stated that 56 of 61 patients available for follow-up had normal sensation and motion. However, a follow-up study conducted by Frandsen found hypoesthesia or dysesthesia in 7 of 10 patients with triangular volar flaps. Four of the 10 patients had subjective complaints of cold intolerance, and 5 of the patients also had difficulty grasping objects. Conolly and Goulston had suboptimal results in 4 of 7 patients treated by this technique. The results were deemed unsatisfactory because of persistent paresthesias or impaired sensibility. Tupper and Miller reported diminished sensibility in all 16 of their patients. Eight of their patients reported hypersensitivity, particularly cold intolerance.
Kutler described the use of “V-Y” advancement flaps for digital tip injuries ( Fig. 49.6 ). The technique involves advancing two triangular flaps from lateral positions to cover the tip of the digit.
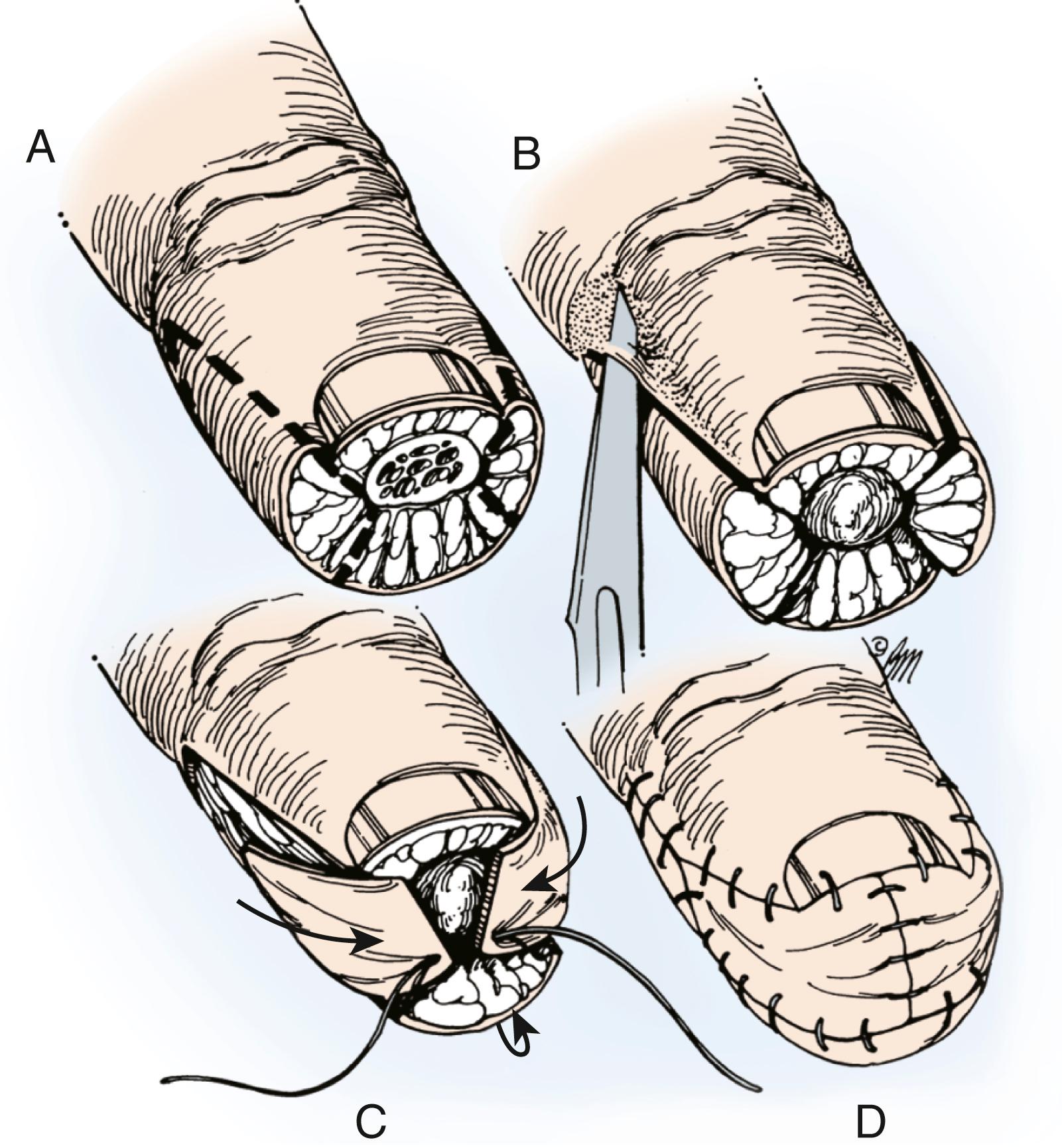
Preparation of the digit is similar to that used in the Atasoy technique. The tip of the digit is debrided as necessary. Two triangular flaps are developed from the midlateral aspect of each side of the digit, and the incisions are made just down through the dermis. The subcutaneous tissue is similarly mobilized from the phalanx on a deep plane by dividing the fibrous septae. Both triangles are advanced to the midline distally and sutured together. The “V” apex of the triangle is closed in a “Y” fashion, and the surrounding edges and nail bed, or nail, are carefully sutured to the distal edges of the advanced flaps (see Fig. 49.6 ). This flap can only be advanced up to 3 to 4 mm. Haddad reported on a series of 20 patients treated with this technique and stated that slight skin necrosis occurred at the edges if the flaps were too large. Subjective evaluation in a series of 22 patients was reported by Freiberg and Manktelow, who noted mild hypersensitivity and numbness in 7 of 22 patients. Frandsen reported a follow-up study of 14 patients who underwent Kutler’s technique and found subjective complaints of coldness in 8 patients (57%), tenderness on percussion in 10 (71%), difficulty in grasping small objects in 6 (43%), and slight hypoesthesia or dysesthesia in 10 (71%) when objectively measured. Patients also reported an average time off work of 61 days.
Shepard reported excellent results with a modification of Kutler’s technique in 28 traumatic amputations and 9 reconstructive procedures by dividing the dorsal pedicle and advancing the flap 10 to 14 mm. The nerves, vessels, and subcutaneous tissues are preserved under the palmar skin incision. The dorsal incision is made down to bone and the fibrous septa divided. On the palmar side, the skin is incised only and the flap advanced distally. Shepard suggested that the Kutler technique is most applicable to oblique palmar and transversely oriented amputations.
Given the limited advancement of the Kutler lateral “V-Y” flaps, others have described modifications by either raising the triangular flap on its neurovascular pedicle or extending the flap to the PIP joint crease to increase its size and ability to advance distally. , The flap could be advanced up to 2 cm, although patients were at risk of cold intolerance (49%), numbness (78%), PIP joint flexion contractures (17%), and DIP joint flexion contractures (22%). These “V-Y” advancement flaps are at risk of necrosis if tension-free closure is not achieved. The tension placed on them at closure could cause a hook nail deformity as it pulls the nail bed palmarly and could also diminish sensation due to tension on the digital nerves. These problems can be overcome by allowing the proximal wound to heal by secondary intention.
Moberg is credited with the technique of volar flap advancement for coverage of thumb tip amputations. The flap is a bipedicled, axial-pattern, cutaneous advancement flap. Snow advocated the technique for fingertip amputations when length is to be maintained. Advancing volar skin on its neurovascular pedicle provides the dermis with sensibility without losing length. Arons has modified this with the addition of a terminal dermal graft for padding, and sometimes a skin graft may be added at the base of the digit to gain length.
Regional anesthesia is obtained, the limb is exsanguinated with an Esmarch bandage, and a pneumatic tourniquet is inflated. The distal tip is appropriately debrided, and midaxial incisions just dorsal to the flexion crease at each of the interphalangeal (IP) joints are made on both sides of the digit. The flap is completely separated from the underlying flexor tendon sheath, advanced to the distal tip, and sutured to the nail bed and the adjacent sides of the digit. The tip of the flap may need to be shaped to fit the distal defect.
This method is only appropriate for the thumb ( Fig. 49.7 ) as the fingers lack the robust dorsal circulation compared with the thumb and the thumb is able to tolerate a mild IP flexion contracture without substantial morbidity. Flap advancement is limited to wounds measuring 1 cm in longitudinal dimension. Reported complications are fixed flexion deformity of the IP joints and skin necrosis on the dorsum of the finger. The studies of Caplan and coworkers, Leffert and associates, and Armenta and Lehrman suggest that the blood supply to the flexor tendon apparatus is compromised using this flap. Reports of tendon nutritional complications, however, are lacking.
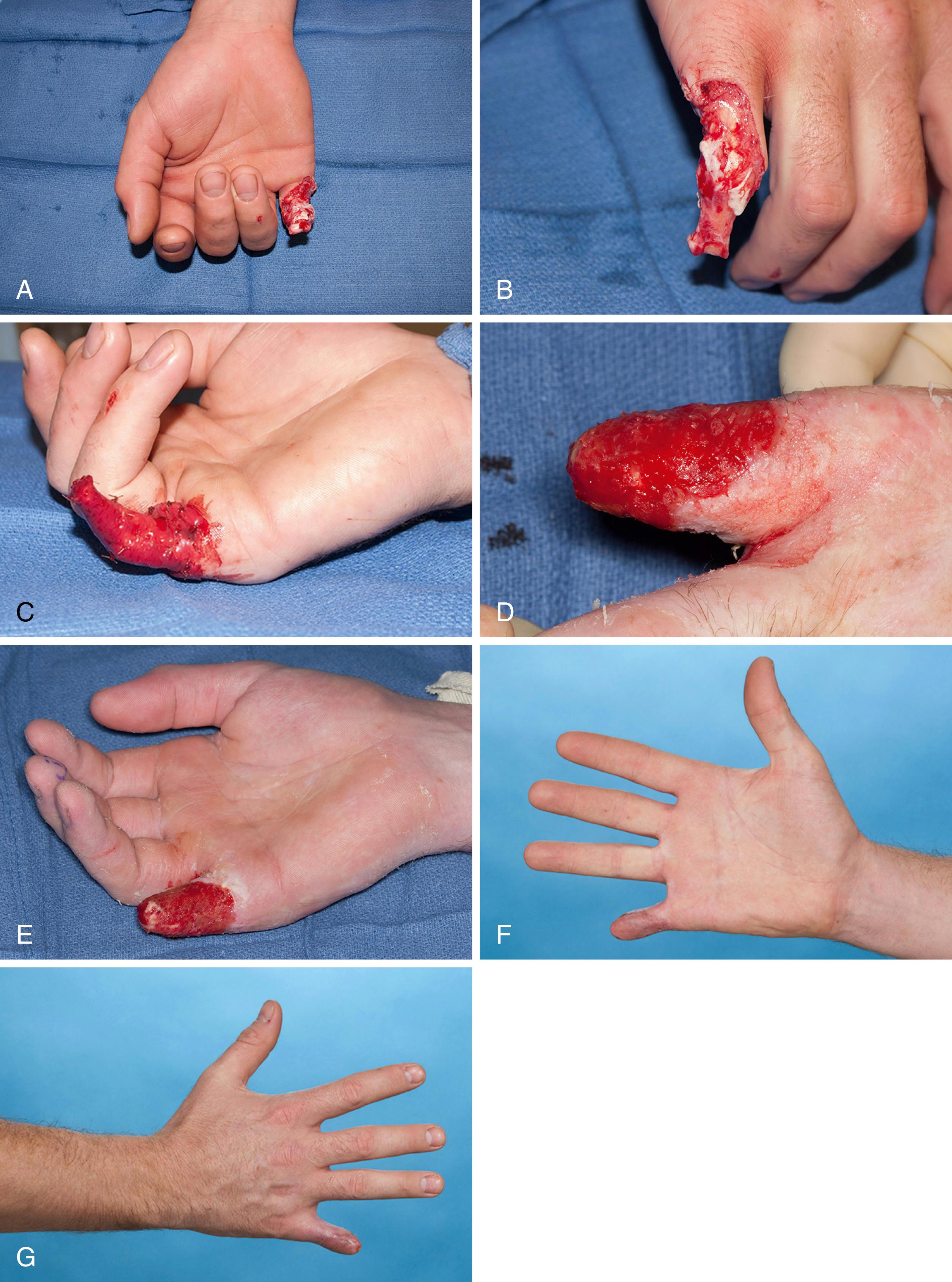
The cross-finger pedicle flap technique, first described by Gurdin and Pangman in 1950, is indicated when other techniques for local flap coverage are not possible and maintenance of length is important. Examples include distal amputations of the index finger or thumb and amputations of multiple digits where remaining length is critical ( Fig. 49.8 ). The flap, however, is associated with stiffness and is considered contraindicated in patients with preexisting arthritis or in patients over the age of 50 years. Paterson noted an increased incidence of stiffness in patients older than 41 years.
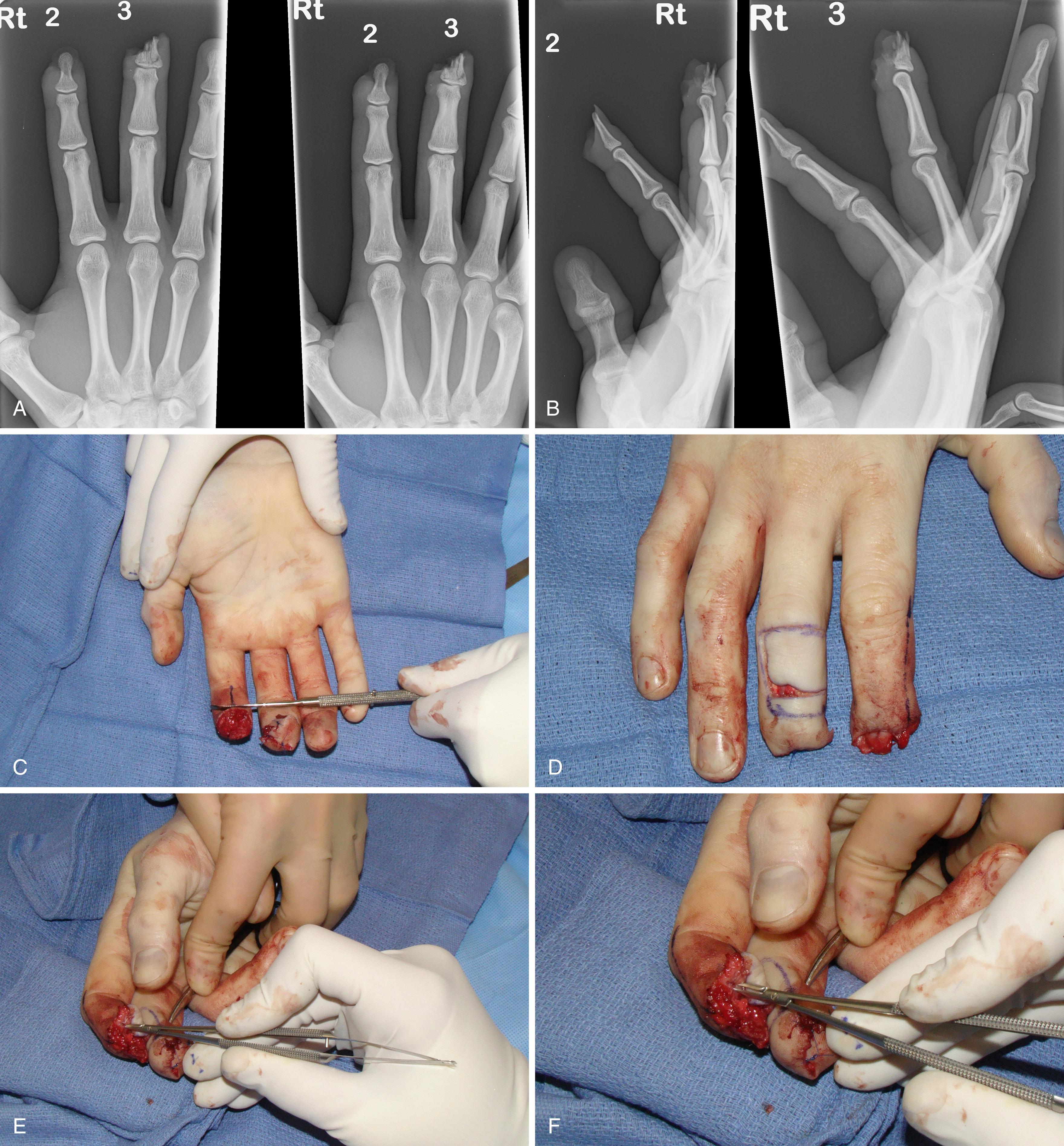
The flap provides coverage for an oblique volar defect of the pulp region or for extensive soft tissue loss on the volar fingertip with exposed bone and tendon (see Fig. 49.8 ). A piece of an Esmarch bandage is used to template the defect and to design the flap. It is important to measure the defect or make a template rather than estimate the flap size. We will make the flap 1 to 2 mm larger than the defect to allow for tissue contracture and ensure tension-free insetting of the flap.
The donor site is outlined with a marking pen on the dorsum of the neighboring digit. The broad pedicle will be on the side adjacent the digit with the wound. With careful tissue handling, the flap is reflected with preservation of its venous drainage at the base of the flap. The dissection is carried down to the plane between the paratenon of the extensor mechanism and the subcutaneous fat. The dissection should not violate the paratenon to preserve a viable bed for skin grafting of the donor site. The three margins of the flap are sutured in place on the recipient site. The fourth margin is to be sutured at the time of flap detachment. A full-thickness skin graft from the ipsilateral upper extremity (i.e., hypothenar, antecubital, or medial forearm skin) is used to cover the defect on the extensor surface of the donor digit. Skin without hair is used to prevent later hair growth on the donor digit. To avoid undue tension on the vascular pedicle of the flap, the two fingers may be sewn together or a transdigital Kirschner wire can be placed. A bulky soft dressing reinforced with a plaster splint is applied. At 3 weeks postoperatively, there should be sufficient circulation from the recipient wound bed to the flap. However, if there is concern about division of the flap, a Penrose drain can be placed around the base of the donor digit to assess flap perfusion from the recipient finger. If adequate, the flap is detached and inset into the recipient site. Cohen and Cronin modified the technique to include a dorsal sensory branch of the digital nerve that is coapted to the recipient digital nerve at the time of flap division. They reported an average two-point discrimination of 4.8 mm in 88% of the patients in their series. The nerve can also be coapted at the time of flap coverage to provide sensation in the flap, which is our preference (see Fig. 49.8 ).
After detachment of the flap, motion of the digits is encouraged to mobilize all the adjacent joints. Follow-up studies by Sturman and Duran, Kleinert and associates, and Johnson and Iverson have indicated that the return of sensibility to cross-finger flaps as measured by two-point discrimination tests showed excellent flap reinnervation that demonstrated progressive improvement over time. Lassner and colleagues reported an average two-point sensibility of 3.6 mm and cold intolerance in 6 of their 15 patients using a bilaterally innervated sensory flap.
In 1926, Gatewood described the technique of a thenar flap for coverage of digital tip injuries with exposed bone. This was subsequently expanded on by Flatt in 1957 and modified by Smith and Albin with a technique that they describe as a thenar “H”-flap.
The indications for the random-pattern thenar flap are similar to those for a cross-finger flap, namely, when preservation of length is important and other techniques are not applicable. The flap has been advocated for use in the index and long fingers only and in younger patients without any preexisting arthritis or joint injury. The proposed advantages are (1) better skin color and texture match, (2) abundance of subcutaneous tissues, and (3) return of some sensibility. To avoid permanent joint stiffness or unsightly scarring in the donor area, one must keep in mind the three cardinal technical principles outlined by Melone and colleagues : (1) Design the flap near the metacarpophalangeal (MCP) crease of the thumb and avoid the midpalmar area, (2) fully flex the MCP joint with whatever amount of flexion is required in the IP joints of the recipient finger, and (3) detach the pedicle 10 to 14 days postoperatively and begin immediate active range-of-motion exercises.
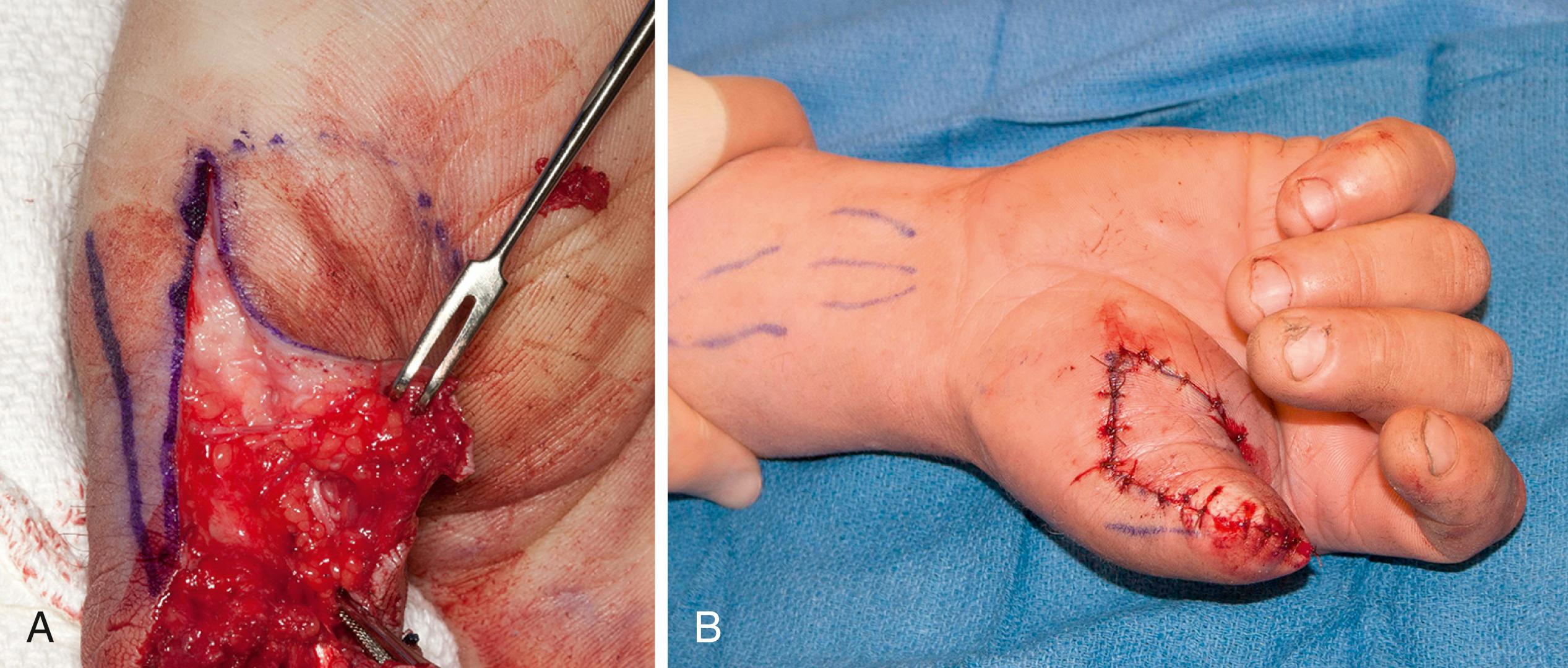
Fig. 49.9 shows the thenar “H”-flap as described by Smith and Albin. The area of contact of the injured digital tip with the thenar eminence is outlined. An “H” is drawn on the skin approximately 20% wider than the defect. The transverse limb of the incision is made at the most distal contact point of the fingertip with the thenar eminence (see Fig. 49.9 A). Square proximal and distal flaps are elevated, including the subcutaneous tissue. The proximal flap is sutured to the fingertip, and the distal flap is sutured to the proximal margin of the defect on the volar side of the injured finger (see Fig. 49.9 B). The proximal flap is advanced distally and the distal flap advanced proximally to close the donor defect. A soft dressing is applied, and 2 weeks later the flap is detached. The fingertip is closed with the proximal flap, and the distal flap is advanced into the thenar defect (see Fig. 49.9 C). This closes the donor site primarily and avoids the potential problem of an unsightly scar in the thenar eminence.
An alternative technique is to elevate a proximally based flap and suture it to the injured tip similar to that just described but to use a full-thickness or split-thickness skin graft or Limberg-type flap for the thenar defect when the flap is divided and inset. ,
Satisfactory outcomes with the thenar flap have been reported in several clinical series. Porter compared the results of 56 pedicle flaps with 44 free grafts. He found sensibility was better in cross-finger and thenar flaps and that these flaps resulted in excellent cosmesis. Porter also concluded that full-thickness grafts were superior to split-thickness skin grafts. In terms of subjective and objective sensibility evaluation, of the five methods evaluated in his study, the results were superior with the thenar and cross-finger flaps. Thanik et al. used a combination of the thenar flap in combination with a bone and split thickness nail bed grafts to reconstruct bony, soft tissue, and nail bed injuries and reported the functional and cosmetic results in over 50 patients. Flexion contracture is a particular concern with the thenar flap as the IP joints of the finger must be flexed to a greater degree during the period of flap “take” than the other options discussed in this chapter.
A number of elegant and ingeniously conceived island flaps have been described for coverage of fingertip amputations. These consist of flaps raised on their neurovascular pedicle, and advantages include avoiding prolonged digital immobilization, single-stage reconstruction permitting early rehabilitation, adding an independent blood supply to provide a good soft tissue bed for nerve grafting or repair, restoring a well-padded sensate digital pulp, offering the potential for a composite tissue transfer via wide selection of donor sites, and allowing a greater arc of rotation over longer distances. These include homodigital and heterodigital island flaps and can be anterogradely or retrogradely based. , However, island flaps are more technically demanding and are associated with complications such as flap failure, joint contracture, and cold intolerance. However, the degree of joint contracture and stiffness is less than the other procedures as these flaps do not require immobilization of the digit in a flexed position. In addition, the homodigital flaps eliminate the morbidity of the neighboring digits. Therefore the use of these island flaps may offer decreased morbidity and improved outcomes in select cases. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here